Download It - Onstream Media
Download It - Onstream Media
Download It - Onstream Media
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
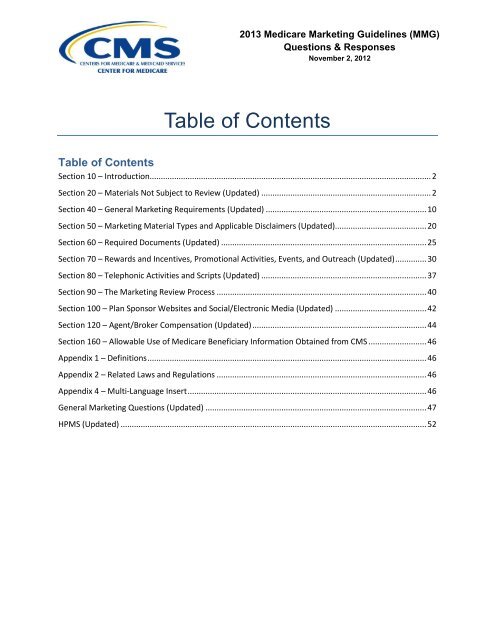
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Table of ContentsTable of ContentsSection 10 – Introduction.............................................................................................................................. 2Section 20 – Materials Not Subject to Review (Updated) ............................................................................ 2Section 40 – General Marketing Requirements (Updated) ........................................................................ 10Section 50 – Marketing Material Types and Applicable Disclaimers (Updated)......................................... 20Section 60 – Required Documents (Updated) ............................................................................................ 25Section 70 – Rewards and Incentives, Promotional Activities, Events, and Outreach (Updated) .............. 30Section 80 – Telephonic Activities and Scripts (Updated) .......................................................................... 37Section 90 – The Marketing Review Process .............................................................................................. 40Section 100 – Plan Sponsor Websites and Social/Electronic <strong>Media</strong> (Updated) ......................................... 42Section 120 – Agent/Broker Compensation (Updated) .............................................................................. 44Section 160 – Allowable Use of Medicare Beneficiary Information Obtained from CMS .......................... 46Appendix 1 – Definitions ............................................................................................................................. 46Appendix 2 – Related Laws and Regulations .............................................................................................. 46Appendix 4 – Multi-Language Insert ........................................................................................................... 46General Marketing Questions (Updated) ................................................................................................... 47HPMS (Updated) ......................................................................................................................................... 52
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 20 – Materials Not Subject to Review (UpdatedNumber Question Response4. General health promotion materials that do notinclude plan specific information are exempt fromreview. Would materials promoting preventiveservices covered under Original Medicare at zerocost sharing and therefore covered under our planat zero cost sharing fall under this exemption if thematerial includes reference to the “zero costsharing” element or does that make it plan specificsuch that it would be subject to submission andreview?Plan materials promotingpreventive services covered at zerocost sharing are exempt fromreview.5. What are examples of ad-hoc enrolleecommunication materials?6. Ad hoc enrollees - if you are changing your billingformat and sending a notice to all members - isthat still considered ad hoc as it is going to allmembers and not a subset?7. Section 20 of the MMG states that ad hoc enrolleecommunications are not required to be submittedto CMS for review. If we send out a flyerpromoting health fairs and then include a note thatthese are services provided w/ no co-pay can thisstill be considered an ad hoc piece?8. New - For Materials not subject to Review areSponsors still expected to display the ContractNumber on the material?9. New - <strong>It</strong> was indicated no unique Material IDrequired for Materials Not Subject to Review. <strong>It</strong>hought a Material ID was needed on all materials,regardless if they are submitted to CMS orreviewed internally.See appendix 1 of the MMG for adefinition and examples of ad hocenrollee communications.As each situation is different andunique, plans should consult theirAccount Manager for assistance indetermining whether a materialwould qualify as ad hoc.If the piece contains benefitinformation, it generally is nolonger ad hoc. Questions shouldbe referred to your MarketingReviewer or Account Manager.Materials not subject to CMSreview would not have a materialID.Material IDs are required formaterials that must be uploadedinto HPMS. Materials that are notsubject to review should not beuploaded into HPMS and thereforedo not require a material id.The Final Contract Year 2013 Medicare Marketing Guidelines 3
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question8. Can a plan put their logo or name on themulti-language insert?9. Per §30.7.1 – Multi-Language Insert of thenew Medicare Marketing Guidelines, theMulti-Language Insert must accompanythe Summary of Benefits and theANOC/EOC. Must plans include the Multi-Language Insert when sending a membera stand-alone EOC (i.e., when no ANOC isrequired)?10. In regards to Member Referral Programs(30.11): Can the member‟s name beprovided to the potential enrollee? Orshould the referring member remainanonymous at all times?11. In section 30.3 there are NCQA guidelinesfor SNPs, but is there guidance for non-SNP plans regarding NCQA?12. If we create advertising campaigns withmaterials targeting women only or menonly, is this considered discriminatorymarketing?13. Is the guidance for provider owned HealthPlans the same as the guidance for cobrandingcontained in 30.2.1 & 50.9?14. Can a general statement be made inmarketing materials such as “not happywith the poor star rating, enroll with our 5star plan” or would that be in conflict withsection 30.12.1?ResponseYes.Yes - If the individual is a new memberreceiving a standalone EOC as part of theirrequired materials at the time of enrollment,No- If the individual is an existing memberreceiving a standalone EOC because theplan separated the ANOC from the EOC(where allowed) and the member receivedthe insert with the ANOC.Plans can make this determination bycontacting the referring member.The NCQA approval process for the modelof care applies only to SNPs. Therefore,the disclaimer is not applicable to non-SNPplans.Plan sponsors may highlight benefits thatwould appeal to differing demographicgroups in advertising materials, but may nottarget those groups specifically. Forexample, a sponsor may promote breastcancer awareness by creating materialsthat highlight plan services to helpbeneficiaries prevent or manage thedisease, but these materials could not bedistributed to only women. They wouldhave to be distributed to any beneficiary.The MMG defines co-branding as arelationship between two or more separatelegal entities, one of which is anorganization that sponsors a Medicare plan.When a provider organization sponsors aMedicare plan, the co-branding rules do notnormally apply unless the entity that issponsoring the Medicare plan is a separatelegal entity from the other entities under theprovider organization‟s umbrella.Plan sponsors should refrain from makingnegative statements about lower performingplans when highlighting their 5-star rating.The Final Contract Year 2013 Medicare Marketing Guidelines 5
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question15. For non-English speaking membersreceiving translated materials identified in§§30.8, 30.9 and 30.12, are we required toprovide them with translated versions ofother member materials, e.g., enrollmentletters, claims letters, G & A letters, etc.?ResponsePlans are encouraged to make thesematerials available upon request.16. If we translate materials into languagesother than Spanish, is it permissible to usethe English version, or must we also havethe Program Mark translated into thoselanguages?17. When filing Alternate Format, what dateshould go on the piece after filing? Do westill use the date of the English approval?18. When will CMS release the new modelenrollment form?19. What if a plan is brand new and has nostar rating. Do they still need to informbeneficiaries of this in the Summary ofBenefits?20. Does the plan ratings document need tobe filed with CMS?21. Should the plan ratings document be in theEnrollment Form?22. If a plan offers just a PDP plan, can itrevise the multi-language insert to removethe reference to health"?23. The multi-language insert - do we have tolist all of the languages? What if we havevery few persons in our city who are of thatlanguage?The Program Mark is proprietary and maynot be altered.The date is not required on marketingmaterials. Plan sponsors should file thealternative format once the English versionhas been approved in HPMS.The 2013 Enrollment guidance wasreleased in HPMS on August 7, 2012,Revisions to Medicare Advantage andPrescription Drug Plan.No.Yes the plan ratings document should befiled under code 1090.The plan ratings document should beprovided with an enrollment form.The multi-language insert is a standardizeddocument that should not be modifiedexcept as allowed by the instructions. Theword "or" was specifically used to accountfor both MAPDs and PDPs, and anychanges would require changing all 15languages.Yes.The Final Contract Year 2013 Medicare Marketing Guidelines 6
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question24. Are plans allowed to use a plan logowithout a standard plan type when thematerial is sent to enrollees of all producttypes?ResponseIf the logo is generic enough to properlyidentify the plan, it would be OK.25. Regarding Multi-language insert, if we areutilizing the template by only addingtelephone numbers, does it need to befiled for approval? File and Use? Or wecan use as is? If we need to add additionallanguage translations, does it need to befiled? What is the filing process?26. This was asked during the draft commentperiod, but the Multi-Language insert stillhas Arabic and Hindi missing, and somelanguages do not download properly. Isthis being addressed?27. Multi-Language Insert - will this berequired more than once if all material isbound into a book?28. Does using a window envelop that showsthe plan logo through the window, satisfythe requirement to show the logo on theenvelope?29. How does the Required Materialsrequirement apply to a telephonicenrollment situation?30. Are new members required to receive theANOC/EOC or just the EOC?The Multi-Language insert should besubmitted in HPMS using the 4036 code. <strong>It</strong>is a standardized document that should notbe modified except as allowed by theinstructions.The word document included on ourwebsite contains the Arabic and Hindilanguages.Plans must include the Multi-LanguageInsert with the Summary of Benefits and theANOC/EOC. D-SNPs that choose to mailthe ANOC and EOC at different times arerequired to send the Multi-Language Insertin the first mailing and have the option toinclude in the second mailing.Section 50.6 states the plan name or logomust be either on the front envelope or onthe mailing, when no envelopeaccompanies the mailing. Plans shouldalso refer to Appendix 2 of the MMG,Mailing Standards.Regardless of the enrollment mechanism,the materials listed in Section 30.9 of theMMG must be provided to all new enrolleeswithin CMS' required timeframes.Beneficiaries who enroll with your plan mustreceive an EOC. The ANOC is not requiredfor new members.The Final Contract Year 2013 Medicare Marketing Guidelines 7
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question31. Are the summary of benefits, star ratingsinsert, and multi-language insert requiredto be sent with the plan change form (orshort application)?ResponseYes, a plan change form is an enrollmentform.32. If a new member is enrolled in our plan onJuly 1st 2012, do we have to send them anANOC that states the changes from 2011to 2012?33. Is Part D EOB required in non-Englishlanguage for plan sponsors operating inareas where the five (5) percent languagerequirement threshold is met?34. Can you please review what is requiredwith the enrollment form? Confused as tothe wording in 30.9 stating thatdirectories/formularies are required at timeof enrollment. Also we used to have toprovide Grievance and Appeals with theenrollment. Is this no longer required?35. Can one set of pre-enrollment documents(like the SB) be sent to a multi-personhousehold? What about enrollmentapplications? Does this apply to individualand group pre-enrollment?36. Do Employer/Union group pre-enrollmentmaterials have to include the full summaryof benefits with Original Medicare benefitsincluded, or is a brief benefits-at-a-glancedocument compliant for employer/uniongroups?37. What if an Employer group plan is verysmall and has no OE period?No.Plan sponsors are strongly encouraged tomake the Part D EOB available in a non-English language.Section 30.8 states that the followingdocuments must be with an enrollment form- Plan Ratings information, the SB, and theMulti-language Insert. Section 30.9 lists thedocuments that need to be provided to allnew enrollees once the enrollment iscompleted.Pre-enrollment documents (like the SB) canbe sent to a multi-person household.However, individual beneficiaries mustcomplete their own enrollment form. Thetypes of documents listed in 30.9.1 arerequired to be sent to beneficiaries whohave enrolled.Please see Section 130 - Employer/UnionGroup Health Plans - for information aboutgroup enrollments. Plan sponsors offeringemployer group health plans are no longerrequired to submit informational copies oftheir dissemination materials to CMS at thetime of use. Chapter 9 of the MedicareManaged Care Manual-Employer/GroupUnion Sponsored Health Plans alsoprovides guidance on disclosurerequirements.Chapter 9 of the Medicare Managed CareManual-Employer/Group Union SponsoredHealth Plans provides guidance ondisclosure requirements and openenrollment.The Final Contract Year 2013 Medicare Marketing Guidelines 8
