Empirical antimicrobial therapy for surgical infections in adults
Empirical antimicrobial therapy for surgical infections in adults
Empirical antimicrobial therapy for surgical infections in adults
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
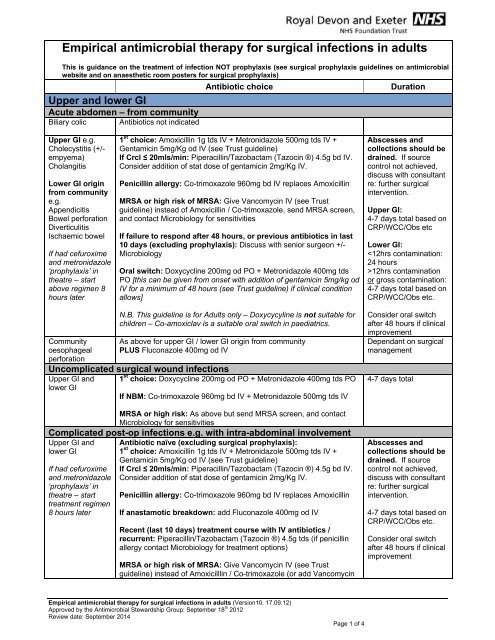
<strong>Empirical</strong> <strong>antimicrobial</strong> <strong>therapy</strong> <strong>for</strong> <strong>surgical</strong> <strong><strong>in</strong>fections</strong> <strong>in</strong> <strong>adults</strong>This is guidance on the treatment of <strong>in</strong>fection NOT prophylaxis (see <strong>surgical</strong> prophylaxis guidel<strong>in</strong>es on <strong>antimicrobial</strong>website and on anaesthetic room posters <strong>for</strong> <strong>surgical</strong> prophylaxis)Upper and lower GIAcute abdomen – from communityBiliary colic Antibiotics not <strong>in</strong>dicatedAntibiotic choiceDurationUpper GI e.g.Cholecystitis (+/-empyema)CholangitisLower GI orig<strong>in</strong>from communitye.g.AppendicitisBowel per<strong>for</strong>ationDiverticulitisIschaemic bowelIf had cefuroximeand metronidazole‘prophylaxis’ <strong>in</strong>theatre – startabove regimen 8hours later1 st choice: Amoxicill<strong>in</strong> 1g tds IV + Metronidazole 500mg tds IV +Gentamic<strong>in</strong> 5mg/Kg od IV (see Trust guidel<strong>in</strong>e)If Crcl ≤ 20mls/m<strong>in</strong>: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g bd IV.Consider addition of stat dose of gentamic<strong>in</strong> 2mg/Kg IV.Penicill<strong>in</strong> allergy: Co-trimoxazole 960mg bd IV replaces Amoxicill<strong>in</strong>MRSA or high risk of MRSA: Give Vancomyc<strong>in</strong> IV (see Trustguidel<strong>in</strong>e) <strong>in</strong>stead of Amoxicill<strong>in</strong> / Co-trimoxazole, send MRSA screen,and contact Microbiology <strong>for</strong> sensitivitiesIf failure to respond after 48 hours, or previous antibiotics <strong>in</strong> last10 days (exclud<strong>in</strong>g prophylaxis): Discuss with senior surgeon +/-MicrobiologyOral switch: Doxycycl<strong>in</strong>e 200mg od PO + Metronidazole 400mg tdsPO [this can be given from onset with addition of gentamic<strong>in</strong> 5mg/kg odIV <strong>for</strong> a m<strong>in</strong>imum of 48 hours (see Trust guidel<strong>in</strong>e) if cl<strong>in</strong>ical conditionallows]Abscesses andcollections should bedra<strong>in</strong>ed. If sourcecontrol not achieved,discuss with consultantre: further <strong>surgical</strong><strong>in</strong>tervention.Upper GI:4-7 days total based onCRP/WCC/Obs etcLower GI:12hrs contam<strong>in</strong>ationor gross contam<strong>in</strong>ation:4-7 days total based onCRP/WCC/Obs etc.N.B. This guidel<strong>in</strong>e is <strong>for</strong> Adults only – Doxycycyl<strong>in</strong>e is not suitable <strong>for</strong>children – Co-amoxiclav is a suitable oral switch <strong>in</strong> paediatrics.Communityoesophagealper<strong>for</strong>ationUncomplicated <strong>surgical</strong> wound <strong><strong>in</strong>fections</strong>Upper GI andlower GIAs above <strong>for</strong> upper GI / lower GI orig<strong>in</strong> from communityPLUS Fluconazole 400mg od IV1 st choice: Doxycycl<strong>in</strong>e 200mg od PO + Metronidazole 400mg tds POIf NBM: Co-trimoxazole 960mg bd IV + Metronidazole 500mg tds IVMRSA or high risk: As above but send MRSA screen, and contactMicrobiology <strong>for</strong> sensitivitiesComplicated post-op <strong><strong>in</strong>fections</strong> e.g. with <strong>in</strong>tra-abdom<strong>in</strong>al <strong>in</strong>volvementUpper GI andlower GIIf had cefuroximeand metronidazole‘prophylaxis’ <strong>in</strong>theatre – starttreatment regimen8 hours laterAntibiotic naïve (exclud<strong>in</strong>g <strong>surgical</strong> prophylaxis):1 st choice: Amoxicill<strong>in</strong> 1g tds IV + Metronidazole 500mg tds IV +Gentamic<strong>in</strong> 5mg/Kg od IV (see Trust guidel<strong>in</strong>e)If Crcl ≤ 20mls/m<strong>in</strong>: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g bd IV.Consider addition of stat dose of gentamic<strong>in</strong> 2mg/Kg IV.Penicill<strong>in</strong> allergy: Co-trimoxazole 960mg bd IV replaces Amoxicill<strong>in</strong>If anastamotic breakdown: add Fluconazole 400mg od IVRecent (last 10 days) treatment course with IV antibiotics /recurrent: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g tds (if penicill<strong>in</strong>allergy contact Microbiology <strong>for</strong> treatment options)MRSA or high risk of MRSA: Give Vancomyc<strong>in</strong> IV (see Trustguidel<strong>in</strong>e) <strong>in</strong>stead of Amoxicilll<strong>in</strong> / Co-trimoxazole (or add Vancomyc<strong>in</strong>Consider oral switchafter 48 hours if cl<strong>in</strong>icalimprovementDependant on <strong>surgical</strong>management4-7 days totalAbscesses andcollections should bedra<strong>in</strong>ed. If sourcecontrol not achieved,discuss with consultantre: further <strong>surgical</strong><strong>in</strong>tervention.4-7 days total based onCRP/WCC/Obs etc.Consider oral switchafter 48 hours if cl<strong>in</strong>icalimprovement<strong>Empirical</strong> <strong>antimicrobial</strong> <strong>therapy</strong> <strong>for</strong> <strong>surgical</strong> <strong><strong>in</strong>fections</strong> <strong>in</strong> <strong>adults</strong> (Version10. 17.09.12)Approved by the Antimicrobial Stewardship Group: September 18 th 2012Review date: September 2014Page 1 of 4
IV if on Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®)), send MRSA screen, andcontact Microbiology <strong>for</strong> sensitivitiesIf failure to respond after 48 hours: Discuss with senior surgeon +/-MicrobiologyOral switch: Doxycycl<strong>in</strong>e 200mg od PO + Metronidazole 400mg tdsPO [this can be given from onset with addition of gentamic<strong>in</strong> 5mg/kg odIV <strong>for</strong> a m<strong>in</strong>imum of 48 hours (see Trust guidel<strong>in</strong>e) if cl<strong>in</strong>ical conditionallows]As above <strong>for</strong> complicated post-op <strong><strong>in</strong>fections</strong>PLUS Fluconazole 400mg od IVPost-opoesophagealper<strong>for</strong>ationSevere Sepsis (see def<strong>in</strong>ition below)Upper GI andlower GISevere Sepsis: ≥2SIRS criteriaAND evidence of<strong>in</strong>fection ANDorgan dysfunctionAntibiotic naïve (exclud<strong>in</strong>g <strong>surgical</strong> prophylaxis): Amoxicill<strong>in</strong> 1g tdsIV + Metronidazole 500mg tds IV + Gentamic<strong>in</strong> 5mg/Kg od IV (seeTrust guidel<strong>in</strong>e)If Crcl ≤ 20mls/m<strong>in</strong>: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g bd IV.Consider addition of stat dose of gentamic<strong>in</strong> 2mg/Kg IV.Penicill<strong>in</strong> allergy: Co-trimoxazole 960mg bd IV replaces Amoxicill<strong>in</strong>MRSA or high risk of MRSA: Give Vancomyc<strong>in</strong> IV (see Trustguidel<strong>in</strong>e) <strong>in</strong>stead