First Quarter 2008 - Issues in Hematology - ION Solutions
First Quarter 2008 - Issues in Hematology - ION Solutions
First Quarter 2008 - Issues in Hematology - ION Solutions
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
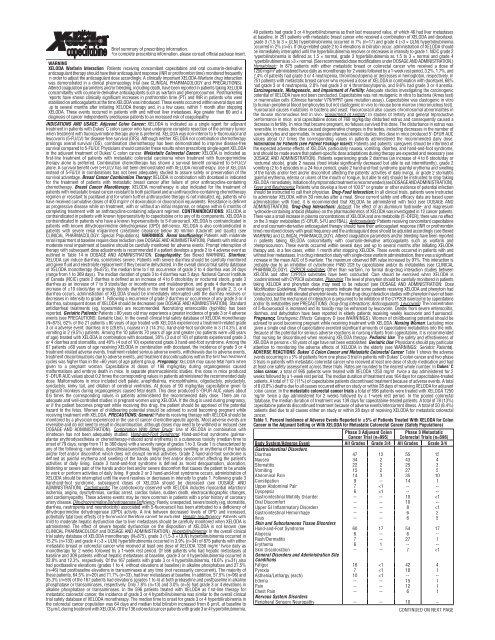
Brief summary of prescrib<strong>in</strong>g <strong>in</strong>formation.For complete prescrib<strong>in</strong>g <strong>in</strong>formation, please consult official package <strong>in</strong>sert.WARNINGXELODA Warfar<strong>in</strong> Interaction: Patients receiv<strong>in</strong>g concomitant capecitab<strong>in</strong>e and oral coumar<strong>in</strong>-derivativeanticoagulant therapy should have their anticoagulant response (INR or prothromb<strong>in</strong> time) monitored frequently<strong>in</strong> order to adjust the anticoagulant dose accord<strong>in</strong>gly. A cl<strong>in</strong>ically important XELODA-Warfar<strong>in</strong> drug <strong>in</strong>teractionwas demonstrated <strong>in</strong> a cl<strong>in</strong>ical pharmacology trial (see CLINICAL PHARMACOLOGY and PRECAUT<strong>ION</strong>S).Altered coagulation parameters and/or bleed<strong>in</strong>g, <strong>in</strong>clud<strong>in</strong>g death, have been reported <strong>in</strong> patients tak<strong>in</strong>g XELODAconcomitantly with coumar<strong>in</strong>-derivative anticoagulants such as warfar<strong>in</strong> and phenprocoumon. Postmarket<strong>in</strong>greports have shown cl<strong>in</strong>ically significant <strong>in</strong>creases <strong>in</strong> prothromb<strong>in</strong> time (PT) and INR <strong>in</strong> patients who werestabilized on anticoagulants at the time XELODA was <strong>in</strong>troduced. These events occurred with<strong>in</strong> several days andup to several months after <strong>in</strong>itiat<strong>in</strong>g XELODA therapy and, <strong>in</strong> a few cases, with<strong>in</strong> 1 month after stopp<strong>in</strong>gXELODA. These events occurred <strong>in</strong> patients with and without liver metastases. Age greater than 60 and adiagnosis of cancer <strong>in</strong>dependently predispose patients to an <strong>in</strong>creased risk of coagulopathy.INDICAT<strong>ION</strong>S AND USAGE: Adjuvant Colon Cancer:XELODA is <strong>in</strong>dicated as a s<strong>in</strong>gle agent for adjuvanttreatment <strong>in</strong> patients with Dukes’ C colon cancer who have undergone complete resection of the primary tumorwhen treatment with fluoropyrimid<strong>in</strong>e therapy alone is preferred. XELODA was non-<strong>in</strong>ferior to 5-fluorouracil andleucovor<strong>in</strong> (5-FU/LV) for disease-free survival (DFS). Although neither XELODA nor comb<strong>in</strong>ation chemotherapyprolongs overall survival (OS), comb<strong>in</strong>ation chemotherapy has been demonstrated to improve disease-freesurvival compared to 5-FU/LV. Physicians should consider these results when prescrib<strong>in</strong>g s<strong>in</strong>gle-agent XELODA<strong>in</strong> the adjuvant treatment of Dukes’ C colon cancer. Metastatic Colorectal Cancer:XELODA is <strong>in</strong>dicated asfirst-l<strong>in</strong>e treatment of patients with metastatic colorectal carc<strong>in</strong>oma when treatment with fluoropyrimid<strong>in</strong>etherapy alone is preferred. Comb<strong>in</strong>ation chemotherapy has shown a survival benefit compared to 5-FU/LValone. A survival benefit