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question38. Please confirm that File & Use is no longerrequired in the CMS ID?ResponseCorrect.39. The ANOC has a lot of information thatdoes not apply to full benefit dual plansthat would be confusing to members. Canthe EOC be submitted for file and use andthe ANOC be submitted for review toensure members can understand thechanges to their plan?40. Can the Summary of Benefits (SBs) befiled as a standard template prior to CMSbid approval? The 2012 MMGs allowedfor submission of the summary of benefitsto be submitted as a template prior to bidapproval. However, the 2013 MMGs isnow silent on this issue, however stillallows for filing of standard templates.Does this mean all plans have to wait tofile their SBs until their CMS bids areapproved?41. Will the Multi Language Insert be a modeldocument?42. When will we receive the Marketingmaterial models (ANOC + EOC) inSpanish?43. In relation to the multi-language insert,CMS stated this should be submitted fileand use. How should it be submitted if theplan adds additional disclaimers toaddress other languages supported (asCMS directed plans to do)?44. When a non-English speaking beneficiaryis provided with enrollment instructions/form, what required materials must she/hereceive?45. SB for D-SNPs along with FIDE SNPs iseligible for file & use, correct?Per the instructions released with theANOC/EOC, both the ANOC and EOC mustbe submitted file & use.The SB may not be filed as a template thisyear. Plans must wait until their bids areapproved to complete and file their SBs.SBs are now file and use, and there is nooption for CMS review.The multi-language insert is a standardizeddocument and cannot be modified except toinclude additional languages.The translated versions of the ANOC/EOCare available on the marketing website.Only additional languages can be added tothe insert. The document can still be fileand use.See section 30.8 of the MMGs.All SBs are file and use.The Final Contract Year 2013 Medicare Marketing Guidelines 9
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 30 – Plan Sponsor Responsibilities (Updated)Number Question46. Regarding the 5-Star SEP, currently CMSallows plans to list their customer servicestar rating in the Medicare & YouHandbook (M&Y); however, beneficiariesmay use the 5-star SEP only for thoseplans that have an overall 5-star rating, notjust 5 star customer service rating. Thisdiscrepancy has led to confusion amongbeneficiaries and has resulted in allegedmarketing misrepresentation againstMEDICARE. When beneficiaries see a 5-star rating, they don't distinguish betweenthe plan's customer service departmentand its overall performance. In theirenrollment instructions, will plans berequired to specify whether the publishedstar ratings are overall or for a specificarea (i.e. customer service)?ResponseSee section 30.1.21 - Referencing PlanRatings in Marketing Materials - Plans mayonly reference the contract's individualmeasures in conjunction with its overallperformance rating in marketing materials.47. New - When will CMS release the newmodel enrollment form?Enrollment models are part of theEnrollment and Disenrollment manuals.Any updates to these models will beincorporated in the Enrollment andDisenrollment manuals, as appropriate.Section 40 – General Marketing Requirements (Updated)Number Question1. Section 40.1; are we to submit ourmarketing material in HPMS referencingonly (1) the sponsor‟s contractnumber and (2) any series of alphanumeric characters?ResponseThe marketing material identificationnumber used when submitting marketingmaterials in HPMS consists of two parts: 1)the plan sponsor‟s contract or MCE numberfollowed by an underscore and 2) anyseries of alpha numeric characters chosenat the plan sponsor‟s discretion. Whenplaced on actual marketing materials, thematerial identification number must befollowed by either “approved” or “accepted”(or “pending” on websites).The Final Contract Year 2013 Medicare Marketing Guidelines 10
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question2. Section 40.1, Page 17- The Material IDappears to have been changed and nowonly requires Plan Sponsor's contract orMCE number and any series of alphanumerical characters immediately followedby approved, pending or accepted. Datesare no longer mentioned in thissection? The use of dates helps to makemost recent version more readilyidentifiable. Is this simply no longermandatory but allowed or must we trulystop using dates after "approved, pendingor accepted?"ResponsePlan sponsors have the option to includedates if they choose.3. Third bullet removed television ads fromthe “do not require a marketing material IDnumber” requirement. How do we obtainan ID number and how is it to bedisplayed?4. Section 40.6, page 20- We understandthat we can use unsubstantiatedstatements in our logo and product taglines, but can we add a tag line under ourlogo?5. How should plan sponsors indicate thestatus of a marketing material? In theprevious version of the MedicareMarketing Guidelines, plans wereinstructed to include the term “CMSApproved MMDDYYY,” “File & UseMMDDYYYY,” “Deemed MMDDYYYY,” or“Pending CMS Approval” (for websitesonly), as appropriate, immediatelyfollowing the marketing materialID. Should plan sponsors continue to usethe same format and structure (includingthe date stamp) for indicating the status ofthe material?6. Section 40.1, page 17: Will reviewersexpect to see the approved/accepted texton the material at the time of submissionto CMS or are we to wait to insert that untilthe CMS approval/5-day waiting period iscomplete?The material ID number that is placed ontelevision advertisements should follow theguidelines found in section 40.1, MarketingMaterial Identification.Yes.Per section 40.1, materials must beimmediately followed by the status of eitherapproved, pending (for websites only), oraccepted (e.g., Y1234_drugx38 CMSApproved). The date is no longer requiredon materials.The status of accepted should not beplaced on the material that is submitted inHPMS. However, it should be on the piecethat is used in the marketplace.The Final Contract Year 2013 Medicare Marketing Guidelines 11
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number QuestionResponse7. Section 40.1, page 17: CMS did not includeTV ads as an exception to the inclusion ofthe ID (it was included previously). This isproblematic due to limited space issues.Was this an oversight?This was not an oversight. Many plansponsors already include the material IDnumber on television advertisements.Now, it is required for all plan sponsors.8. In the final ANOC/EOC model letters, CMSincluded the File & Use date. This conflictswith the instruction in Section 40.1Marketing Material Identification, whichindicates that the date is no longer arequired part of the material id. Can youplease confirm that the File and Use date isnot required on the ANOC/EOC modelletters?The file & use date is not required.9. Is use of the plan type required for radioand television ads? Do we need to verballysay for example “HMO-POS” after use ofthe plan name in the ad? Section 40.13requires use of the plan type on “allmarketing materials when the plan name ismentioned” and I have not found anexemption from this requirement for verbalmarketing materials elsewhere in the 2013Marketing Guidelines.10. How should we format website material IDsbefore they are approved by CMS? Thecurrent guidelines do not have the sameformat as last year and just mention thewords 'pending'.11. Marketing Material Identification (40.1):During our website submission, it was oncedisapproved because it stated “pending”within the material ID itself instead ofseparately. In order to make sure we do notcommit the same mistake, would thematerial ID status be “pending” (whileawaiting approval) or should it have theapproved or accepted status and separatelystate “pending”?Per MMG section 40.13, plan sponsorsmust include the plan type on all marketingmaterials when the plan name ismentioned. This includes radio andtelevision advertisements.Per section 90.2.2, Plan sponsors maymake the website available for public useduring the CMS review period; however,plan sponsors must include the statuspending on their website until CMS hasgranted final approval/disapproval. Forwebsites, plan sponsors should include thematerial ID followed by the word pending.The website should include the termpending as part of the material ID.The Final Contract Year 2013 Medicare Marketing Guidelines 12
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question Response12. Marketing Material Identification Number forNon-English or Alternate Format Materials(40.1.1): Previous version of the MMG statedthat the approval date for these materials isthe same as the original document (Englishversion). Although the date will no longer formpart of the material id, can these be used anddistributed once submitted or will the samereview/wait period that applied for the originaldocument apply?Once the English version is approved, theNon-English or Alternate Format materialcan be uploaded and distributed.13. Standardization of Plan Name Type (40.13):The exclusions mentioned on the draft versionwere removed; does this mean that thoseexclusions no longer would apply?Please refer to the guidance in 40.13, theexclusion are provided in this section.14. Can you confirm that if marketing material hasthe status of “deemed” due to neither anapproval or disapproval being received withthe review time frame that the material IDshould be followed by CMS “Deemed” ratherthan one of the status designations specificallylisted in Section 40.1 (i.e., approved, pending,or accepted).The material ID should not be identified with“deemed” status. Disregard the lastsentence in Section 90.3.3.15. Can 2 Material IDs (2 different contract #‟s) goon one document (i.e. EOC) and then besubmitted in HPMS under each contractalthough it is the same document?16. Material ID - If a single marketing piece iscreated to encompass MCE contracts and asingle HXXXX contract, do we place two IDson the piece, e.g., the MCE ID and theindividual Hxxxx ID?Yes. If a plan sponsor has an MCE (multicontractentity) number, then the MCEnumber must be used instead of thecontract numbers. If the plan sponsor doesnot have an MCE number, it should createa material ID that incorporates all of thecontract numbers for the contracts that willuse the document.Plan sponsors that submit materials usingthe MCE contract do not need to showindividual contract numbers. The Plansponsor should select the contract(s) inHPMS under the MCE that will apply tomaterials.The Final Contract Year 2013 Medicare Marketing Guidelines 13
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question17. Material ID - Do TV ads now require theMarketing Material ID to be displayed? Ifyes, is it required to be displayed duringthe entire ad?18. Is the Material ID required on TV ads? Yes.ResponseTV ads must include the marketing materialid. The material id should be displayed atthe bottom of the ad and is not required toappear during the entire commercial.19. If you no longer have to have a date withthe material id - how will the five dayperiod be measured?20. Should the material ID include thestatement CMS Approved"21. Can beneficiaries opt out of receiving thematerials at all as long as they know howto request or view materials?22. Do emails to beneficiaries/prospectsrequire the material marketingidentification number?23. Do you need beneficiary okay for alternatemedia for each and every document, orcan one authorization form withcheckmarks for each category suffice?24. Must you advise a member that they havethe ability to change their opinion re:receiving information via electronic media?25. Is it any customer service number or justthe plan customer service number?26. Does the hour of operation requirementapply to the website as well?27. How do we handle hours of operation onmodel documents when it indicates thatthis must be entered in every instancewhere the customer service number isindicated?HPMS lists the date the piece can bedistributed, which is 5 days after uploading.Per section 40.1, material IDs must beimmediately followed by the status of eitherapproved, pending (for websites only), oraccepted. The date and CMS, is no longerrequired on materials.Yes.Yes.One authorization is acceptable as long asit's clear which documents the beneficiarywishes to receive in alternate media.Yes.Any customer service number.Yes.Section 40.8 states: Note: The hours ofoperation need to only be listed once inconjunction with the customer servicenumber, they do not need to be listed everytime a customer service number isprovided.The Final Contract Year 2013 Medicare Marketing Guidelines 14
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question28. Does the TTY # need to be listed eachtime or only once for 40.8ResponseThe TTY # should be listed each time acustomer service phone number is listedper 40.9.29. What constitutes a customer servicenumber? Does a departmental phonenumber, for example, a direct phonenumber or a billing department phonenumber constitute a customer servicephone number?30. What if an agent represents several plansand they want a generic flyer withoutspecific health plan benefits. Does eachplan have to review it or just a lead plan forCMS submission?31. If we want to put a date on the AlternateFormat filed materials, does it still stay thesame date as the English material or thedate the alternate format material issubmitted in HPMS?32. <strong>It</strong> used to be considered event-specificwhen an enrollee or prospective enrolleeprovided an email address. Is this nowconsidered open-ended (provided theperson has the option to opt out)?33. If I submit a material to be used during2012, must I adapt the document to the2013 guidelines, if I continue to use thedocument during 2013?34. Last year we did have to wait 5 days forFile & Use for the EOC. This was waivedbecause of the earlier ANOC date. Willthis be true for this year?The phone number to reach your customerservice staff is considered your customerservice number. Your examples are notcustomer service phone numbers as youhave stated.This could be "multi-plan material" - seesection 90.2.4 for how to file suchdocuments.This is plan discretion.How the email address was obtained woulddictate if it was event specific or not.Marketing materials are required to becompliant with current guidance. If amaterial is no longer compliant for CY 2013,the plan should make the appropriateupdates to the material and resubmit thepiece.The 5 day wait no longer exists for theANOC/EOC.The Final Contract Year 2013 Medicare Marketing Guidelines 15