of Amoxicill<strong>in</strong> / Co-trimoxazole, send MRSA screen,and contact Microbiology <strong>for</strong> sensitivitiesHealthcare associated or recent treatment course (last 10 days)with IV antibiotics: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g tds IV ±Vancomyc<strong>in</strong> IV (see Trust guidel<strong>in</strong>e). Send MRSA screen and stopVancomyc<strong>in</strong> if screen & diagnostic specimens negative. If penicill<strong>in</strong>allergy contact Microbiology <strong>for</strong> treatment optionsPANCREATITIS – calculate *Glasgow scoreMild (score 0-2) Antibiotics not <strong>in</strong>dicatedDependant on <strong>surgical</strong>managementTreat with<strong>in</strong> ONE hourof diagnosis.Review daily – discusswith Microbiology with<strong>in</strong>next 24 – 48 hoursSend MRSA screenIf source control notachieved, discuss withconsultant re: further<strong>surgical</strong> <strong>in</strong>terventionSevere(score 3-8)>30% necrosis onCT scan at 48hours1st choice: Piperacill<strong>in</strong>/tazobactam (Tazoc<strong>in</strong>®) 4.5g tds IVMild penicill<strong>in</strong> allergy: Meropenem 1g tds IVSevere allergy: Discuss with MicrobiologyMRSA: Add Vancomyc<strong>in</strong> IV (see Trust guidel<strong>in</strong>e)Add Fluconazole 400mg od IV to above regimenMaximum 10 days*Glasgow score: score 1 po<strong>in</strong>t <strong>for</strong> any of the follow<strong>in</strong>g occurr<strong>in</strong>g at any time <strong>in</strong> the first 48 hours of admission:• Age >55 years• Serum album<strong>in</strong> 16.1 mmols/L (45 mg/dL)• WBC count >15 x 10^9/L (15 x 10^3/microlitre)Glasgow Score Severity Assessment0-2 Mild3-8 Severe<strong>Empirical</strong> <strong>antimicrobial</strong> <strong>therapy</strong> <strong>for</strong> <strong>surgical</strong> <strong><strong>in</strong>fections</strong> <strong>in</strong> <strong>adults</strong> (Version 10. 17.09.12)Approved by the Antimicrobial Stewardship Group: September 18 th 2012Review date: September 2014Page 2 of 4
Breast Antibiotic choice DurationMastitis1 st choice: Flucloxacill<strong>in</strong> 1g qds PO/IVAbscessBreastuncomplicated<strong>surgical</strong> site<strong><strong>in</strong>fections</strong>Penicill<strong>in</strong> allergy: Doxycycl<strong>in</strong>e 200mg od PO or Vancomyc<strong>in</strong> IV (seeTrust guidel<strong>in</strong>e)MRSA: Add Vancomyc<strong>in</strong> IV if not already on (see Trust guidel<strong>in</strong>e) orcheck lab sensitivities <strong>for</strong> oral optionIf necrotis<strong>in</strong>g <strong>in</strong>fection suspected: Add Cl<strong>in</strong>damyc<strong>in</strong> 1.2g qds IV anddiscuss urgently with senior surgeon +/- MicrobiologyN.B. Doxycycyl<strong>in</strong>e is not suitable if pregnant or breastfeed<strong>in</strong>g – contactMicrobiology <strong>for</strong> alternative treatment options <strong>for</strong> these patients.Abscesses andcollections should bedra<strong>in</strong>ed4-10 days total basedon CRP/WCC/Obs etcAcute breastimplant <strong>in</strong>fectionMust bediscussed withConsultantsurgeon1 st choice: Flucloxacill<strong>in</strong> 1-2 g qds IVPenicill<strong>in</strong> allergy: Vancomyc<strong>in</strong> IV (see Trust guidel<strong>in</strong>e)If sub-acute or late <strong>in</strong>fection: discuss <strong>antimicrobial</strong> management withMicrobiology14 days total (discussoral switch withMicrobiology)Urology Antibiotic choice DurationUTIUncomplicatedCheck