The Clinical Side of PFMs - JDT Unbound
The Clinical Side of PFMs - JDT Unbound
The Clinical Side of PFMs - JDT Unbound
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
As doctors have becomeincreasingly overloaded withever changing techniquesand materials, they rely moreheavily on their laboratorypartners for guidanceabout materials. MaterialsMastery by Dean Mersky,DDS, is a multi-part seriesthat will help you meet thischallenge by providing youwith the information youneed about materials so youcan more confi dently makerecommendations to yourdentist clients.This series will coverdiverse topics includingmetal-ceramic systems,silica-based and non-silicabasedceramics, cements,adhesives, impressions, tissuemanagement and implants.Mersky will present evidencebasedinformation regardingthe clinical outcomes <strong>of</strong>laboratory materials andtechniques. Additionally,you will gain frank insight intothe clinical world and whathappens to a restoration oncethe doctor receives it from thelaboratory.Each Material Masteryarticle comes with a quiz(download it on <strong>JDT</strong> <strong>Unbound</strong>at www.nadl.org/jdtunbound)that Certifi ed DentalTechnicians can take to earncontinuing education credits.This article is part one in theseries.<strong>The</strong> <strong>Clinical</strong> <strong>Side</strong> <strong>of</strong> <strong>PFMs</strong>here was a time when crowns and bridges were madefrom gold. Form and function were predictable. <strong>The</strong>rewere only two cements to choose from and placing marginssub-gingivally was not a sin. Clearly times have changed!First came <strong>PFMs</strong> and then dozens<strong>of</strong> more technically challenging cements.In the past decade, doctors using thesenewer materials have been advised tokeep margins supra-gingival and prepwith a more conservative nature, whileremaining acutely concerned withesthetics. If there was ever a Catch 22 forthe laboratory technician, this is it.In this article we will explore thechallenges posed by <strong>PFMs</strong> and the clinicaloutcomes that <strong>of</strong>ten are unseen bythe laboratory technician. We will focuson the two most widely used: traditionalcast alloys and the non-cast compositemetal, Captek.For decades, <strong>PFMs</strong> have served asthe standard esthetic dental restoration.And, despite the limitations, they did aDean Mersky, DDSgood job. Even though all-ceramics havemade in-roads, the PFM still remainsthe mainstay <strong>of</strong> most dental practices.Unlike all-ceramics, they can be usedwith any cement, any margin design that(subject to debate) can be placed supraorsub-gingival and <strong>of</strong>fer a lot <strong>of</strong> latitudefor abuse. In short, despite its shortcomings,the traditional PFM makes life forthe dentist a whole lot easier.<strong>The</strong> dental technician sees preparationguidelines violated everyday. Sometoo short, some too tapered, not enoughreduction and combinations <strong>of</strong> all three.Applied skills and practical knowledgeare <strong>of</strong>ten insufficient in bringing a completeunderstanding to the management<strong>of</strong> materials <strong>of</strong>fered by the dental laboratory.<strong>The</strong> dental laboratory technician48 Journal <strong>of</strong> Dental Technology February 2007
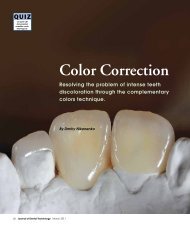
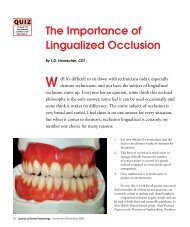
has a unique opportunity to assist hisor her customer in acquiring the skillsneeded for more consistent success.Dr. Charles Goodacre <strong>of</strong> LomaLinda University presented an exhaustivepaper in 2001 that summarized thecrown and bridge literature over thepast 100 years 1 . He found that there isno consensus when comparing margindesigns for best fit and that to attainadequate retention and resistance forma preparation should not exceed 20°degrees <strong>of</strong> taper. He found that axialwall height <strong>of</strong> molars needs to be at least4mm with all others at least 3mm inaxial height.Research by others has shown thatthe greater the taper the greater thechance for seating errors with a correspondingincrease in margin gap 2 .Unfortunately, doctors don’t understandhow difficult it can be for the technicianto manipulate crowns with poor retentionand how that will affect their clinicaloutcome. Of course, today’s cementscan overcome some retention problems,but they will not overcome open marginsfrom mis-seatings.Figure 1In the same report, Goodacre statedthat in order to avoid clinical fracturescrowns veneered with ceramic materialsrequire at least 1mm <strong>of</strong> porcelainover the substrate. That means in mostcases occlusal clearance should be approximately1.5mm. <strong>Clinical</strong>ly, this isnot normally a difficult task. However,we need to keep in mind that there willvery <strong>of</strong>ten be super-eruption beforethe crown is seated and what was onceadequate clearance will no longer be thecase. When working with their doctors,laboratories need to take into considerationwhen examining models that itis possible to loose .5mm <strong>of</strong> clearanceduring temporization.