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question35. If changes are made to the EOC, areincluded in the file and use submission?ResponsePlans should file the final copy of theirANOC/EOCs.36. In the past, the EOC for SNPs has notbeen eligible for File & Use because ofadditional Medicaid information and otherchanges required. Will SNPs now be ableto submit EOCs as F&U?37. Do I understand correctly that it is nolonger required to include "This is anAdvertisement" on the front cover ofpotential enrollee direct mail marketingmaterials?38. We have two new H contracts approvedfor 2013. We would like to know when wecan begin submitting marketing materialsfor these two new contracts.Also, will we currently have File and Usestatus and want to make sure we will beable to submit using File and Use for ournew H contracts as well?39. For the 10% File & Use rule, does thatmean that plans which use non-modelenrollment letters when those models areavailable are having that counted againstthem? Or is it strictly for pieces more likeadvertising which really should not beCMS reviewed?40. If a letter template does not change fromone year to the next, does it need to be resubmittedin HPMS for the new yearagain?41. In Sec. 40.1 (marketing materialidentification), it appears that CMSAccepted" has replaced "File & Use" in thematerial ID that is to appear on the finaldocuments. However the 2013 modelANOC/EOC shows "File & Use". Why isthere inconsistency here? What is thecorrect term that plans should use if amodel document says one thing and theMMG says something different?Yes.No - Section 50.16 lists the mailingstatements and their use. If no envelope isused, the statement needs to be on themailing itself.Marketing material for new contracts can befiled beginning July 1. Section 90.6explains the certification process for newcontracts.Yes, submitting non-model documents,when a model is available is countedagainst the plan sponsor.No.For the ANOC/EOC, plans may use eitherterm "File & Use" OR "CMS Accepted"The Final Contract Year 2013 Medicare Marketing Guidelines 16
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question42. Should we leave off "CMS Approved" untilthe approval has happened? How doesCMS want to see 45-day material inregards to the status after the material ID?43. If you mention only premiums and notdetailed benefits information such ascopays is this still considered a 45 dayreview piece?44. Does this mean file and use statements onmaterial ID`s are no longer required?45. What constitutes a "banner-like" ad?Material? Usage?46. So TV ads now must have a MID? Theremay be space/time limitations to include aMID in TV ads.47. Is "CMS Approved" or "File and Use" stillrequired on the marketing material IDnumber (i.e. Y1234_123456 CMSApproved)?48. Can the cover letter be submitted in HPMSwith the ANOC and EOC under thecombined ANOC/EOC code?49. Social media site still require CMS review?Just not the material ID correct?50. What status should be included in thematerial ID for ad hoc communications thatno longer have to be filed?51. We are not required to include the date onmaterials; however do we need to identifywhether or not it is a CMS approved or File& Use document?ResponsePieces reviewed by CMS prospectivelyshould show "approved".All advertising is now file and use, exceptfor websites.That is correct.An example of a banner-like ad is an adthat scrolls across the bottom of a TVscreen.TV ads do require a material ID, unless theyare banner-like ads.No, only the status is required, e.g.,approved, accepted, or pending forwebsites.The letter will need to be filed separately.The content of the social media site andmessages determines the type of piece it is,and whether it is required to be reviewed,e.g., advertising is file and use.Since Ad Hoc communications no longerare subject to CMS review, no material ID isneeded.The status that is required as part of thematerial ID, informs the reader of the typeof material. If it's approved, it was reviewedby CMS prior to use. If accepted is used, itwas submitted as file and use.The Final Contract Year 2013 Medicare Marketing Guidelines 17
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question52. Please confirm "CMS Accepted" is to beused on all F&U submissions and "CMSApproved" are those pieces manuallyreviewed?ResponseOnly approved and accepted are nownecessary.53. Should sponsors refer to section 40.12 -Providing Materials in Different <strong>Media</strong>Types for guidance concerning alternatematerials (i.e. Braille, large font)?54. The Summary of Benefits guidanceindicates that this will be able to besubmitted file and use this year. However,HPMS does not reflect this. Will HPMS beupdated to match the guidance?55. When mailing marketing materials tomultiple people at same address (i.e.husband and wife) can plan include aseparate ID Card for each member in thesame envelope, or must plan send the IDCard to each member in separateenvelopes?56. In Ch. 4 of the model EOC, the benefits inthe chart must be listed in alphabeticalorder. What about Spanish-languagetranslations of these documents?57. So if the model exhibit letters currently listthe hours of op more than once, if wechoose not to list them more than once,does that make the model a non-model?58. How many times hours of operation needto be listed on Application Form if itconsists of 3 pieces which are 1) Coverletter 2) App Form and 3) Attestation Formas one binder?59. Can a plan sponsor use the MMG 2013 formaterials been submitted to be used for2012? Or can I only use it for materialsthat will be used in 2013?No, section 30.6 - Anti-Discrimination wouldbe more appropriate. "Basic services andinformation must be made available toindividuals with disabilities, upon request."HPMS was updated on July 1.Yes, the ID cards can be in the sameenvelope - see section 30.9.1.The Spanish translation should follow theorder used in the English version.This example would still be a modeldocument.The hours of operation must be listed onceon each material. In the example youprovided, the Cover letter, application form,and Attestation form would be consideredseparate materials.Plans may begin using these guidelinesimmediately.The Final Contract Year 2013 Medicare Marketing Guidelines 18
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 40 – General Marketing Requirements (Updated)Number Question60. Section 40.8.1 requires that materials withan agent/broker phone # must include theplan sponsor`s customer service phonenumber. Please confirm that the plan`snumber is not required if the materials aregeneric and do not include any plansponsor names (i.e. Flyers, BRCs, etc.that only have the agent/broker name andphone #). [Agents are often licensed to sellMA plans for more than one plan sponsor.]61. For file & use is it still 90 % for materialsunder the File & Use process and 10% formaterials under manual review?62. Since you are no longer require theapproval date, how will we tell if thedocument is not an updated version?63. Section 40.1 material ID, when submit adocument they have to use for exampleH1234_testA so once the document isapproved they would have to insert CMSApproved into the document?64. New - In regards to the marketing materialidentification (Sec. 40.1), previousversions required a date placeholder(MMDDYYYY) to be included in thematerial ID that appeared on finaldocuments (for example, the actual CMSapproval date). In the new MMG, the dateplaceholder is not mentioned at all - butsome 2013 model materials such as theANOC/EOC do show a placeholder for thedate. Do plans have the option to include adate on all final documents if they sochoose?65. New - Our plan uses Material IDS (withoutApproval dates) for items that are notsubmitted. Will that cause any issues forCMS?ResponseIf the plan sponsor is not listed, nocustomer service number is required.Ninety percent of file and use eligible piecesmust be submitted as file and use.Sponsors should have an internal trackingsystem to determine if they have the mostupdated version. HPMS will also beavailable to determine the most recentversion.Plan sponsors should add approved afterapproval.The date approved is no longer required. Adate can be used, if the plan wishes.Plans are allowed to create and use theirown material IDs on materials not submittedin HPMS.The Final Contract Year 2013 Medicare Marketing Guidelines 19
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question1. Is the former PFFS disclaimer still requiredto be read aloud/used at salespresentations?ResponseNo.2. Please clarify that plans may discontinuefiling ads with 5 or more benefits for CMSmarketing review 45-day approval and thatthese materials are now File & Useeligible?3. Section 50.1 requires either the legal ormarketing name be used in the FederalDisclaimer. An extreme legal entitydisclaimer for general advertising andmember communications would be quitelengthy especially for large organizationswith many legal entities and it length legaldisclaimer would be very confusing toprospects and members. Can CMSconfirm that “Humana” would be theappropriate marketing name referenced inthe guidance? For example “Humana is aMedicare Advantage Organization with aMedicare contract.”4. For the new Federal ContractingDisclaimer requirements for Cost plans,are plans required to use the insurer‟slegal/marketing name, or the name of theplan itself? <strong>It</strong> seems like, for this particularstatement, it makes more sense to use thename of the product, instead of the nameof the insurer.5. Old MMG 50.1.10; 50.1.11; 50.1.14 whichI call network disclaimers are not in thenew MMG. Again is this because ofappearing in model pieces? If we have aproduct brochure with benefit informationwhat reference material should we refer tomake sure we have all requireddisclaimers?Advertisements that contain plan benefitinformation must include the requireddisclaimers and may be submitted File &Use.The updated MMG gives plan sponsorsmore flexibility with how they choose todisplay the Federal contracting statement.Plans may choose to include their legalname or their marketing name. CMS doesnot dictate requirements for a plansponsors‟ legal or marketing name.The updated MMG gives plan sponsorsmore flexibility with how they choose todisplay the Federal contracting statement.Plans may choose to include their legalname or their marketing name. CMS doesnot dictate requirements for a plansponsors‟ legal or marketing name.Plans sponsors should refer to Section 50of the most recent MMG for requireddisclaimers.The Final Contract Year 2013 Medicare Marketing Guidelines 20
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question6. Contracting statement shows legal andmarketing name - Does this mean weshould not show the plan name?ResponsePlan sponsors should use the legal ormarketing name (which could be the planname) in the disclaimer.7. Old MMG 50.1.4 required the bulleted LISdisclaimer on explanatory materials. NewMMG does not show this disclaimeranywhere. Is this no longer arequirement since it is in the Summary ofbenefits model?8. Please confirm the Extra Help disclaimeris no longer required on the website?Also, can CMS please clarify if the ExtraHelp Disclaimer is still required onmarketing materials that reference Part Dor if this is no longer a required disclaimeroutside of model/standard materials thatinclude the disclaimer?Plans sponsors should follow the mostrecent MMG for required disclaimers.All required disclaimers for websites arelisted in Section 50 of the MMG. The LISdisclaimer is no longer required.9. We would like confirmation that thefollowing disclaimer is no longer neededon materials for marketing educationalmaterials “This event is only foreducational purposes and no plan-specificbenefits or details will be shared".10. Do envelopes that contain more thanmerely the required plan mailingstatement (2013 MMGs Section 50.16)require a 45 day review, or are allenvelopes now 5 day File & Use? The2013 MMGs are now silent on this issue.All required disclaimers are listed inSection 50 of the MMG.Yes, envelopes that contain additionalinformation outside of the mailingstatements should be submitted for review.11. The 2013 MMGs Section 50.2 indicatesthat the disclaimers contained in thissection must be used when „benefitinformation‟ is included in marketingmaterials. We were hoping to get furtherclarification on what is meant by ‘benefitinformation’. Does this mean that thedisclaimers are required when actualbenefit dollar amounts are used in?The term “benefit” is used to describebenefits broadly and is not limited todescribing dollar amounts.The Final Contract Year 2013 Medicare Marketing Guidelines 21
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question Response12. Where can we find the VAIS guidanceregarding how VAIS materials arehandled, such as there must be a clearbreak between true benefit materials andVAIS, and the requirement in the priorMMG about inserting the mention aboutmembers with VAIS not having Appealrights but having grievance rights?13. Last year the following disclaimer wasonly used on materials that were stillmarketing current year benefits.“[Benefits, formulary, pharmacy network,premium and/or co-payments/coinsurance]may change on January 1 ofeach year.” This year the guidelinesstate that it should go on all marketingpieces. If we are marketing in October for2013 benefits isn‟t it confusing to thebeneficiary that we are saying our plansmay change each year?14. Will the Federal Contracting Statementbe required on letters to currentmembers for routine operational issues?15. The 2013 MMGs Section 50.2 indicatesthat the disclaimers contained in thissection must be used when „benefitinformation‟ is included in marketingmaterials. We were hoping to get furtherclarification on what is meant by „benefitinformation‟. Does this mean that thedisclaimers are required when actualbenefit dollar amounts are used inmarketing materials only (e.g. $0premium, $0 co-pay)? Or does „benefitinformation also include such statementsas „low copays‟, etc.?‟Information about VAIS (value-add itemor service) can be found in Chapter 4 ofthe Medicare Managed Care Manual.The disclaimer is required and is stillaccurate for materials marketingupcoming contract year benefits.Yes - per Section 50.1, all marketingmaterials must include the statementthat the plan sponsor contracts with theFederal government.The term “benefit” is used to describebenefits broadly and is not limited todescribing dollar amounts. Anydescription of benefits will require the useof disclaimers outlined in Section 50.2..The Final Contract Year 2013 Medicare Marketing Guidelines 22