over 5-FU/LV has not been demonstrated with XELODA monotherapy. Use of XELODA<strong>in</strong>stead of 5-FU/LV <strong>in</strong> comb<strong>in</strong>ations has not been adequately studied to assure safety or preservation of thesurvival advantage. Breast Cancer Comb<strong>in</strong>ation Therapy:XELODA <strong>in</strong> comb<strong>in</strong>ation with docetaxel is <strong>in</strong>dicatedfor the treatment of patients with metastatic breast cancer after failure of prior anthracycl<strong>in</strong>e-conta<strong>in</strong><strong>in</strong>gchemotherapy. Breast Cancer Monotherapy: XELODA monotherapy is also <strong>in</strong>dicated for the treatment ofpatients with metastatic breast cancer resistant to both paclitaxel and an anthracycl<strong>in</strong>e-conta<strong>in</strong><strong>in</strong>g chemotherapyregimen or resistant to paclitaxel and for whom further anthracycl<strong>in</strong>e therapy is not <strong>in</strong>dicated, eg, patients whohave received cumulative doses of 400 mg/m 2 of doxorubic<strong>in</strong> or doxorubic<strong>in</strong> equivalents. Resistance is def<strong>in</strong>edas progressive disease while on treatment, with or without an <strong>in</strong>itial response, or relapse with<strong>in</strong> 6 months ofcomplet<strong>in</strong>g treatment with an anthracycl<strong>in</strong>e-conta<strong>in</strong><strong>in</strong>g adjuvant regimen. CONTRAINDICAT<strong>ION</strong>S: XELODA iscontra<strong>in</strong>dicated <strong>in</strong> patients with known hypersensitivity to capecitab<strong>in</strong>e or to any of its components. XELODA iscontra<strong>in</strong>dicated <strong>in</strong> patients who have a known hypersensitivity to 5-fluorouracil. XELODA is contra<strong>in</strong>dicated <strong>in</strong>patients with known dihydropyrimid<strong>in</strong>e dehydrogenase (DPD) deficiency. XELODA is also contra<strong>in</strong>dicated <strong>in</strong>patients with severe renal impairment (creat<strong>in</strong><strong>in</strong>e clearance below 30 ml/m<strong>in</strong> [Cockroft and Gault]) (seeCLINICAL PHARMACOLOGY: Special Populations). WARNINGS: Renal Insufficiency:Patients with moderaterenal impairment at basel<strong>in</strong>e require dose reduction (see DOSAGE AND ADMINISTRAT<strong>ION</strong>). Patients with mild andmoderate renal impairment at basel<strong>in</strong>e should be carefully monitored for adverse events. Prompt <strong>in</strong>terruption oftherapy with subsequent dose adjustments is recommended if a patient develops a grade 2 to 4 adverse event asoutl<strong>in</strong>ed <strong>in</strong> Table 14 <strong>in</strong> DOSAGE AND ADMINISTRAT<strong>ION</strong>. Coagulopathy:See Boxed WARNING. Diarrhea:XELODA can <strong>in</strong>duce diarrhea, sometimes severe. Patients with severe diarrhea should be carefully monitoredand given fluid and electrolyte replacement if they become dehydrated. In the overall cl<strong>in</strong>ical trial safety databaseof XELODA monotherapy (N=875), the median time to first occurrence of grade 2 to 4 diarrhea was 34 days(range from 1 to 369 days). The median duration of grade 3 to 4 diarrhea was 5 days. National Cancer Instituteof Canada (NCIC) grade 2 diarrhea is def<strong>in</strong>ed as an <strong>in</strong>crease of 4 to 6 stools/day or nocturnal stools, grade 3diarrhea as an <strong>in</strong>crease of 7 to 9 stools/day or <strong>in</strong>cont<strong>in</strong>ence