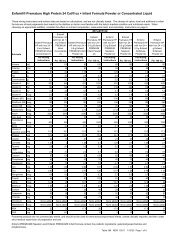
EXHIBIT 17 - METHODS OF ESTABLISHING CAPITATION RATESMethodPercentage of PremiumFlat PMPMGuaranteed RatesVariable Rates Based onDemographic DataRate$100 premium per month x 3% = $3 PMPM$3 PMPM for each eligible member$100 premium per month; 2% premium+ 1% premium guaranteeOr$2 PMPM rate + $1 PMPM guaranteeOther capitation rates can be established as specific set rateor a percentage based on age, sex, diagnoses or other criteriaA percentage premium rate means the provider and themanaged care organization agree to a percentage of thepremium, which is billed <strong>by</strong> the managed care organization.In the example above, the managed care organization bills a$100 premium per person and the provider is reimbursed3% of the premium amount. Percentage premiums areadvantageous if the provider is not interested in determiningeligibility for enrollees as is required with flat capitationrates. Calculation of a percentage premium rate willnecessitate the provider to analyze the premium informationgenerated <strong>by</strong> the managed care organization. Financialaudits may be a part of this process and should be includedin the contractual agreements between providers andmanaged care organizations.A flat per member per month rate is a very commoncalculation which is done in capitation. Flat rates make iteasy to compare one provider’s experience to another’s.Providers can translate flat pmpm rates into percentagepremium rates. The advantage of a flat pmpm rate is it iseasy to calculate, but the disadvantage is the provider mustkeep track of the number of enrollees or beneficiaries inthe managed care organization’s plan in order to calculatethe pmpm rate. This can be a cumbersome processrequiring the provider to receive, analyze, and audit themember data generated <strong>by</strong> the managed care organization.When this is too difficult a process, providers need toconsider a percentage premium rate.Guarantees are important to negotiate if the MCO isjust starting to market its services or there is limited or noutilization information available. In the example above,the capitation rate is calculated as a 2% premium paymentto the provider with a 1% premium guarantee rate. Theguarantee rate could also be calculated on a flat permember per month rate. For example, a $2 per member permonth rate and a $1 per member per month guarantee rate.A guarantee could also be calculated as a flat amount, forexample a $5,000 or $10,000 guarantee amount. Often,providers are asked to calculate a rate with limited data orexperience from the managed care organization. The useof a guarantee demonstrates the managed careorganization is committed to adding new enrollees andmeeting its marketing plans.Variable rates can be calculated in a wide variety ofsituations. Capitation rates are often calculated, and themost expensive or risky diagnoses or cases are excludedfrom the capitation rate. These diagnoses or cases canbecome carve outs from which a specific variablecapitation rate can be calculated. For example, aninfectious disease provider may want to carve out adiagnosis, such as AIDS, because of the unpredictable andpotentially high number of infections associated with thisdisease. Another example would be to develop a variablerate for a particular age group where the usage of providerservices would be extremely high. Product providers maycarve out certain types of equipment which are much moreexpensive than others. For example, a home equipmentsupplier might offer a capitation rate for usual equipment,but develop a variable rate for ventilators because oneventilator patient could represent an expense as high as thegeneral equipment for the member population.Managed care organizations do not particularly likecapitation rates with certain members not included in therate, especially if the provider does not offer a variable ratefor these members. In many markets, specialty providersare developing disease, age and other specific variablecapitation rates and these are often tied to diseasemanagement or carve out programs.INSURANCE VERIFICATIONInsurance verification is a critical process that needsto be performed to obtain reimbursement. Enteral servicesgenerally should not be provided before insuranceverification has taken place. If the provider starts enteralservices prior to verification, then there is a higher riskthat services won’t be covered or they will be paid at ahighly discounted rate.Most insurance verification information is obtained atthe point of intake for providers. Insurance verificationthen takes place with the patient’s primary and secondary(if in place) insurance companies. The phone numbers forinsurance verification can be found on the patient’sinsurance card or through the Kelly Insurance Directory.This directory can be ordered <strong>by</strong> calling 1-800-328-4144or through their web site at www.fbka.com.May, 2002 73
Once the number is obtained, the provider reimbursement personnel contact the company to determine the likelihood andamount of reimbursement. Unfortunately, this isn’t a guarantee of reimbursement, but an important step in the reimbursementprocess. Specific areas that need to be addressed are:Coverage InformationPolicy RestrictionsProvide: ➝ Pre-existing conditionsPatient name, sex, insured’s name, relation ➝ Homecare restrictionsto patient, insured’s identification number, ➝ Contracted providers and restrictionsgroup number and patient date of birth ➝ Time of service limitations➝ Timely filing requirementsDetermine: ➝ Precertification/preauthorization requirements➝ Whether or not the patient/insured are covered➝ Effective coverage dates➝ Enteral nutrition coverage➝ Certification/credentialling requirements➝ DeductiblesBilling Documentation and ProcessPricing➝ Claim forms (HCFA-1500, other) ➝ Acceptable methodologies➝ Codes (HCPCS) ➝ Negotiated rates➝ Medicare documentation ➝ Payment terms➝ Documentation process➝ Billing process (case management)CODES AND FORMSPrivate and managed care payers generally acceptthe HCFA-1500 for billing enteral products in the home.When the HCFA-1500 is required <strong>by</strong> the payer, theneither the HCPCS codes with a narrative will be requiredfor enteral billing or the payer may accept internallydeveloped codes <strong>by</strong> the provider. The ICD-9-CM codesare also typically required <strong>by</strong> payers to identify thepatient’s diagnosis. Where per diem billing has beennegotiated, the HCFA-1500 can still be used to denote theper diem rates. Some payers require itemizations with perdiem billing.When capitation payment methodologies are in place,billing and coding may not be required <strong>by</strong> the payer,depending upon how the capitation contract is written.Because the payer reimburses the provider a per memberper month (PMPM) rate prior to each month, the payer mayonly require utilization summaries of services for theirparticular member population. Where a payer requirescodes and forms on each patient, there is essentially anundue administrative burden placed on the provider.TIMELY FILINGManaged care organizations (MCOs) have differentpolicies on timely filings of claims. Some MCOs attemptto shorten the timely filing requirements to 30 to 60 daysand this may be unreasonable for your organization. Aminimal timely filing of 90 days should be requested anda period of one year is ideal. The reimbursementdepartment should work closely with the managed carecontracting department to ensure contracts are written in areasonable manner. Whatever the timely filing limits maybe, it is advisable to bill as soon as possible after servicesare rendered.74MEDICAL DOCUMENTATIONEven when insurance verification takes place,insurance companies will only approve services “subjectto medical necessity.” Private insurance companies do notrequire, nor do they prefer Medicare CMNs, so these arenot recommended.Medical documentation needed is a single page ofpatient information that is signed <strong>by</strong> the prescribingphysician. Sometimes these are called letters of medicalnecessity (LOMN). These can be completed in a letter orform and they typically need to include:❏ The patient’s name❏ The insured’s name❏ Patient diagnosis❏❏❏❏Type(s) of enteral products and servicesrenderedMethod of administrationEstimated durationThe provider name, address, telephone numberand federal tax identification number❏ The prescribing physician’s name, address,telephone number, signature and dateManaged care payers often require a precertification(precert) or prior authorization before services aredelivered and/or to continue services. Sometimes these areverbal and other times there is a paper certificationgenerated that needs to be submitted with the claim form.Other times there is a certification number that needs to beput on the claim form.May, 2002