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question Response16. If a single marketing piece advertisesmultiple plans including a D-SNP plan,do we place two statements on thepiece, e.g., is a HealthPlan with a Medicare Contract and is a Coordinated Care Plan witha Medicare Contract and a Contract withthe [state] Medicaid Program?Plan sponsors are responsible forincluding only the federal contractingstatements that are applicable. Thereforeif there is mention of D-SNP in theadvertising piece, the sponsor would beresponsible for including the disclaimerfor D-SNPs.17. Is the federal contracting statementrequired on all materials or just thoseconsidered advertising or some sort ofattempt to sell a plan?18. The MMG provides that the co. namemay appear in the federal contractingdisclaimer for MA or MA-PD. What aboutthe Part D standalones?19. Are we required to re-submit anymaterials due to changes in disclaimers?20. Section 50.4 Disclaimer on Availability ofNon-English Translations - Our Planmeets 5 percent threshold for Spanish.Do we put this disclaimer onANOC/EOC, SB, Enrollment Form andall other Marketing Materials" forprospective members direct mail?21. Regarding the change to not include adate in the material ID. Does this meanwe do not need to include the File & Usedate?22. In regards to disclaimers, whenconsidering the websites, certain pageshave content that is targeted toprospects and certain pages are targetedto members. However, both haveaccess to the pages. Is there moreguidance on how to apply disclaimers tothe website?Section 50.1, first sentence states: "Allmarketing material must include thestatement that the plan sponsor contractswith the Federal government."Section 50.1 applies to PDP sponsors aswell as MA plans. This section lists thecontracting statements that must be usedby PDPs.No.Section 30.7 lists the RequirementsPertaining to Non-English SpeakingPopulations.Yes.Disclaimers should be on the pages withthe material that requires the disclaimer.The Final Contract Year 2013 Medicare Marketing Guidelines 23
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question Response23. Please clarify- We have Plan RatingInformation‟s, Language insert availableonline but people can access the enrollmentform prior to seeing these if they wish. Mustwe somehow lock down enrollment apps sothat enrollees can`t access them until afterthey`ve viewed other information?The requirement is plans must make thesematerials available prior to accessing anonline enrollment form. Plans should usethe guiding principles and sound judgmentwhen implementing this requirement.24. Section 50.4 Disclaimer on Availability ofNon-English Translations - Our Plan meets 5percent threshold for Spanish. Do we putthis disclaimer on ANOC/EOC, SB,Enrollment Form and all other MarketingMaterials" for prospective members directmail?Section 30.7 lists the RequirementsPertaining to Non-English SpeakingPopulations.25. Will CMS provide a standard AlternateLanguage Disclaimer for use with writtenmember communication that informs themembers or prospective members that thecommunications are available to them inother languages or formats, or will the planscontinue to be responsible for translating theEnglish Disclaimer?26. Per 50.15, if a directory lists all networkpharmacies in an entire state; would thestate be considered the service area for thatdirectory?27. If we are using stars as a visual symbol,must we include the Disclaimer WhenReferencing Plan Ratings Informationmentioned in 50.14?See section 50.4 for the disclaimer.The service area is determined by eachcontract and PBP's service area.Yes.28. Where will the CMS gold star icon be found? The icon will be provided to 5 star plansvia their Account Manager. Thisinformation is generally provided inOctober.29. Is the VAIS disclaimer (refer to CY2012MMG, Sec. 110.1) no longer required inmarketing materials?VAIS materials are no longer materialssubject to review; thus, the MMG do notdictate VAIS requirements, includingdisclaimer requirements. Plan sponsorsshould refer to Chapter 4 of the MedicareManaged Care Manual for VAIS guidance.The Final Contract Year 2013 Medicare Marketing Guidelines 24
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012Section 50 – Marketing Material Types and Applicable Disclaimers(Updated)Number Question Response30. Some plans want to deviate, using modeldocs and use their own created docssuch as letters etc., is this practiceacceptable?Plan sponsors may create non-modeldocuments; however they must ensure thatall elements of the model are in the nonmodeldocument. In addition, for thosemodels that make a piece eligible for fileand use, plan sponsors should ensure that90% of file and use eligible pieces aresubmitted as file and use.31. New - The Section 50 disclaimers arealso to be said when a CSR is speakingto a beneficiary, correct?For scripts that are required to be submittedto CMS, yes.Section 60 – Required Documents (Updated)Number Question Response1. If the Summary of Benefits includes asection III or IV, please confirm that it willstill require filing under the 45-day reviewprocess.The SB is now a file & use document,regardless of which sections areincluded.2. Must health plans reissue all ID cards tocurrent members if current cards do notmeet these new requirements? Or dothey only have to add this new informationto cards for new members?3. HPIDs have not yet been distributed tohealth plans. What is the effective date ofthis requirement, and when does CMSexpect that health plans must add thisinformation to ID cards?4. 60.1 Section II – References PDPs. CanMA-PDPs include a premium table?5. Can MAOs continue to submit the SB as astandard template prior to approval of finalbids?All health plan identification cardsmust contain the requiredinformation. If plan sponsors haveissued cards in past years that do notinclude the required information, theymust reissue updated cards that arecompliant with the new requirements.CMS will release information abouthow to obtain HPIDs in the fall.Yes.No, the SB can no longer besubmitted as a template and shouldbe submitted as final, populatedversions.The Final Contract Year 2013 Medicare Marketing Guidelines 25
Section 60 – Required Documents (Updated)Number Question6. Please clarify the Health Plan IdentificationNumber (HPID) required to be included onID cards- is this contract #?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012ResponseNo, the Health plan identificationnumber is a number that will beissued by CMS at a later date.7. Section 60.4.3 no longer states that acombined provider/pharmacy directory is 10day model-please clarify if this is still thecase.8. Section 60.1 indicates SB's are to besubmitted as one document under the Fileand Use process, but HPMS still reflects10/45 day review. Please confirm how toprocess.9. Submission of Summary of Benefits withSection III: Can you clarify how an SB thatincludes a Section III is to be submitted?The HMPS memo dated May 31, 2012indicates that plans “must submit allsections of the SB as one document underthe file & use process.” However, theMarketing Code Lookup module in HPMSincludes the code 1061-Summary ofBenefits (SB) with Free Form text (Section3) and specifies for that code that 45-dayreview is applicable and that File & Use isnot available.10. Can the Summary of Benefits (SBs) be filedas a standard template prior to CMS bidapproval? The 2012 MMGs allowed forsubmission of the summary of benefits tobe submitted as a template prior to bidapproval. However, the 2013 MMGs is nowsilent on this issue, however still allows forfiling of standard templates. Does thismean all plans have to wait to file their SBsuntil their CMS bids are approved?11. If the multi-language information is addedto the SB or EOC and not an insert wouldthat make the SB or EOC non-model?Yes, combined provider/pharmacydirectories are still considered modelmaterials if no modifications are made toeither the pharmacy or provider directory.HPMS submission codes will be updatedto reflect the file & use submissioneffective July 1, 2012.Plans should submit all sections of the SBas one document under the file & useprocess. The HPMS codes will beupdated to reflect the file & use statuseffective July 1, 2012.For CY 2013, plan sponsors may notsubmit the SB as a standard template. Allsections of the SB should be submitted asone populated document after bidapproval under File & Use.No, the SB and/or EOC will still beconsidered a model with the inclusion ofthe insert.The Final Contract Year 2013 Medicare Marketing Guidelines 26
Section 60 – Required Documents (Updated)Number Question12. Is there a specific location on the Member IDcard where the HPID needs to be displayed?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012ResponsePer section 60.2.1, the location of theHPID must conform to the specificationsof the WEDI Health Identification CardImplementation Guide.13. Can provider/pharmacy directories beincluded in the ANOC/EOC mailing?14. If we include the Summary of Benefits in ourANOC/EOC mailing do we also need toinclude the Plan Ratings form (as the newChapter 3 states that we must include thePlan Ratings form with the Summary ofBenefits, however, guidance also states thatnothing else can be included with theANOC).15. Can you clarify if notices to membersregarding provider/pharmacy terminationreferenced in Section 60.4 of the Guidelinesrequire CMS review and approval or wouldthis fall under the definition of an ad hocmaterial? If the notice required CMS reviewand submission, what code should plansponsors use to submit these notices.16. We will be offering 9 total HMO plans fortwo contracts in 2013. Of the 9, 8 are MAPD(1 MA-only), 5 are SNP (1 MLTCP, 2 FIDESNP, 1 ISNP, 1 Partial Medicaid SNP).What is CMS‟s preference to breaking outthe different templates (1 MAPD, 1 MA-only,1 SNP)? Since we only have one MA-onlyplan, this will be filed as a populatedversion. The SNP templates can getcomplicated since 3 of the 5 will utilize aSection 4 and will therefore be filed as a 45-Day review.17. Is a new id card needed every year forcontinuing members?18. If plans keep the date in MMID, can it be onthe same line as the MMID?Yes, plans may mail theprovider/pharmacy directory with theANOC/EOC.If a plan sponsor chooses to send the SBwith the ANOC/EOC mailing the planratings information must be included.Provider/pharmacy termination noticescan be considered ad hoc materials andtherefore not subject to review.Since the SB now qualifies as a File &Use document, plan sponsors may nolonger submit it as a standard template.Only if the card changes.Yes.The Final Contract Year 2013 Medicare Marketing Guidelines 27
Section 60 – Required Documents (Updated)Number Question19. If a plan decides to put a date, should weinclude the < mmddyyyy > on the materialwhen submitting to HPMS?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseNo.ust 29, 201220. Where can the WEDI guide be found? The WEDI Health Identification CardImplementation Guide can be found at thefollowing link:http://wedi.org/snip/public/articles/details~74.shtml.21. Do combination medical and prescriptiondrug ID cards require the plan website to bedisplayed? Do they require the HPID numberthat CMS will provide?22. Is a new id card needed every year forcontinuing members?23. If plans keep the date in MMID, can it be onthe same line as the MMID?24. Section 60.1, Summary of Benefits, indicatesit is to be submitted via File & Use. Does thismean it is no longer subject to RO review?25. New - What is considered significantchange?26. New - One provider directory is used formultiple plans, 2 different disclaimers areneeded as one of the plans is a dual plan.Can both of the applicable statements beincluded in one directory? Or, is a separatedirectory required for the Dual plan with theapplicable contracting statement?27. New - Is written notice required for nonprimarycare physician changes, i.e.specialists terminating from the network?CMS will provide additional guidance onthe requirements for ID cards.Only if the card changes.Yes.Correct, the SB is no longer subject toprospective CMS review but may bereviewed on a retrospective basis.CMS does not define what is considered asignificant change for directories. The plansponsor must use their judgment indetermining what a significant change is.In the example presented, the plan mayplace both disclaimers in one directory andstill meet CMS requirements.Plan sponsors must make a good faitheffort to provide written notice oftermination of a contractedprovider/pharmacy at least thirty (30)calendar days before the terminationeffective date to all members who regularlyuse the provider/pharmacy‟s services. Thisis true whether the termination was for orwithout cause.The Final Contract Year 2013 Medicare Marketing Guidelines 28
Section 60 – Required Documents (Updated)Number Question28. New - For the Provider Directories - dochange pages equal directory inserts (thatinclude Provider terminations and add-ons?)2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ust 29, 2012ResponseChange pages are no longer required byCMS.29. New - We would like to clarify if the LIS Rideris still required to be sent with theANOC/EOC as the requirement has beenremoved from section 60.730. New - Plans are still required to provide LISRider and abridged or comprehensiveformularies for the upcoming year for currentmembers, correct?The LIS Rider is considered part of theEOC. CMS strongly encourages plans tosend the LIS Rider in the same envelopeas the EOC. Please refer to theinstructions for the ANOC/EOC on ourwebsite.The LIS Rider and abridged orcomprehensive formulary is an annualrequirement and must be mailed to thebeneficiary annually.The Final Contract Year 2013 Medicare Marketing Guidelines 29