and malabsorption, and grade 4 diarrhea as an<strong>in</strong>crease of ≥10 stools/day or grossly bloody diarrhea or the need for parenteral support. If grade 2, 3, or 4diarrhea occurs, adm<strong>in</strong>istration of XELODA should be immediately <strong>in</strong>terrupted until the diarrhea resolves ordecreases <strong>in</strong> <strong>in</strong>tensity to grade 1. Follow<strong>in</strong>g a recurrence of grade 2 diarrhea or occurrence of any grade 3 or 4diarrhea, subsequent doses of XELODA should be decreased (see DOSAGE AND ADMINISTRAT<strong>ION</strong>). Standardantidiarrheal treatments (eg, loperamide) are recommended. Necrotiz<strong>in</strong>g enterocolitis (typhlitis) has beenreported. Geriatric Patients:Patients ≥80 years old may experience a greater <strong>in</strong>cidence of grade 3 or 4 adverseevents (see PRECAUT<strong>ION</strong>S: Geriatric Use). In the overall cl<strong>in</strong>ical trial safety database of XELODA monotherapy(N=875), 62% of the 21 patients ≥80 years of age treated with XELODA experienced a treatment-related grade3 or 4 adverse event: diarrhea <strong>in</strong> 6 (28.6%), nausea <strong>in</strong> 3 (14.3%), hand-and-foot syndrome <strong>in</strong> 3 (14.3%), andvomit<strong>in</strong>g <strong>in</strong> 2 (9.5%) patients. Among the 10 patients 70 years of age and greater (no patients were >80 yearsof age) treated with XELODA <strong>in</strong> comb<strong>in</strong>ation with docetaxel, 30% (3 out of 10) of patients experienced grade 3or 4 diarrhea and stomatitis, and 40% (4 out of 10) experienced grade 3 hand-and-foot syndrome. Among the67 patients ≥60 years of age receiv<strong>in</strong>g XELODA <strong>in</strong> comb<strong>in</strong>ation with docetaxel, the <strong>in</strong>cidence of grade 3 or 4treatment-related adverse events, treatment-related serious adverse events, withdrawals due to adverse events,treatment discont<strong>in</strong>uations due to adverse events, and treatment discont<strong>in</strong>uations with<strong>in</strong> the first two treatmentcycles was higher than <strong>in</strong> the 3 × ULN) hyperbilirub<strong>in</strong>emia occurred <strong>in</strong> 3.9% (n=34) of 875 patients with eithermetastatic breast or colorectal cancer who received at least one dose of XELODA 1250 mg/m 2 twice daily asmonotherapy for 2 weeks followed by a 1-week rest period. Of 566 patients who had hepatic metastases atbasel<strong>in</strong>e and 309 patients without hepatic metastases at basel<strong>in</strong>e, grade 3 or 4 hyperbilirub<strong>in</strong>emia occurred <strong>in</strong>22.8% and 12.3%, respectively. Of the 167 patients with grade 3 or 4 hyperbilirub<strong>in</strong>emia, 18.6% (n=31) alsohad postbasel<strong>in</strong>e elevations (grades 1 to 4, without elevations at basel<strong>in</strong>e) <strong>in</strong> alkal<strong>in</strong>e phosphatase and 27.5%(n=46) had postbasel<strong>in</strong>e elevations <strong>in</strong> transam<strong>in</strong>ases at any time (not necessarily concurrent). The majority ofthese patients, 64.5% (n=20) and 71.7% (n=33), had liver metastases at basel<strong>in</strong>e. In addition, 57.5% (n=96) and35.3% (n=59) of the 167 patients had elevations (grades 1 to 4) at both prebasel<strong>in</strong>e and postbasel<strong>in</strong>e <strong>in</strong> alkal<strong>in</strong>ephosphatase or transam<strong>in</strong>ases, respectively. Only 7.8% (n=13) and 