<strong>The</strong> bottom line message tocommunicate to doctors is that 1mm<strong>of</strong> porcelain needs to be present overthe entire occlusal surface after occlusaladjustment. But even before that,the technician should remain cautiouswhen grinding in occlusion during theporcelain stage. I have seen occasionswhen too much porcelain was removedin an occlusal pit or groove, whereby thetechnician unknowingly violated thicknessguidelines.A preparation Catch 22 has beentrying to keep margins supra-gingivalwhile still gaining enough occlusal clearanceand axial height. <strong>The</strong>se requirementscan be mutually exclusive. <strong>The</strong>tendency is to sacrifice axial heightfor the sake <strong>of</strong> clearance or visa versa.Unfortunately, experience and sciencetells us that PFM margins placedsub-gingival in order to accommodatenecessary preparation parameters willvery <strong>of</strong>ten lead to gingival recession,blackened and/or inflamed gums and,possibly, darkened roots. Consequently,doctors using <strong>PFMs</strong> will <strong>of</strong>ten leavemargins supra-gingival and sacrificeretention.Crowns with compromisedretention can be aided by mesial anddistal retentive grooves, metal primerscombined with resin type cements andsometimes air abrasion for metals low inoxides. In cases <strong>of</strong> extremely inadequateaxial height clinicians should considerperiodontal crown lengthening. Failureto follow these guidelines can surely leadto clinical failure.PFM’s have been and remain thestandard for many dentists today. <strong>The</strong>yhave been around the longest (next togold) and have great predictability. <strong>The</strong>yare also less technically demanding thanother types <strong>of</strong> restorations, making themvery easy to use. However, the fact thatthey remain the easiest does not meanthey are without clinical challenges.High-noble <strong>PFMs</strong>, considered theCadillac <strong>of</strong> metal-ceramic restorations,have always produced a more estheticand biocompatible crown than less noblemetals. Why then do many patients stillreact with inflammation and recessionwhen doctors place these crowns?Research published in Europefound that even high-noble crownswithout oxides can be toxic to humanfibroblasts 3 . However, it’s not the goldcausing these problems, but the modifiersin the gold used to develop characteristicsrequired by porcelain, namelyoxide-to-porcelain bonding and metalstrength. Additionally, copper and berylliumcontaining nickel alloys have beenfound to lead to corrosion 4 . Further, thedistortion that can accompany porcelaincontraction <strong>of</strong>ten leads to distortion <strong>of</strong>margins. Research in Germany foundthat <strong>of</strong> 40 high-noble castings fit to astandard die (shoulder-bevel) only fourretained their fit following porcelainapplication 5 . <strong>The</strong> fit discrepancies at themargins <strong>of</strong> <strong>PFMs</strong> very <strong>of</strong>ten result inshort and inadequately sealed marginsand overly tight fits. One researcherfound that the mean margin gap for traditional<strong>PFMs</strong> was 126 microns, meaningsome less and some more 6 . A tight fitwill mean cement has been scraped awayin some areas. Unfortunately, the technicianwill <strong>of</strong>ten not be aware <strong>of</strong> theseproblems (Figure 1). This goes a longFebruary 2007 Journal <strong>of</strong> Dental Technology 49