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question1. New regulations state a conference callcan be made for a Scope of Appointment.Does that mean a sales agent canfacilitate a 3-way call to our recorded lineto meet the SOA requirements?ResponseIn Section 70.10.3, CMS lists “conferencecalls” as an example of a means of fulfillinga scheduled appointment. Thedocumentation of the scope of appointmentagreement must occur prior to the actualconference call to fulfill the appointment.2. Are we required to submit educationalevents now? Or is it still optional?3. The guidelines state that we can enter N/Afor agent number –when is that okay todo? Only with Educational Events?4. The 2012 MMG had requirements thatboth the OEV script and the OEV lettercontain information regarding how long amember has to notify the plan sponsor ifhe/she wants to cancel processingenrollment. The 2013 guidelines do nothave similar language. Has thisrequirement been removed from the OEVprocess?5. The 2012 MMG also had a link to a modelOEV letter and a model OEV script, butthe 2013 MMG does not have a similarlink. Will CMS issue a model OEV letterand script for 2013?6. If the provider agrees to make availableand/or distribute generic materials for asales agency that is licensed to sell ALLMedicare Advantage plans that theprovider participates with, would theprovider be required to let health plansdisplay their plan-specific materials?(If generic materials are not "planmarketing materials" then the provider isnot really displaying any planmaterials. Or if the generic materials are"plan marketing materials" is the providerokay to refuse future requests, becausethe sales agency already represents all ofthe plans the provider participates with).Per section 70.10.1, plan sponsors have theoption to upload educational events.Plans should enter N/A for agent numberwhen the person conducting the event doesnot have a National Insurance ProducerRegistry (NIPR) National Producer Number(NPN).Plan sponsors should refer to theappropriate Enrollment guidance forcancellation timeframes.Yes, updated models will be issued withinthe next few months.A provider is free to determine which type ofmaterials it will make available and/ordistribute, as long as they are willing tomake available and/or distribute materialsfrom all of the plans with which itparticipates.The Final Contract Year 2013 Medicare Marketing Guidelines 30
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question7. Sections 70.12.1 - Does the term“sales/appointment forms” include aBusiness Reply Card (BRC)? The BRC isused by a sales agent to obtain permissionto call the beneficiary and discuss MedicareAdvantage plans and schedule amarketing/sales meeting.ResponseA business reply card can be used as anappointment form.8. Would it be permissible for a provider tooffer a Business Reply Card to theirpatients if this was done during an objectivediscussion of Medicare Advantage plansand the provider was not assisting withenrollment decisions, but only providingobjective information about MedicareAdvantage in general?9. If a member goes in for a preventiveservice such as a screening mammogrambut then the service becomes diagnosticbased on the results, are plans permitted toreward as a preventive service since themember has no control over how theservice is billed by the provider (i.e.preventive vs. Diagnostic).10. In addition, we have filed for 2013 to covera supplemental annual routine physicalexam that is above and beyond the annualwellness visit provided by Medicare. Is itpermissible for plans to provide rewardsand incentives for supplemental routinephysical examinations?11. We cover Medicare covered preventiveservices at $0 cost share beyond those thatMedicare covers at 100% such asglaucoma screenings. Is it permissible forplans to provide rewards and incentives forpreventive services that the plans charges$0 cost share where Medicare wouldrequire some member cost share?If a beneficiary requests contact informationfor a plan sponsor, a provider may offer thebeneficiary a business reply card(s).Yes. In the example provided, themember‟s appointment began as apreventive service with zero dollar costshare;therefore, a reward or incentive ispermissible.No.No, it is not permissible. Rewards andincentives may only be offered to currentmembers for Medicare covered preventiveservices that have a zero dollar cost-share.The Final Contract Year 2013 Medicare Marketing Guidelines 31
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question12. How long are plans allowed to contactbeneficiaries who have responded toBusiness Reply Cards (BRCs)? The 2012MMGs stated that permission given by abeneficiary to be called or otherwisecontacted (BRCs) is to be considered shortterm,event-specific, and may not be treatedas open-ended permission for futurecontacts. This language is not contained inthe 2013 MMGs.ResponseSection 70.6 - Marketing throughUnsolicited Contacts states the following,“permission given to be called or otherwisecontacted must be event-specific, and maynot be treated as open-ended permissionfor future contacts.”13. Are plans allowed to collect leads through, forexample SEP marketing activities, prior to theAEP, for future contact during the AEP?14. Section 70.9 has a note. If this is truly aneducational/retention event where no salesinformation is provided, would we still be ableto post an announcement to our Facebookpage, where most of the “Friends” aremembers?15. In section 70.2 it states, “Plan sponsors musttrack and document items given to currentmembers.” Where is this documented?16. CMS clarifies that the SOA should bedocumented 48-hours in advance of theappointment "when practicable". Does CMSdefine practicable? Or is this an Organizationdecision?17. How long are plans allowed to contactbeneficiaries who have responded toBusiness Reply Cards (BRCs)? The 2012MMGs stated that permission given by abeneficiary to be called or otherwisecontacted (BRCs) is to be considered shortterm,event-specific, and may not be treatedas open-ended permission for futurecontacts. This language is not contained inthe 2013 MMGs.Please refer to guidance provided inSection 70.6 and 70.7 of the MMG.Plans are allowed to advertise educationalevents (via Facebook and other means)provided they are advertised as such.Documentation should be kept with the plansponsor.CMS does not define practicable. Plansponsors should use the guiding principlesoutlined in Section 10 of the MMG to define“practicable”.Section 70.6 - Marketing throughUnsolicited Contacts states the following,“permission given to be called or otherwisecontacted must be event-specific, and maynot be treated as open-ended permissionfor future contacts.”The Final Contract Year 2013 Medicare Marketing Guidelines 32
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question18. Section 70.9 – how does these guidanceimpact renewal sales presentations? Wecurrently file advertisements in HPMS andget approval for renewal sales presentations,which then are advertised in our newsletterfor current members, to review changes forthe new plan year. While there isn‟t a hugeattendance, members appreciate usreviewing changes for the new year inperson. Does the note in 70.9 only impacteducational events so that we could continueour renewal sessions as sales sessionscontinuing to list these dates in HPMS? Wedo review plan specific benefits andpremiums at these sessions.ResponseRenewal sessions can be conducted in theexample provided, as it targets only currentmembers.19. New - AHIP Certification for agentsextensively covers fraud waste and abusewill CMS honor this requirement having beenmet and not expect Plans to repeat this withagents using their own program? If not willCMS allow Plans to accept attestation fromagents completing this requirement from acompeting Plan so agents don`t have tocomplete this require from 6 different Plans ifthey are appointed with that many? Thankyou.20. New - We are under the impression gift cardsare not allowed as they can be transferrableto cash.21. New - What does "Medicare limiting chargesapply" mean?22. New - How do you track the $50 limit whenthere is a crowd present? Is the $15 limit toone per visit or can you provide multiple ofthe $15 dollar item/service at the same visit.Plans are responsible for ensuring thatagents meet the requirements specified fortraining and testing. Training and testingfacilitated by a third party is acceptable;however the sponsor must be able toprovide documentation that training andtesting completed by the third party iscompliant with the guidance.Correct-Gift cards that may be readilyconverted to cash are not acceptable.Limiting charges are 115% of the Medicareallowable amount for a non-participatingMedicare provider. These charges couldapply when a beneficiary obtains routineservices from a non-contracted provider,e.g., PFFS, PPO, or HMOPOS. The plan'sbid determines whether the beneficiary orthe plan is liable for the limiting charges.Plan sponsors are responsible for trackingthe nominal limits. CMS does not specifyhow this should be conducted. Thereshould be a $15 limit for each beneficiary.The Final Contract Year 2013 Medicare Marketing Guidelines 33
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question23. New - Are gas cards of $10 value allowed asa reward for attending a seminar?ResponseCards that can be converted to cash are notacceptable; therefore gas cards that can beconverted to cash are prohibited.24. New - If you give out coupon booklets - dothe coupons have to be less than a certainamount?25. New - Would you please clarify the use of giftcertificates and gift cards (section 70.1Nominal Gifts)? Cash gifts are prohibitedand gift certificates and gift cards that can bereadily converted to cash are prohibited. Thespeaker used gift cards as an example of anominal gift. Please clarify what types of giftcards or gift certificates are allowed.26. New - Why require OEV phone calls tomembers, but not require a phone number onthe enrollment application?27. New - Can a member disenroll during anOEV call?28. New - Are applications submitted byemployees of the health plan also required tohave an OEV?29. New - For OEV, last year CMS has said thatthe plan can send the letter first and then dothe 3 phone attempts. Is that being changedagain for this year?30. New - Please clarify "potential enrollee" and"prospective member."The coupon must meet the requirements fornominal gifts.Gift cards or certificates that cannot bereadily converted to cash are acceptable.A telephone number is an element on theenrollment form.Members can request that their enrollmentbe cancelled during the OEV call.OEV calls apply to all enrollmentseffectuated by agents/brokers (contractedor employed).In accordance with Section 70.8, plansponsors must make a minimum of threedocumented attempts to contact theapplicant by telephone within fifteen (15)calendar days of receipt of the application;the first two attempts must be made withinthe first 10 days. Plan sponsors that do notsuccessfully reach the beneficiary on thefirst or second attempt must send theapplicant an enrollment verification letter inaddition to making the third documentedoutbound verification call attempt within the15 day timeframe.Potential enrollee and prospective memberhave the same meaning.The Final Contract Year 2013 Medicare Marketing Guidelines 34
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question31. New - Does CMS categorize money rebateincentive as a gift certificate?ResponseMonetary rebates are not considered giftcertificates.32. New - Can you advertise Member-Onlyevents via newspapers if they are clearlylabeled "Member-Only Events"?33. New - Can we distribute plan change formsat member meetings we hold in October togo through the ANOC with our members?34. New - Do educational events need to besubmitted through HPMS for educationalevents for members only? For educationalevents directed for the public (may includenon-members)?35. New - Member only events - to helpmembers utilize their benefits -should not besubmitted to CMS as sales events - correct?36. New - In regards to section 70.9. Theguidance says that the plan can not advertisean educational event and then hold a salesand marketing event immediately following atthe same venue, which implies the plan didnot advertise the sales/marketing event. Canwe assume that the plan CAN hold asales/marketing event shortly after aneducational event if it is advertised?37. New - If a beneficiary chooses to cancelhis/her enrollment during an OEV call, arethey required to cancel their enrollment within7 days of the OEV call or letter or by the lastday of the month in which the enrollmentrequest was received (whichever is later) ordo they truly have either 7 days from the dateof the OEV call/letter or by the day prior toeffective date, whichever is later?CMS expects that member only events willbe advertised in a way that reasonably onlytargets members. Plans should workdirectly with the Account Manager if theyhave a question on a specific advertisingstrategy.Plans may distribute plan change formsduring the AEP; however this should beentered as a sales event in the eventsmodule.CMS does not require submission ofeducational events in HPMS.Member only events designed solely toeducate members on existing or upcomingbenefits do not need to be entered inHPMS.Marketing and educational events must beseparate. If a plan would like to hold a jointsales and education event they may;however it should be uploaded in the salesevent module.The beneficiary may cancel their enrollmentthrough the OEV process even if theenrollment has become effective. Pleasereference the memo released on November4, 2011-Correction of Timeframe forCancellation of Enrollment RequestContained in Outbound Enrollment andVerification CommunicationsThe Final Contract Year 2013 Medicare Marketing Guidelines 35