3.0% (n=5) had grade 3 or 4 elevations <strong>in</strong>alkal<strong>in</strong>e phosphatase or transam<strong>in</strong>ases. In the 596 patients treated with XELODA as first-l<strong>in</strong>e therapy formetastatic colorectal cancer, the <strong>in</strong>cidence of grade 3 or 4 hyperbilirub<strong>in</strong>emia was similar to the overall cl<strong>in</strong>icaltrial safety database of XELODA monotherapy. The median time to onset for grade 3 or 4 hyperbilirub<strong>in</strong>emia <strong>in</strong>the colorectal cancer population was 64 days and median total bilirub<strong>in</strong> <strong>in</strong>creased from 8 µm/L at basel<strong>in</strong>e to13 µm/L dur<strong>in</strong>g treatment with XELODA. Of the 136 colorectal cancer patients with grade 3 or 4 hyperbilirub<strong>in</strong>emia,49 patients had grade 3 or 4 hyperbilirub<strong>in</strong>emia as their last measured value, of which 46 had liver metastasesat basel<strong>in</strong>e. In 251 patients with metastatic breast cancer who received a comb<strong>in</strong>ation of XELODA and docetaxel,grade 3 (1.5 to 3 × ULN) hyperbilirub<strong>in</strong>emia occurred <strong>in</strong> 7% (n=17) and grade 4 (>3 × ULN) hyperbilirub<strong>in</strong>emiaoccurred <strong>in</strong> 2% (n=5). If drug-related grade 2 to 4 elevations <strong>in</strong> bilirub<strong>in</strong> occur, adm<strong>in</strong>istration of XELODA shouldbe immediately <strong>in</strong>terrupted until the hyperbilirub<strong>in</strong>emia resolves or decreases <strong>in</strong> <strong>in</strong>tensity to grade 1. NCIC grade 2hyperbilirub<strong>in</strong>emia is def<strong>in</strong>ed as 1.5 × normal, grade 3 hyperbilirub<strong>in</strong>emia as 1.5 to 3 × normal and grade 4hyperbilirub<strong>in</strong>emia as >3 × normal. (See recommended dose modifications under DOSAGE AND ADMINISTRAT<strong>ION</strong>.)Hematologic: In 875 patients with either metastatic breast or colorectal cancer who received a dose of1250 mg/m 2 adm<strong>in</strong>istered twice daily as monotherapy for 2 weeks followed by a 1-week rest period, 3.2%, 1.7%, and2.4% of patients had grade 3 or 4 neutropenia, thrombocytopenia or decreases <strong>in</strong> hemoglob<strong>in</strong>, respectively. In251 patients with metastatic breast cancer who received a dose of XELODA <strong>in</strong> comb<strong>in</strong>ation with docetaxel, 68%had grade 3 or 4 neutropenia, 2.8% had grade 3 or 4 thrombocytopenia, and 9.6% had grade 3 or 4 anemia.Carc<strong>in</strong>ogenesis, Mutagenesis, and Impairment of Fertility:Adequate studies <strong>in</strong>vestigat<strong>in</strong>g the carc<strong>in</strong>ogenicpotential of XELODA have not been conducted. Capecitab<strong>in</strong>e was not mutagenic <strong>in</strong> vitro to bacteria (Ames test)or mammalian cells (Ch<strong>in</strong>ese hamster V79/HPRT gene mutation assay). Capecitab<strong>in</strong>e was clastogenic <strong>in</strong> vitroto human peripheral blood lymphocytes but not clastogenic <strong>in</strong> vivo to mouse bone marrow (micronucleus test).Fluorouracil causes mutations <strong>in</strong> bacteria and yeast. Fluourouracil also causes chromosomal abnormalities <strong>in</strong>the mouse micronucleus test <strong>in</strong> vivo. Impairment of Fertility:In studies of fertility and general reproductiveperformance <strong>in</strong> mice, oral capecitab<strong>in</strong>e doses of 