way to explain why cast <strong>PFMs</strong> are <strong>of</strong>tentimes associated with recession, inflammationand plaque retention, and why4 percent have been reported to lead tolichinoid type lesions 7 .Captek, though technically a porcelain-fused-to-metaltype restoration,is hand-formed from a wax sheet and isfundamentally different than cast alloysystems. It is comprised <strong>of</strong> pure particles<strong>of</strong> platinum, palladium, gold and a traceamount <strong>of</strong> silver. It has no modifiers tocreate hardness or oxides. <strong>The</strong> platinumand palladium is used to create neededstrength and serve as major components<strong>of</strong> the external porcelain-bondingsurface.<strong>The</strong> external bonding surfaceprovides porcelain bond strength inexcess <strong>of</strong> most all other crown andbridge systems, with shear strengths <strong>of</strong>approximately 56 mpa 8 . Additionally, byeliminating oxides and corrosive factorsusers report an improvement in estheticsover traditional cast <strong>PFMs</strong>.Perhaps one <strong>of</strong> its most importantcharacteristics is plaque inhibition. Dr.Max Goodson reported that Captekrestored teeth accumulated at least71 percent less bacterial plaque thannon-restored teeth in the same mouth 9 .Doctors using Captek <strong>of</strong>ten commentthat the gums surrounding the crownsand bridges don’t recede and lookhealthier than other areas <strong>of</strong> the mouth.But like all materials, if not managedproperly there will be challenges.Although the porcelain shear strengthis greater than most all other <strong>PFMs</strong> itscompressive strength is not. At times,doctors will press the limit with regardsto obtaining adequate occlusal reduction.Doctors need to be advised thattotal occlusal thickness must be maintainedat 1.5mm minimally. This meansreduction should be approximately 2mmto compensate for possible super-eruptionduring temporization.50 Journal <strong>of</strong> Dental Technology February 2007Doctors will also need your adviceon cementation. Captek has margingaps smaller than most any other material.At 15 microns, the gap is smallerthan many cements 10 . Zinc phosphate,carboxylate, glass ionomer (includingresin modified varieties) all have appropriatefilm thickness. Resins can alsobe used even though most are thickerthan the margin gap. However, manyresins require an adhesive and in combinationmay open the margin beyondwhat many doctors will accept. Also,advise your doctors that when retentionis compromised it would be wiseto air abrade the inside <strong>of</strong> the copingwith 50 micron aluminum oxide at 40pounds <strong>of</strong> pressure. According to studiesat UCLA and the University <strong>of</strong> Oregonthis will increase mechanical retention<strong>of</strong> the cement to the crown 5-20 times.Additionally, this very small opening atthe margin means that the doctor shouldonly line the inside <strong>of</strong> the crown (notfill it), and seat it slowly in order to helpexpress the excess cement more easily.Used successfully for decades,<strong>PFMs</strong> clearly provide predictability andfamiliarity for the dentist. Newer materialsbring improved qualities but also mayrequire closer attention to details. Still,even with the advent <strong>of</strong> all-ceramics, the<strong>PFMs</strong> familiarity and ease <strong>of</strong> use willhelp them to remain the restoration <strong>of</strong>choice for many.About the AuthorMersky is thedirector <strong>of</strong> clinicalcommunications forthe Captek Co.Mersky graduatedfrom the University <strong>of</strong>Detroit in 1976 andpracticed dentistry inManhattan Beach, Calif., for 26 years.He interacts nationally with laboratoriesand doctors on a variety <strong>of</strong> subjects fromclinical topics to business principals.References1 Goodacre, DDS, MSD,Campagne, DMD, Aquilino, DDS, MS:Tooth preparations for complete crowns:An art form based on scientific principles.J <strong>of</strong> Prosth Dent 2001, 85:363-3762 Chan, Willson, JR, Barbe,Cronin, Jr, C. Chung & K. Chung:Effect <strong>of</strong> preparation convergence onretention and seating discrepancy <strong>of</strong>complete veneer crowns. J <strong>of</strong> OralRehabilitation 2005, 32:583 Schmalz, Arenholt, hiller,Schwikl: An Investigation <strong>of</strong> theCytotoxic effects <strong>of</strong> Dental CastingAlloys. European J or Oral Science1997, 105(1):86-914 B. I. Johansson, L. C. Lucas, J.E. Lemons: Corrosion <strong>of</strong> copper, nickel,and gold dental casting alloys: An invitro and in vivo study. J BiomedicalMaterials Research 2004, 23(14):349-3615 Biffar, Krapp: Deformation <strong>of</strong>crowns by porcelain fusion. ZWR 1990,99(9):694-66 Ferrari, Mason, Poli, Dente:Marginal adaptation <strong>of</strong> crowns: SEMinvestigation, International Journal OfPeriodontics and Restorative Dentistry1994 Jun; 14(3):272-97 Larsson A, Warfvinge G: <strong>The</strong>histopathology <strong>of</strong> oral mucosal lesionsassociated with amalgam or porcelainfused-to-metalrestorations. Oral Disease1995, 1(3):152-88,10 Nathanson, Giordano,Juntavee, IADR, 19959 Goodson, Shoher, Imber, Som,Nathanson: Reduced dental plaque accumulationon composite gold alloy margins.Jrnl Periodontal Research 2001, 36:252-259