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 70 – Rewards and Incentives, Promotional Activities, Events,and Outreach (Updated)Number Question38. New - Is there still a 48 hr requirement for anagent to present non-health care products ifrequested by a bene during a MA/PDPappointment (life insurance, annuities)?ResponseThe 48 hour requirement does not apply tonon-health care products if the beneficiaryhas requested information.39. New - If a last minute change is made on theday of the event, and a different agentpresents, will this count against the plan if notentered prior to the event?40. New - Can a provider attend a marketingevent to provide health screening activities?41. New - Is the contracting statement requiredon health education materials?42. New - Are OEV calls required to berecorded?43. New - Do we have to submit memberorientation events?44. New - Are PACE, SPAPs, auto-enrollments &reassignments effectuated by CMS no longerexcluded from the OEV requirement?45. New - Do events need to have a plantranslator if it is determined that the audienceis non-English speaking? Can an audiencemember do the translating, or do we have tohave a plan translator at the event?46. New - Clarification - under educationalevents a plan`s new member meeting canbe held which will discuss plan-specificmaterial, but no enrollment may be taken,correct?If the agent changes during the sales eventthis will not count against the plan.Plan sponsors may not conduct a healthscreening activity at a marketing event.The contracting statement is only requiredon marketing materials. Health promotionmaterials that do not include any specificplan related information are not consideredmarketing materials and do not need to besubmitted in HPMS.OEV calls must be documented. Plansponsors may record or use anothermechanism for documenting.Member orientation events are considerededucational; therefore they do not requiresubmission.PACE, SPAPs, auto-enrollment andreassignments are still excluded from theOEV requirement.CMS expects that plans will providereasonable accommodations to meet theneeds of their audience.Enrollment may not be conducted atmember only events designed to educatethe member.The Final Contract Year 2013 Medicare Marketing Guidelines 36
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 80 – Telephonic Activities and Scripts (Updated)Number Question1. Draft guidance stated that "From October1 - February 14, plans sponsors mustoperate a toll-free call center." FinalVersion states "Plan Sponsors mustoperate a toll-free call center….. And Laterstates "Note: From February 15 toSeptember 30, plan sponsors may usealternative technologies on Saturdays,Sundays and Federal Holidays." Finalversion also refers back to "During thistime period" but has not time period torefer back to. Confirmation that we mustnow be open 10/1-2/14 rather than 10/15-2/14.ResponseThe 10/1/12 date is correct.2. Telephonic contact - Does an auto dialercampaign for marketing topics, e.g., AEPdates, upcoming plan changes, newbenefits, etc., require CMS approval?3. Are the requirements for non-Englishspeaking populations applicable for agentcall centers?Per Section 80.2 Expectations for Scripts,informational scripts designed to respond tobeneficiary information requests andprovide objective information about the planand Medicare program do not requiresubmission into HPMS for review andapproval. However, plan sponsors mustretain these scripts and make themavailable upon CMS request. CMS expectssponsors to incorporate in all their scripts allrelevant requirements outline in the MMGs(e.g. hours of operation, TTY number etc.).Plan sponsors are responsible for ensuringthat their contractors are compliant with theMMG. To the extent that a plan sponsorhas delegated or sub-contracted some of itsmarketing functions to other entities, all ofthe requirements that the plan sponsormust comply with translate to the delegatedentity or sub-contractor.The Final Contract Year 2013 Medicare Marketing Guidelines 37
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 80 – Telephonic Activities and Scripts (Updated)Number Question4. New - Please confirm 8-8 7 days appliesto Part C member service as well as PartD. <strong>It</strong> used to be "strongly suggested" but Iinterpret the new guidelines to state it isrequired.5. New - If a telephonic enrollment starts onan inbound call and the call disconnects,when the beneficiary calls back in tocomplete the enrollment can the Agentproceed with the enrollment where the callwas dropped? Or does the Agent need tostart the telephonic enrollment over fromthe beginning?6. New - Is it required to provide theenrollment form and other requiredinformation at the time of enrollment ifmeeting with an agent? Or can it be mailedafter the appt?7. New - What about Telesales? Do theyhave to be open from 8am-8PM 7 days aweek?8. New - Must there be live sales agentsavailable during all the required customerservice hours?9. New - Changes to hours of operationsdon`t require a material to be resubmitted,does this hold true for phone numberchanges also? What about the changefrom 10/15 to 10/1?10. New - To satisfy the 48 hour advance SOAcontact, is the actual time that the SOA isexecuted required to be captured andcompared to the actual appointment time?11. New - Does the employer group CustomerService Center have to adhere to the 8/8,7 day hours?ResponseThe customer call center requirementsapply to Part C and Part D plans.If a beneficiary is disconnected from atelephonic enrollment the agent mayproceed where the call was dropped off ifthere is documentation in the system ofwhat had been previously discussed.CMS required materials should bedistributed at the time of enrollment.Telesales are not required to be availableduring the customer service call centerhours.Live sales agents are not required duringthe customer service call center hoursPlan sponsors are not required to re-submitmaterials if there is a change in the phonenumber, hours of operation, or the datechanging from 10/15 to 10/1.The time for the 48 hour requirement shouldbe compared to when the initialappointment was scheduled.No.The Final Contract Year 2013 Medicare Marketing Guidelines 38
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 80 – Telephonic Activities and Scripts (Updated)Number Question12. New - If our offices are located in the CSTtime zone and we operate in the State ofHawaii, do we need to operate on HI TimeZone of 8-8?ResponseYes, the call center should operate 8-8, 7days a week according to the time zones forthe regions in which they operate.13. New - Section 80.3 indicates PlanSponsors may not Request beneficiaryidentification numbers (e.g. Social Securitynumber.14. New - Section 80.1 - Call CenterRequirements - Could you please clarifythat live customer service representativesmust be available on New Year Day?Thank you.15. New - Please answer whether or not alldisclaimers must be said during phone andface to face interactions. (Section 50 and80)16. New - Are the requirements for non-English speaking populations applicablefor agent call centers?17. New - Section 80.4 indicates telephoneenrollment scripts must be submitted intheir entirety (bullets or talking points arenot acceptable). Does this mean that CMSexpects telephonic enrollment scripts to beread verbatim? If so, are therecircumstances which CMS would allow forany deviation (i.e. saying can instead ofcannot)? Please note, Section 80.5 CMSindicates that the Telephone Sales Scriptsmust be read verbatim.Correct-Plan sponsors may not requestbeneficiary identification numbers except ininstances where it is needed to verifymembership, enrollment eligibility or anenrollment request.Unless otherwise directed by CMS, callcenters are required to have customerservice representatives available on NewYear‟s Day.Disclaimers are required (as applicable) onmarketing materials, which include scripts.A face to face interaction is not a marketingmaterial.Section 30.7 is applicable to plan sponsors‟call centers.CMS expects that CSR's use the scripts asthey are submitted in HPMS.The Final Contract Year 2013 Medicare Marketing Guidelines 39
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 90 – The Marketing Review ProcessNumber Question1. Does CMS plan on releasing any foreignlanguage model documents for 2013?ResponseYes, this information will be released viaHPMS.2. When will the Model documents forEnrollment Forms and Scope ofAppointment be available?3. Section 90.2.1, Page 68- Discussessubmission of Non-English Materials orAlternative Formats- No Mention of 5%rule? Has this been retracted?4. How will plan sponsors determine whichmaterials to submit under file & use vs.which materials to submit for a 45-dayCMS review?5. Section 90.8 (Template Materials)differentiates between "standard" and"static" templates, but does not adviseplan sponsors whether the templatesshould be submitted under file & use or45-day review. How should plansdetermine whether to submit a templateunder file & use or 45-day review?6. How should we format website materialIDs before they are approved by CMS?The current guidelines do not have thesame format as last year and just mentionthe words 'pending'.7. MMG § 90.7 - Model Materials, lists“adding any applicable disclaimers” as anallowable alteration to CMS modelmaterials. Does this mean that we arerequired to put applicable disclaimers onmodel documents (even if they are notincluded in the model), or does it simplymean that we have the option to add saiddisclaimers?Updated enrollment models will be releasedwith the updated enrollment guidance. Atthis point, CMS does not intend to issue anupdated scope of appointment form for2013.Please refer to Section 30.7 for additionalguidance on requirements pertaining toNon-English speaking populations.Please use the material code look-up in themarketing module of the HPMS. This toolindicates the submission status of eachcode.Whether a marketing material piece iseligible for file and use is determined by thepiece and its category code. Please referto the Marketing Code Look-up Module forthe review time frame.Per section 90.2.2, Plan sponsors maymake the website available for public useduring the CMS review period; however,plan sponsors must include the statuspending on their website until CMS hasgranted final approval/disapproval. Forwebsites, plan sponsors should include thematerial ID followed by the word pending.If a plan sponsor chooses to modify amodel they must include any requireddisclaimers. Plans sponsors using themodel without modification have the optionto include applicable disclaimers on thematerial.The Final Contract Year 2013 Medicare Marketing Guidelines 40
Section 90 – The Marketing Review ProcessNumber Question8. Static templates - What is the significanceof the reference to File & Use in thedefinition of static templates? Does CMSintend that static templates cannot be filedfor 45 day review, and can only be filedunder the File & Use provision?9. If the plan has material that was approvedfor CY 2012 and that remains accurate forthe 2013 plan year (and the plan wishes tocontinue to use the material in themarketplace) are we required to updatethe MMID line?10. Static Template: "LIS Rider” was includedunder "variable data fields exempt fromthe template resubmissionrequirement”. Do you mean the LIS Riderdocument is considered a static template?11. The HPMS manual directs us to use thematerial codes for “Final ExpeditedReview.” But there are not Final ExpeditedReview codes for every type of material –Most notably file & use advertising. Forexample, we have uploaded templatesusing 4002 (F&U Newspaper Ad) But theclosest final description “4022 Final ExpRev – Newspaper Ads with Benefits”which is 45 days for the initial approval,not file & use.12. Section 90.7, Model Materials (page 76).Does this mean that plan is *required* toput applicable disclaimers on modeldocuments (even if they are not includedin the model)? Or does it simply mean thatplan may *choose* to add saiddisclaimers?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseStatic templates may or may not be file &use. The ability of a material to besubmitted file & use is dictated by thesubmission code in HPMS, not by whethersomething is a static template.No.Yes, the LIS Rider is considered a statictemplate.Advertising templates should not besubmitted as standard templates since theymay be submitted as File & Use.Plans may choose to add any missingdisclaimers.The Final Contract Year 2013 Medicare Marketing Guidelines 41
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 100 – Plan Sponsor Websites and Social/Electronic <strong>Media</strong>(Updated)Number Question1. Are Health and Wellness websitesincluded in the guidance that live reviewsonline for websites are needed for thereview process and screenshots will nolonger meet CMS‟ expectations?ResponseHealth and wellness websites that do notmention benefits are not subject to review.2. We have had challenges with previousweb page and social media submissions inthat the URL submitted for approval mustcontain “www.” in order for the CMSreviewer to view the page. However, manyURLs do not contain the “www.” prefix anylonger, including a major social media site.When “www.” is added to the URL for thissocial media site, it defaults the vieweraway from our company web page on thesite and to a user login page. Please let usknow the proper procedure for submittingweb pages that do not use” www.” in theirURL.3. What if that disapproved portion is a linkfrom other pages - how does that work?4. What are the rules around building a socialnetwork site in which members talk toeach other about the experiences with theplan?5. When something is disapproved on thewebsite, is there a time limit to make thecorrection?6. Is it acceptable to announce aneducational event for current members onFacebook since many current membersare on Facebook?7. For online store websites should CMS beconcern about formulary data presentedas tool finder to beneficiaries? Should aCMS pharmacist look at the websitesection on formulary area presented byplans?Plan sponsors should submit an active linkto the website for review. The reviewershould be able to access the webpage if theURL does not have a prefix.Work with your AM or Marketing Reviewer.CMS has no policy regarding the portions ofsocial media sites in which customers areallowed to have discussions and shareexperiences.Work with your AM or Marketing Reviewer.<strong>It</strong> is acceptable to announce educationalevents for current members on Facebookas long as the content of the announcementhas been submitted to CMS andapproved/accepted.Plan sponsors are responsible for ensuringthe accuracy of formulary informationpresented on websites. This would includeinformation presented on a plan sponsors'website or information presented on a sitewith which the sponsor contracts, (e.g., aFMO).The Final Contract Year 2013 Medicare Marketing Guidelines 42