760 mg/kg/day disturbed estrus and consequently caused adecrease <strong>in</strong> fertility. In mice that became pregnant, no fetuses survived this dose. The disturbance <strong>in</strong> estrus wasreversible. In males, this dose caused degenerative changes <strong>in</strong> the testes, <strong>in</strong>clud<strong>in</strong>g decreases <strong>in</strong> the number ofspermatocytes and spermatids. In separate pharmacok<strong>in</strong>etic studies, this dose <strong>in</strong> mice produced 5'-DFUR AUCvalues about 0.7 times the correspond<strong>in</strong>g values <strong>in</strong> patients adm<strong>in</strong>istered the recommended daily dose.Information for Patients (see Patient Package Insert):Patients and patients’ caregivers should be <strong>in</strong>formed ofthe expected adverse effects of XELODA, particularly nausea, vomit<strong>in</strong>g, diarrhea, and hand-and-foot syndrome,and should be made aware that patient-specific dose adaptations dur<strong>in</strong>g therapy are expected and necessary (seeDOSAGE AND ADMINISTRAT<strong>ION</strong>). Patients experienc<strong>in</strong>g grade 2 diarrhea (an <strong>in</strong>crease of 4 to 6 stools/day ornocturnal stools), grade 2 nausea (food <strong>in</strong>take significantly decreased but able to eat <strong>in</strong>termittently), grade 2vomit<strong>in</strong>g (2 to 5 episodes <strong>in</strong> a 24-hour period), grade 2 hand-and-foot syndrome (pa<strong>in</strong>ful erythema and swell<strong>in</strong>gof the hands and/or feet and/or discomfort affect<strong>in</strong>g the patients’ activities of daily liv<strong>in</strong>g), or grade 2 stomatitis(pa<strong>in</strong>ful erythema, edema or ulcers of the mouth or tongue, but able to eat) should be <strong>in</strong>structed to stop tak<strong>in</strong>gXELODAimmediately. Initiation of symptomatic treatment is recommended (see DOSAGE AND ADMINISTRAT<strong>ION</strong>).Fever and Neutropenia:Patients who develop a fever of 100.5° or greater or other evidence of potential <strong>in</strong>fectionshould be <strong>in</strong>structed to call their physician. Drug-Food Interaction:In all cl<strong>in</strong>ical trials, patients were <strong>in</strong>structedto adm<strong>in</strong>ister XELODA with<strong>in</strong> 30 m<strong>in</strong>utes after a meal. S<strong>in</strong>ce current safety and efficacy data are based uponadm<strong>in</strong>istration with food, it is recommended that XELODA be adm<strong>in</strong>istered with food (see DOSAGE ANDADMINISTRAT<strong>ION</strong>). Drug-Drug Interactions: Antacid: The effect of an alum<strong>in</strong>um hydroxide- and magnesiumhydroxide-conta<strong>in</strong><strong>in</strong>g antacid (Maalox) on the pharmacok<strong>in</strong>etics of XELODA was <strong>in</strong>vestigated <strong>in</strong> 12 cancer patients.There was a small <strong>in</strong>crease <strong>in</strong> plasma concentrations of XELODA and one metabolite (5'-DFCR); there was no effecton the 3 major metabolites (5'-DFUR, 5-FU and FBAL). Anticoagulants:Patients receiv<strong>in</strong>g concomitant capecitab<strong>in</strong>eand oral coumar<strong>in</strong>-derivative anticoagulant therapy should have their anticoagulant response (INR or prothromb<strong>in</strong>time) monitored closely with great frequency and the anticoagulant dose should be adjusted accord<strong>in</strong>gly (see BoxedWARNING and CLINICAL