The Clinical Side of PFMs - JDT Unbound
The Clinical Side of PFMs - JDT Unbound
The Clinical Side of PFMs - JDT Unbound
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
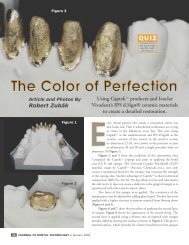
has a unique opportunity to assist hisor her customer in acquiring the skillsneeded for more consistent success.Dr. Charles Goodacre <strong>of</strong> LomaLinda University presented an exhaustivepaper in 2001 that summarized thecrown and bridge literature over thepast 100 years 1 . He found that there isno consensus when comparing margindesigns for best fit and that to attainadequate retention and resistance forma preparation should not exceed 20°degrees <strong>of</strong> taper. He found that axialwall height <strong>of</strong> molars needs to be at least4mm with all others at least 3mm inaxial height.Research by others has shown thatthe greater the taper the greater thechance for seating errors with a correspondingincrease in margin gap 2 .Unfortunately, doctors don’t understandhow difficult it can be for the technicianto manipulate crowns with poor retentionand how that will affect their clinicaloutcome. Of course, today’s cementscan overcome some retention problems,but they will not overcome open marginsfrom mis-seatings.Figure 1In the same report, Goodacre statedthat in order to avoid clinical fracturescrowns veneered with ceramic materialsrequire at least 1mm <strong>of</strong> porcelainover the substrate. That means in mostcases occlusal clearance should be approximately1.5mm. <strong>Clinical</strong>ly, this isnot normally a difficult task. However,we need to keep in mind that there willvery <strong>of</strong>ten be super-eruption beforethe crown is seated and what was onceadequate clearance will no longer be thecase. When working with their doctors,laboratories need to take into considerationwhen examining models that itis possible to loose .5mm <strong>of</strong> clearanceduring temporization.<strong>The</strong> bottom line message tocommunicate to doctors is that 1mm<strong>of</strong> porcelain needs to be present overthe entire occlusal surface after occlusaladjustment. But even before that,the technician should remain cautiouswhen grinding in occlusion during theporcelain stage. I have seen occasionswhen too much porcelain was removedin an occlusal pit or groove, whereby thetechnician unknowingly violated thicknessguidelines.A preparation Catch 22 has beentrying to keep margins supra-gingivalwhile still gaining enough occlusal clearanceand axial height. <strong>The</strong>se requirementscan be mutually exclusive. <strong>The</strong>tendency is to sacrifice axial heightfor the sake <strong>of</strong> clearance or visa versa.Unfortunately, experience and sciencetells us that PFM margins placedsub-gingival in order to accommodatenecessary preparation parameters willvery <strong>of</strong>ten lead to gingival recession,blackened and/or inflamed gums and,possibly, darkened roots. Consequently,doctors using <strong>PFMs</strong> will <strong>of</strong>ten leavemargins supra-gingival and sacrificeretention.Crowns with compromisedretention can be aided by mesial anddistal retentive grooves, metal primerscombined with resin type cements andsometimes air abrasion for metals low inoxides. In cases <strong>of</strong> extremely inadequateaxial height clinicians should considerperiodontal crown lengthening. Failureto follow these guidelines can surely leadto clinical failure.PFM’s have been and remain thestandard for many dentists today. <strong>The</strong>yhave been around the longest (next togold) and have great predictability. <strong>The</strong>yare also less technically demanding thanother types <strong>of</strong> restorations, making themvery easy to use. However, the fact thatthey remain the easiest does not meanthey are without clinical challenges.High-noble <strong>PFMs</strong>, considered theCadillac <strong>of</strong> metal-ceramic restorations,have always produced a more estheticand biocompatible crown than less noblemetals. Why then do many patients stillreact with inflammation and recessionwhen doctors place these crowns?Research published in Europefound that even high-noble crownswithout oxides can be toxic to humanfibroblasts 3 . However, it’s not the goldcausing these problems, but the modifiersin the gold used to develop characteristicsrequired by porcelain, namelyoxide-to-porcelain bonding and metalstrength. Additionally, copper and berylliumcontaining nickel alloys have beenfound to lead to corrosion 4 . Further, thedistortion that can accompany porcelaincontraction <strong>of</strong>ten leads to distortion <strong>of</strong>margins. Research in Germany foundthat <strong>of</strong> 40 high-noble castings fit to astandard die (shoulder-bevel) only fourretained their fit following porcelainapplication 5 . <strong>The</strong> fit discrepancies at themargins <strong>of</strong> <strong>PFMs</strong> very <strong>of</strong>ten result inshort and inadequately sealed marginsand overly tight fits. One researcherfound that the mean margin gap for traditional<strong>PFMs</strong> was 126 microns, meaningsome less and some more 6 . A tight fitwill mean cement has been scraped awayin some areas. Unfortunately, the technicianwill <strong>of</strong>ten not be aware <strong>of</strong> theseproblems (Figure 1). This goes a longFebruary 2007 Journal <strong>of</strong> Dental Technology 49