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 100 – Plan Sponsor Websites and Social/Electronic <strong>Media</strong>(Updated)Number Question8. New - Web sites are no longer required tobe compliant with Section 508 of theRehabilitation Act?ResponseIncorrect. Websites are required to be 508compliant (see Appendix 2 of the MMG).9. New - What if that disapproved portion is alink from other pages - how does thatwork?10. New - May you go over social mediausage...Facebook pages11. New - What are the rules around buildinga social network site in which memberstalk to each other about the experienceswith the plan?12. New - Can you please confirm that thenew Summary of Benefits and Coveragedocuments added by Section 2715 of thePHS Act do not apply to MA plans?13. New - When something is disapproved onthe website, is there a time limit to makethe correction?14. New - Is it acceptable to announce aneducational event for current members onFacebook since many current membersare on Facebook?Given that each situation is unique, pleasediscuss any specific concerns with yourAccount Manager and/or MarketingReviewer.Plan sponsors may have Facebook pages.Per Section 100, plan sponsors are allowedto use social/electronic media. These toolsare still considered marketing materials andsubject to the MMG.Medicare health and drug plans are onlyrequired to produce the Summary ofBenefits document that is generated fromHPMS and referenced in Section 60.1 ofthe MMG.No. However, if any portion of a plan‟swebsite is disapproved, the disapprovedportion must be removed from the websiteimmediately.Plan sponsors may announce eventsthrough social media provided anymarketing guidance for advertising theevent is followed.The Final Contract Year 2013 Medicare Marketing Guidelines 43
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 120 – Agent/Broker Compensation (Updated)Number Question1. Beneficiary notifications when Unqualifiedvs. Unlicensed agents submit applications:Is this notification only required when theagent is unlicensed or should thebeneficiary also be notified when the agenthasn`t completed the entire certificationprocess?ResponseBeneficiaries must be notified when anunqualified agent/broker has enrolled themin a plan. Unqualified agents/brokersinclude agents/brokers who are unlicensedor have not completed the certificationprocess.2. Do we need to submit the agent/brokerattestation?3. Regarding compensation, what are theguidelines for paying FMO`s/TMO`s.There seems to be some confusion onwhen, how, and how much over ride to paythe FMO`s/TMO`s4. Do the agents that draw base salaries areconsidered employed agents are do notfall into CMS guidance?5. Under the agent/broker compensationmodule, if you employ agents and contractwith external agents and brokers; thecorresponding amounts you submit mustapply to both or include amounts whichapply only to external agents/brokers.6. Beneficiaries that enroll in dual plans, theiragents may get compensation for both theplans. Can it exceed the FMV approved byCMS since it‟s the addition of the twoplans?The agent/broker attestation is part of theannual plan agent/broker compensationamount submission process in HPMS.TMOs typically receive two types ofcompensation: 1) compensation forenrollment and 2) compensation for otherservices. TMO compensation forenrollment must follow the compensationrules for independent agents. TMOcompensation for other services must beconsistent with local market rates for thoseservices.Agents who receive a fixed amount and sellexclusively for one plan are exempt fromthe independent agent compensation rules(like employed agents).When submitting agent/brokercompensation information in HPMS, theHigh/Low amounts entered only apply toindependent agents/brokers.Compensation paid to agents for enrollingbeneficiaries in dual plans (e.g., a cost planand a separate PDP), cannot exceed theFMV amount respectively for each plan.The Final Contract Year 2013 Medicare Marketing Guidelines 44
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 120 – Agent/Broker Compensation (Updated)Number Question7. This may be an enrollment question, butwe discussed 120.2, terminated agents.Do beneficiaries have until the date ofnotification plus 2 months to make adecision to remain in a plan or change?ResponsePlans should refer to the enrollmentguidance in Chapter 2 of the MMCM andChapter 3 of the PDM regarding beneficiarycancellation timeframes.8. New - When will 120.3 Annual Up-datesbe available?9. New - Has the 2013 agent compensationbeen released? If so, where is it? If not,when will it be released? Thanks10. New - What SEP code should be used ifan agent is terminated and the memberwishes to make a change.11. New - Are plans allowed to collect leadsthrough, for example SEP marketingactivities, prior to the AEP, for futurecontact during the AEP?12. New - Regarding agent charge backs: itseems that the guidelines are based on aCY basis. For those of us with only a D-SNP plan (and enroll using SEP), can wepay renewals and charge back on aconstant rolling year?13. New - If an agent is termed for fraud (i.e.forging signature on an enrollment form)does CMS need to be notified?This information was released via HPMS onAugust 21, 2012.Compensation rates for CY 2013 werereleased via HPMS on May 3, 2012.This situation would be considered anexceptional circumstance SEP.Plans should use the guiding principleswhen determining whether beneficiarycontact is appropriate. Note that Section70.6 states permission to be contacted isconsidered to be event-specific and maynot be treated as open-ended permissionfor future contact.No, agent/broker compensation can only bepaid on a calendar year basis, never arolling year.Plans should notify the appropriate StateAuthority when an agent is terminated.The Final Contract Year 2013 Medicare Marketing Guidelines 45
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012Section 160 – Allowable Use of Medicare Beneficiary InformationObtained from CMSNumber Question1. Can members opt-in via an online form (onplan website or member portal) or are werequired to obtain a paper form frommember stating they would like to opt-in.ResponseElectronic confirmation is appropriate.Appendix 1 – DefinitionsNumber Question1. Does a member retention letter (urging themember to continue enrollment with theplan) qualify as an Ad Hoc EnrolleeCommunication?ResponseAd hoc materials are customized or limitedto a subset of enrollees. If a material isbeing sent to the entire membership, it willnot qualify as ad hoc enrolleecommunication.Appendix 2 – Related Laws and RegulationsNumber Question1. Are websites required to be 508-compliant? <strong>It</strong> was not included in theguidelines this year.ResponsePer Appendix 2, all plan sponsors arerequired to have an Internet website that iscompliant with web-based technology andinformation standards for people withdisabilities as specified in section 508 of theRehabilitation Act.Appendix 4 – Multi-Language InsertNumber Question Response1. In Appendix 4 (the Multi Language Insert)it looks like there was a technical issuewith the translations for Arabic and Hindi--nothing appears on the sheet. Is CMSgoing to make another, complete versionavailable for health plans to utilize?The CMS Marketing Web page contains theMulti-language insert in the zip fileannouncing the release of the MMG.Please click on the link titled 2013 MedicareMarketing Guidelines from the following webpage to view the information:http://www.cms.gov/Medicare/Health-Plans/ManagedCareMarketing/index.html?redirect=/ManagedCareMarketing.The Final Contract Year 2013 Medicare Marketing Guidelines 46
General Marketing Questions (Updated)Number Question1. Do the 2013 Marketing Guidelines applyto marketing materials that will be usedduring the AEP season starting thisOctober since they will apply to plansoffered in CY 2013 or do we use the2012 Marketing Guidelines through theend of the year?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseThe recently released MMG are applicable forCY 2013 materials used during the AEP.2. Will a red lined version of to theMedicare Marketing Guidelines beavailable to plans?3. Will the Medicare Marketing GuidelineTraining be recorded and when will therecording be available?4. We have multiple customer servicephone numbers for our various Medicareplans. We typically create materials suchas our formulary, pharmacy directories,and letters to target multiple plans.Model documents generally includereferences to one Customer Servicephone number (and TTY) throughout thematerial. For plans with multiple phonenumbers would it be OK to list all phonenumbers once and then refer thebeneficiary back to that page at eachreference in the document thereafter?Or even better, could we insert a contactpage in the document and refer thebeneficiary to that page?CMS has significantly revised the MedicareMarketing Guidelines in almost every section;therefore a redlined version will not bereleased.The webinar was recorded and is availableanytime by clicking on the following link:http://www.visualwebcaster.com/CMS/87543/event.html.Plan sponsors with multiple customer servicenumbers should submit these documents inHPMS as static templates with a placeholderfor the customer service number. SeeSection 90.8.2 of the MMG for moreinformation on static templates.The Final Contract Year 2013 Medicare Marketing Guidelines 47
General Marketing Questions (Updated)Number Question5. We note that the draft MedicareMarketing Guidelines eliminated thedistinction between general advertisingand explanatory marketing materials;and that change has carried through tothe final Medicare Marketing Guidelinesreleased on June 7, 2012. We havealso noted that the new guidelines havedispensed with the list of File & Useeligible materials, and instead refer tothe Material Code LookUp function inHPMS to determine what materials maybe submitted File & Use. With theelimination of explanatory marketingmaterials as a category, we interpret thatthe impact of this change is to classify alladvertising material as eligible for File &Use submission, with the exceptionof:4006 – Internet Web Pages 4011 –Scope of Sales AppointmentConfirmation Form (if non-model) allFinal Expedited Review codes. Is this acorrect interpretation?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseCMS no longer makes the distinction betweengeneral advertising and explanatorymarketing materials. Instead, CMS requiresmaterials that contain benefit information toinclude the disclaimers in §50.2.6. What does OMB mean? OMB is the acronym for the White HouseOffice of Management and Budget.7. When ad-hoc enrollee code is removed,what marketing codes should plans useto submit plan created material thatwould require a 45 day review becauseit contains benefit information?Advertising materials that include benefitinformation are required to contain thedisclaimers in Section 50.2 and can besubmitted using File & Use.8. Does the NCDs uploaded through theplan sponsor website, needs to bereviewed by CMS?9. If stuff was cut from MMG but is notreplaced by information that contradictsit--in other words if it is just cut, doesthat mean the rules cut no longer apply?No.In the 2013 MMG update, CMS removed a lotof the prescriptive language found in previousversions of the MMG. This does not mean inevery instance that those rules no longerapply. What it does mean is that whenorganizations develop their marketingstrategies and activities, they should use theguiding principles (MMG, section 10) alongwith the requirements contained in the otherMMG sections to determine the bestapproach.The Final Contract Year 2013 Medicare Marketing Guidelines 48
General Marketing Questions (Updated)Number Question10. Why was the decision made to makethe guidelines public prior to the trainingor an HPMS memo?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseThat has been our process for quite sometime. The MMG was loaded onto our websitebefore the release of the HPMS memo toensure that the most recent MMG wereavailable when they were announced.Additionally, it is important for individuals tohave an opportunity to review the MMG priorto the training so that they can ask questionsaccordingly.11. Is the marketing mailbox going to beavailable and will the slides presentedtoday be distributed?The marketing mailbox is still available. <strong>It</strong> isavailable to both the ROs and plan sponsors.This presentation materials are available onthe following site:http://www.cmsdrughealthplanevents.org/cms/.12. Do we have a word version of the MMGfor internal use so cut/paste activitiesfor cheat sheets would be available?13. How can we tell if a document isstandardized or not? Is there a listsomewhere?14. New - Are appeals and grievancesprocedures still required to be in presalematerials?15. New - How do these MMG`s affect orimpact the "Dual Eligibles" Medi/Mediclients in CA?There is not a word version that is available.At the present time, the Summary of Benefits,ANOC/EOC, Plan Star Ratings document, andMulti-Language Insert are standardizeddocuments.No.The MMG are applicable to all health and drugplan sponsors, including Dual Eligible SpecialNeeds Plans.16. New - If we have a pending contract,when will we be able to submitdocuments?17. New - Will you be discussing changesto EOBs at all or will there be anothertraining session to discuss thosespecifically?Plans can submit materials for a pendingcontract as soon as the contract is available inHPMS. These materials will be conditionallyapproved until the contract approval is final.At this time, CMS does not have plans to holdtraining specific for the EOB.The Final Contract Year 2013 Medicare Marketing Guidelines 49