PHARMACOLOGY). Altered coagulation parameters and/or bleed<strong>in</strong>g have been reported<strong>in</strong> patients tak<strong>in</strong>g XELODA concomitantly with coumar<strong>in</strong>-derivative anticoagulants such as warfar<strong>in</strong> andphenprocoumon. These events occurred with<strong>in</strong> several days and up to several months after <strong>in</strong>itiat<strong>in</strong>g XELODAtherapy and, <strong>in</strong> a few cases, with<strong>in</strong> 1 month after stopp<strong>in</strong>g XELODA. These events occurred <strong>in</strong> patients with andwithout liver metastases. In a drug <strong>in</strong>teraction study with s<strong>in</strong>gle-dose warfar<strong>in</strong> adm<strong>in</strong>istration, there was a significant<strong>in</strong>crease <strong>in</strong> the mean AUC of S-warfar<strong>in</strong>. The maximum observed INR value <strong>in</strong>creased by 91%. This <strong>in</strong>teraction isprobably due to an <strong>in</strong>hibition of cytochrome P450 2C9 by capecitab<strong>in</strong>e and/or its metabolites (see CLINICALPHARMACOLOGY). CYP2C9 substrates: Other than warfar<strong>in</strong>, no formal drug-drug <strong>in</strong>teraction studies betweenXELODA and other CYP2C9 substrates have been conducted. Care should be exercised when XELODA iscoadm<strong>in</strong>istered with CYP2C9 substrates. Phenyto<strong>in</strong>: The level of phenyto<strong>in</strong> should be carefully monitored <strong>in</strong> patientstak<strong>in</strong>g XELODA and phenyto<strong>in</strong> dose may need to be reduced (see DOSAGE AND ADMINISTRAT<strong>ION</strong>: DoseModification Guidel<strong>in</strong>es). Postmarket<strong>in</strong>g reports <strong>in</strong>dicate that some patients receiv<strong>in</strong>g XELODA and phenyto<strong>in</strong> hadtoxicity associated with elevated phenyto<strong>in</strong> levels. Formal drug-drug <strong>in</strong>teraction studies with phenyto<strong>in</strong> have not beenconducted, but the mechanism of <strong>in</strong>teraction is presumed to be <strong>in</strong>hibition of the CYP2C9 isoenzyme by capecitab<strong>in</strong>eand/or its metabolites (see PRECAUT<strong>ION</strong>S: Drug-Drug Interactions: Anticoagulants).Leucovor<strong>in</strong>: The concentrationof 5-fluourouracil is <strong>in</strong>creased and its toxicity may be enhanced by leucovor<strong>in</strong>. Deaths from severe enterocolitis,diarrhea, and dehydration have been reported <strong>in</strong> elderly patients receiv<strong>in</strong>g weekly leucovor<strong>in</strong> and fluorouracil.Pregnancy:Teratogenic Effects: Category D (see WARNINGS). Women of childbear<strong>in</strong>g potential should beadvised to avoid becom<strong>in</strong>g pregnant while receiv<strong>in</strong>g treatment with XELODA. Nurs<strong>in</strong>g Women: Lactat<strong>in</strong>g micegiven a s<strong>in</strong>gle oral dose of capecitab<strong>in</strong>e excreted significant amounts of capecitab<strong>in</strong>e metabolites <strong>in</strong>to the milk.Because of the potential for serious adverse reactions <strong>in</strong> nurs<strong>in</strong>g <strong>in</strong>fants from capecitab<strong>in</strong>e, it is recommendedthat nurs<strong>in</strong>g be discont<strong>in</strong>ued when receiv<strong>in</strong>g XELODA therapy. Pediatric Use: The safety and effectiveness ofXELODA <strong>in</strong> persons