You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
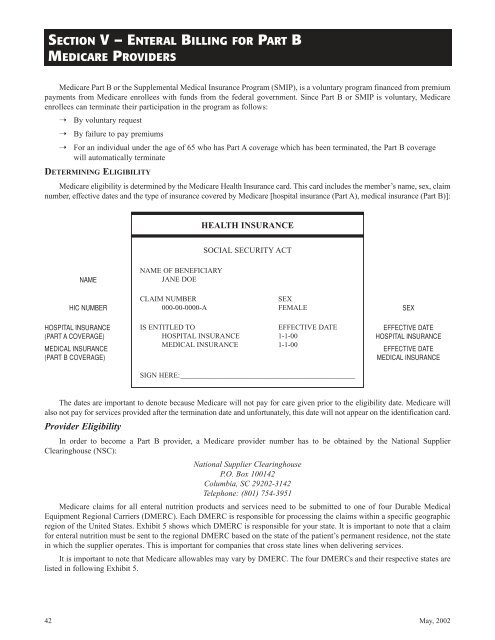
SECTION V – ENTERAL BILLING FOR PART BMEDICARE PROVIDERSMedicare Part B or the Supplemental Medical Insurance Program (SMIP), is a voluntary program financed from premiumpayments from Medicare enrollees with funds from the federal government. Since Part B or SMIP is voluntary, Medicareenrollees can terminate their participation in the program as follows:➝ By voluntary request➝ By failure to pay premiums➝For an individual under the age of 65 who has Part A coverage which has been terminated, the Part B coveragewill automatically terminateDETERMINING ELIGIBILITYMedicare eligibility is determined <strong>by</strong> the Medicare Health Insurance card. This card includes the member’s name, sex, claimnumber, effective dates and the type of insurance covered <strong>by</strong> Medicare [hospital insurance (Part A), medical insurance (Part B)]:HEALTH INSURANCESOCIAL SECURITY ACTNAMENAME OF BENEFICIARYJANE DOEHIC NUMBERCLAIM NUMBER000-00-0000-ASEXFEMALESEXHOSPITAL INSURANCE(PART A COVERAGE)MEDICAL INSURANCE(PART B COVERAGE)IS ENTITLED TOEFFECTIVE DATEHOSPITAL INSURANCE 1-1-00MEDICAL INSURANCE 1-1-00SIGN HERE:________________________________________________EFFECTIVE DATEHOSPITAL INSURANCEEFFECTIVE DATEMEDICAL INSURANCEThe dates are important to denote because Medicare will not pay for care given prior to the eligibility date. Medicare willalso not pay for services provided after the termination date and unfortunately, this date will not appear on the identification card.Provider EligibilityIn order to become a Part B provider, a Medicare provider number has to be obtained <strong>by</strong> the National SupplierClearinghouse (NSC):National Supplier ClearinghouseP.O. Box 100142Columbia, SC 29202-3142Telephone: (801) 754-3951Medicare claims for all enteral nutrition products and services need to be submitted to one of four Durable MedicalEquipment Regional Carriers (DMERC). Each DMERC is responsible for processing the claims within a specific geographicregion of the United States. Exhibit 5 shows which DMERC is responsible for your state. It is important to note that a claimfor enteral nutrition must be sent to the regional DMERC based on the state of the patient’s permanent residence, not the statein which the supplier operates. This is important for companies that cross state lines when delivering services.It is important to note that Medicare allowables may vary <strong>by</strong> DMERC. The four DMERCs and their respective states arelisted in following Exhibit 5.42May, 2002