General Marketing Questions (Updated)Number Question18. New - What do you do if you comeacross referenced sections that havebeen removed? Example 80.1.32013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseThe reference to 80.1.3 should read 80.3 inthe MMG.19. New - Will templates be provided forFinancial Alignment Demonstrationplans?20. New - On the sales event reportingtemplate, is there a difference betweenthe newly added representative namefield and the event contact field?21. New - Will you be discussing thechanges to the Federal Contractingnumber?22. New - At a minimum, plan sponsorsmust develop scripts that respond toinquiries from prospective and currentenrollees about certain subjects. Pleaseclarify the scope of the following item, isit no longer limited to Part D?Models for certain documents will be releasedfor the FAD plans, now known as MMP(Medicare/Medicaid Plans).The representative field should be the agent'sname which may or may not be the sameindividual as the event contact.Requirements for the Federal ContractingNumber are located in Section 50.1 of theMMG.Plans should be prepared to respond toinquiries on grievance, coveragedeterminations, and appeals for all planbenefits; this includes health and drugbenefits.Old verbiage: How to access the PartD grievance, coverage determination(including exceptions) and appealsprocess*New verbiage: Grievance, coveragedetermination (including exceptions) andappeals process23. New - How long are plans allowed tocontact beneficiaries who haveresponded to Business Reply Cards(BRCs)? The 2012 MMGs stated thatpermission given by a beneficiary to becalled or otherwise contacted (BRCs) isto be considered short-term, eventspecific,and may not be treated asopen-ended permission for futurecontacts. This language is notcontained in the 2013 MMGs.CMS does not define a specified timeframefor BRC contact. Plans should use theguiding principles when determining anappropriate amount of time to honor a BRC.Note that Section 70.6 states permission to becontacted is considered to be event-specificand may not be treated as open-endedpermission for future contact.The Final Contract Year 2013 Medicare Marketing Guidelines 50
General Marketing Questions (Updated)Number Question24. New - Are claim EOBs/notices of denialof payment considered marketingmaterials?2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012ResponseOMB forms are not subject to review persection 20 of the MMG. An EOB for drugs orhealth claims is considered a marketingmaterial.25. New - The EOB appendices were notreceived with the 2013 model. Will 2013appendices be issued or are plans touse the 2012 versions.26. New - What is the RewardsIncentives.pdf? Does the informationthere supplement what is in theMedicare Marketing Guidelines? If so,does this limit the number of activitiesthat can be incentivized?27. New - When will the Enrollment FormGuide be available?28. New - When will CMS release theFinancial Demo Evidence of CoverageModel document?29. New - What member materials qualifyfor file and use opposed to 45 dayreview? If there is no model available?We plan to update the 2012 exhibits in thenear future, but we do not anticipatesignificant changes. The models will beposted on the Part D Model MarketingMaterials webpage at:http://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Part-D-Model-Marketing-Materials.html.The PDF in Section 70.3, Rewards andIncentives, provides resources for the mostcurrent listing of Medicare covered preventiveservices with a zero dollar cost-share. Plansponsors may only provide rewards andincentives for Medicare covered preventiveservices with a zero dollar cost-share.Any updates to the enrollment form will bereleased with the MA and PDPEnrollment/Disenrollment Guidance. CMSissued updated versions of Enrollment andDisenrollment Guidance on Aug 7, 2012.Questions on the FAD/MMP should be sent tothe mmcocapsmodel@cms.hhs.gov mailbox.Plans should use the material code look-upfunction in HPMS to determine whether amaterial is eligible for file & use.The Final Contract Year 2013 Medicare Marketing Guidelines 51
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question1. When will CMS release an update to theHPMS Marketing Module to align with thenew 2013 MMG (e.g., providing SB codesthat qualify for File & Usesubmission)? When a new MarketingModule is released, will CMS notify theindustry, e.g., via HPMS Memo or someother means?2. In HPMS, plans are required to include anorganization marketing name. We havetwo contracts: one includes individualHMO and HMO SNP plans, as well asEGWP HMO plans; and H2411, the otherincludes only EGWP PPO plans. Toaddress the fact that we have differenttypes of HMO plans under one contract,we have entered “Fallon Senior Plan orNaviCare” as our organization marketingname. (For H2411, we have entered“Fallon Senior Plan” as our org. marketingname.) Our HMO and PPO plan namesunder these contracts all start with “FallonSenior Plan” (e.g. H9001: PBP 021 FallonSenior Plan Saver Enhanced Rx HMO,PBP 803 Fallon Senior Plan PremierHMO, and PBP 001 Fallon Senior PlanStandard HMO; H2411: PBP 803 FallonSenior Plan Premier PPO), and our HMOSNP plan is called “NaviCare HMO SNP.”We would like clarification that whenmarketing our family of Fallon Senior Planplans, we are allowed to market and referto them as “Fallon Senior Plan.”3. HPMS does not have an expedited revcode for final populated templates andcorresponding alternate format of finalpopulated. How should plans documentthese?ResponseAs listed in the Call Letter calendar,marketing materials for CY 2013 will beaccepted after June 30, 2012. Therefore,on July 1, 2012, the updated codes for 2013materials will be available. CMS does notintend to issue further guidance on thissubject.You may market your family of plans as“Fallon Senior Plan,” as long as you makethe distinctions when highlighting planfeatures.Codes with corresponding “final expeditedreview” codes are the only ones that qualifyfor standard template submission. Statictemplates should be submitted under thecode that best represents the content of thematerial; there is no submission codespecific for static templates. Plan sponsorsshould consult with their marketingreviewers and/or account managers whenhaving difficulty identifying appropriatesubmission codes.The Final Contract Year 2013 Medicare Marketing Guidelines 52
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question4. Ad-Hoc materials no longer require review.Will the HPMS code for ad-hoc be retired?5. Will someone provide updates to Humanawhen codes are added and/or retired inHPMS?6. What types of materials are to besubmitted under code 1127?7. While you are updating the HPMSsubmission codes, are you also going toupdate the type of submission flags?Some codes have a 45 day review flag butunder file and use" have a status of "yes".8. Where in HPMS is the report showing theFile & Use 10%?9. What is the national producer number foragents?10. The new MMG chapter removed theguidance around the way you submitexplanatory vs. non-explanatory materials,and has not added any information on howto submit prospect vs. member materials.The HPMS Marketing Module and codingdoes not address this change. As anexample, could you please advise us onhow to go about submitting the followingdocument: a plan sponsor creates a directmail (standard) template that containspremium information in a variable textfield? Under the current marketing IDcodes, the plan sponsor would assigncode 4001" to the master template. If theplan sponsor has file & use privilegesshould the plan sponsor request that thestandard template with premiuminformation be reviewed manually?ResponseYes.CMS is currently working on a way to notifyplan sponsors of category and codechanges in HPMS. For now, if newcategories or codes are created, CMS willprovide notice through HPMS.1127 is the Combined ANOC/EOC code.The 45-day review flag means that if File &Use is not selected, the material will receivea 45-day review.In the "Reports" tab within the MarketingModule.The National Producer Number (NPN) isassigned when an agent has registered inthe National Insurance Producer Registry(NIPR).The plan sponsor should not submitadvertisements as templates.Advertisements may be submitted as statictemplates, but benefit information likepremiums and cost-sharing must bedisplayed. When including benefitinformation, the plan sponsor must includethe required disclaimers.The Final Contract Year 2013 Medicare Marketing Guidelines 53
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question11. How do we retire old material in HPMS oris it necessary to do so?12. What is the difference between theAccepted and Approved designation forthe tracking ID?13. When can we upload materials for CMSreview for new contracts that are not yetshowing in HPMS?ResponsePlan sponsors should indicate in HPMS,“No longer in use.”Approved indicates that a material has beenprospectively reviewed and approved byCMS. Accepted indicates that a materialhas been accepted using File & Use andmay be retrospectively reviewed by CMS.Plans that are in a pending status mayupload documents in HPMS.14. What does MCE stand for? Multi-Contract Entity. <strong>It</strong> is used to groupcontract numbers together in the HPMSMarketing Module.15. Regarding 10% Report Drill Functionalityin HPMS - do plans have access to thisreport? If no, can the AM share the reportwith their plan?16. New - Module 1: "Must have completeinformation to make informed decisions"will be helpful to members but will likelyput plans in conflict with the 10% F&Uthreshold as including benefit informationinto material such as directmail/advertising qualifies them as a 45-dayreview. Can CMS elaborate on anyupcoming HPMS Category changes?17. New - What types of materials are to besubmitted under code 1127?Yes. Please refer to the report titled Fileand Use 10% Manual Review in themarketing module of HPMS.HPMS category changes can occur at anytime. Plan sponsors should continue toscrutinize the codes in HPMS to ensurematerials are submitted under theappropriate codes. All advertising, exceptwebsites, are file and use, regardless of anybenefit information included.1127 is the Combined ANOC/EOC code.The Final Contract Year 2013 Medicare Marketing Guidelines 54
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question18. New - When looking at the HPMS Reportfor File & Use 10% Manual Review Reportthe parameters that can be selected areeither the contract year or received daterange or both. In the past, we have lookedat our percentage on a monthly basis toensure the number of file and use versusthe number of 45-day review documentsare both meeting the requirements.However, the reporting capability indicatesthat this percentage may be looked at on arolling annual basis. After reviewing thenew requirements in Chapter 3 Section90.6.1, this section does not indicate atime frame for monitoring the 10%requirement. What we are questioning iscan we monitor this requirement on arolling year basis? Any guidance you canprovide would be helpful.19. New - While you are updating the HPMSsubmission codes, are you also going toupdate the type of submission flags?Some codes have a 45 day review flag butunder file and use" have a status of "yes".20. New - Where in HPMS is the report showsthe File & Use 10%?21. New - What is required for the "NationalProducer Number" in HPMS whensubmitting a marketing/sales event? Ourproducers don`t have a national number.Should I input the state license number?22. New - Does the event type still need to beincluded in the event name?23. New - Is the Representative the plan`sstaff member?24. New - Can you view in HPMS seminarevents submitted under the required 7-daytimeframe?ResponseFrom a monitoring perspective, CMSreviews the data from this report bothmonthly and cumulatively based on contractyear material submissions.Yes. CMS is continually looking at codes toensure they are coded in the systemappropriately.In the "Reports" tab within the MarketingModule.The intent is to have the National InsuranceProducer Registry‟s (NIPR) NationalProducer Number (NPN) placed in the field.If the producer does not have a NPN, plansponsors may enter the state licensenumber or NA.Plans should include one of the followingterms, as appropriate, in the event namefield: "informal", "formal", or "educational".The term representative includes anyonewho is representing the plan, not just a staffmember.Plans can see their events in HPMS,including when they submitted it and theevent date.The Final Contract Year 2013 Medicare Marketing Guidelines 55
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question25. New - The new MMG chapter removed theguidance around the way you submitexplanatory vs. non-explanatory materials,and has not added any information on howto submit prospect vs. member materials.The HPMS Marketing Module and codingdoes not address this change. As anexample, could you please advise us onhow to go about submitting the followingdocument: a plan sponsor creates a directmail (standard) template that containspremium information in a variable textfield? Under the current marketing IDcodes, the plan sponsor would assigncode 4001" to the master template. If theplan sponsor has file & use privilegesshould the plan sponsor request that thestandard template with premiuminformation be reviewed manually?26. New - Is it possible to enter multiplenational producer numbers for a singleevent in HPMS?27. New - How do we retire old material inHPMS or is it necessary to do so?28. New - Will CMS create a star rating modeldocument to be translated into otherformats vs. providing a PDF download onthe HPMS web site that cannot bemodified?29. New - What do we use for status at theend of the material ID code for file and useitems?30. New - Is it possible to provide moreinformation on HPMS memos to showwhether the memo has an action item orjust informational in its purpose?ResponseIn the example provided, the plan maysubmit the direct mail standard templateunder code 4001 as file and use. The directmail populated templates would beuploaded under code 4021.No.Plans may indicate a material is no longerin use by using the Update Materialfunctionality in HPMS. Please refer to theUser Guide for additional instructions.At this time, CMS does not have plans totranslate the star ratings document.Per Section 40.1, plans should use the term"accepted" for file & use materials.CMS will consider this request.The Final Contract Year 2013 Medicare Marketing Guidelines 56
2013 Medicare Marketing Guidelines (MMG)Questions & ResponsesNovember 2, 2012HPMS (Updated)Number Question31. New - What is the difference between theAccepted and Approved designation forthe tracking ID?32. New - When can we upload materials forCMS review for new contracts that are notyet showing in HPMS?ResponseMaterials submitted under the file & useprocess should contain the "accepted"status. Materials submitted for CMS reviewshould contain the "approved" status.Plans must wait for a contract to show inHPMS prior to submitting a material inHPMS for that contract.The Final Contract Year 2013 Medicare Marketing Guidelines 57