You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
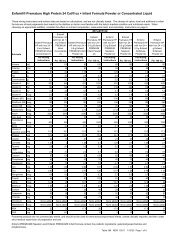
Timely FilingMedicare requires that all claims be submitted in atimely manner in order for payment to be made. BecauseHCFA is on a fiscal year that starts on October 1 st and endson September 30 th , they have established their timely filingtime frames to meet this fiscal year. The time-frames fortimely filing are summarized in Exhibit 11.the provider terminates the agreement earlier. The majoradvantage of these agreements is that a toll free numbercan be used to submit claims and after the Medicareportion is paid, the claim will be automatically transmittedto the MEDIGAP (secondary insurance) payer. Theseadvantages may be outweighed <strong>by</strong> the disadvantage ofhaving to accept Medicare assignment on each claim,whether or not the patient will qualify for service, and theneed to file claims to secondary carriers.EXHIBIT 11MEDICARE TIMELY FILING LIMITSInitial claims for servicesrendered between these dates:Must be filed<strong>by</strong> these dates:10/1/98 to 9/30/99 12/31/0010/1/99 to 9/30/00 12/31/0110/1/00 to 9/30/01 12/31/0210/1/01 to 9/30/02 12/31/03Initial claims that are filed more than one year after theservice date, but within the limits, will receive a 10%reduction in the Medicare allowable. If there is a denial anda resubmission is being made, it is generally advisable torefile the claim within six months from the denial date asindicated in the EOMB for Medicare to reconsider the claim.If a claim is being submitted for a denial, as is the caseif a secondary insurer requires a Medicare denial in orderto make a payment, the initial claim to Medicare must bemade within one year from the date of service.Assessment of BenefitsThere are two means <strong>by</strong> which the Part B provider canbe paid – assigned and non-assigned. Under assignment,the provider agrees to bill Medicare and receive paymentdirectly from Medicare. Under the non-assigned method,the patient pays the provider for the products, and then thePart B provider sends a non-assigned claim to Medicare. IfMedicare agrees to pay for the products, then payment ismade directly to the patient. The majority of enteralproducts are billed via the assigned method to Medicare.Medicare Participation Options for ProvidersPart B Medicare providers can participate in Medicarein two ways. The first is through the use of the Medicareprovider number that allows the provider to either acceptassignment or not accept assignment as discussed in the“assignment of benefits” section.The second option is to participate through a PARagreement. The PAR agreement mandates Medicareassignment on all claims for a period of one year, unlessBilling OptionsMedicare claims can be filed either <strong>by</strong> hardcopy orelectronically. Most providers file claims electronicallybecause the data is entered directly into the DMERCsystem, which eliminates the possibility of the DMERCexaminer incorrectly entering the data. In addition, claimpayments and denials may be returned sooner fromMedicare. In order to establish electronic billing, contactyour DMERC to request an application.Medicare as a Secondary PayerMedicare can be either a primary or secondary payer.This needs to be determined with insurance verificationprior to initiating services. Medicare may be a secondaryprovider if:May, 2002 57❏❏The patient has been injured in an automobileaccident and is covered <strong>by</strong> no fault insuranceThe patient is covered <strong>by</strong> worker’scompensation (an on the job accident)❏ The patient is eligible for group health benefitsthrough their employerHCFA requires providers to determine if Medicare isthe primary or secondary payer. Where Medicare is thesecondary payer, other carriers need to be billed firstbefore billing Medicare. When Medicare is billed as asecondary payer, the explanation of benefits (EOB) fromthe primary insurance company needs to be attached to theMedicare claim. For more specific information on billingMedicare as a secondary payer, contact the Medicaresecondary payer department at your DMERC.Physician UPIN DirectivesHCFA assigns unique physician identificationnumbers (UPIN) for each physician, and these are requiredon the HCFA-1500 form. The UPIN can be obtained <strong>by</strong>either asking the physician for their UPIN or obtaining aUPIN directly from the state in which the physician’soffice is located. To request a UPIN, the provider musthave a Medicare provider number and then send a writtenrequest to the Medicare carrier. Medicare allows one freecopy of the directory for each Medicare provider number.Copies of the UPIN directory can also be obtained throughthe Government Printing Office at the following address:U.S. Government Printing OfficeSuperintendent of DocumentsWashington, DC 20402