cultureresults & modifytreatmentaccord<strong>in</strong>gly1 st choice: Trimethoprim 200mg bd PO2 nd Choice: Nitrofuranto<strong>in</strong> 50–100mg qds POIf pregnant: Cefalex<strong>in</strong> 500mg bd PO <strong>for</strong> 7 days – send ur<strong>in</strong>e cultureseven days after completion to confirm cure3 days <strong>for</strong> female7 days <strong>for</strong> male7 days <strong>for</strong> pregnantComplicated (e.g. catheter, structural abnormality, post-op etc)7 days1 st choice: Amoxicill<strong>in</strong> 1g tds IV + Gentamic<strong>in</strong> 5mg/kg od IV (see Trustguidel<strong>in</strong>e, max 5 days). Oral switch asap Trimethoprim 200mg bd PO2 nd Choice (penicill<strong>in</strong> allergic): Gentamic<strong>in</strong> 5mg/kg od IV (see Trustguidel<strong>in</strong>e, max 5 days). Oral switch asap Trimethoprim 200mg bd POPyelonephritis:10-14 daysAcute prostatitisEpididymo-orchitisSee full guidel<strong>in</strong>e1 st choice: Amoxicill<strong>in</strong> 1g tds IV + Gentamic<strong>in</strong> 5mg/kg od IV (see Trustguidel<strong>in</strong>e, max 5 days). Oral switch asap Co-amoxiclav 625mg tds PO2 nd Choice (penicill<strong>in</strong> allergic): Gentamic<strong>in</strong> 5mg/kg od IV (see Trustguidel<strong>in</strong>e, max 5 days). Oral switch asap discuss with MicrobiologyUrological severe sepsis see below1 st choice: Trimethoprim 200mg bd PO2 nd choice after discussion with Microbiology: Ciprofloxac<strong>in</strong> 500mgbd POLikely STD cause: Doxycycl<strong>in</strong>e 100mg bd PO + Ceftriaxone 500mgIM s<strong>in</strong>gle dose (omit if gonorrhoea unlikely)Likely enteric cause: Ciprofloxac<strong>in</strong> 500mg bd PO14 days10-14 days10 days<strong>Empirical</strong> <strong>antimicrobial</strong> <strong>therapy</strong> <strong>for</strong> <strong>surgical</strong> <strong><strong>in</strong>fections</strong> <strong>in</strong> <strong>adults</strong> (Version 10. 17.09.12)Approved by the Antimicrobial Stewardship Group: September 18 th 2012Review date: September 2014Page 3 of 4
Urologicaluncomplicated<strong>surgical</strong> wound<strong><strong>in</strong>fections</strong>Urologicalcomplicated postop<strong>in</strong>fectionUrological severesepsisSevere Sepsis: ≥2SIRS criteriaAND evidence of<strong>in</strong>fection ANDorgan dysfunction1 st choice: Doxycycl<strong>in</strong>e 200mg od PO + Metronidazole 400mg tds POIf NBM: Co-trimoxazole 960mg bd IV + Metronidazole 500mg tds IVMRSA or high risk: as above, send MRSA screen, and contactMicrobiology <strong>for</strong> sensitivitiesAntibiotic naïve (exclud<strong>in</strong>g <strong>surgical</strong> prophylaxis):1 st choice: Co-trimoxazole 960mg bd IV + Metronidazole 500mg tdsIV + Gentamic<strong>in</strong> 5mg/Kg od IV (see Trust guidel<strong>in</strong>e)If Crcl ≤ 20mls/m<strong>in</strong>: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g bd IV.Consider addition of stat dose of gentamic<strong>in</strong> 2mg/Kg IV.Recent (last 10 days) treatment course with IV antibiotics /recurrent: Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g tds IV (if penicill<strong>in</strong>allergy contact Microbiology <strong>for</strong> treatment options)MRSA or high risk of MRSA: Give Vancomyc<strong>in</strong> IV (see Trustguidel<strong>in</strong>e) <strong>in</strong>stead of Co-trimoxazole (or add Vancomyc<strong>in</strong> IV if onPiperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®)), send MRSA screen, and contactMicrobiology <strong>for</strong> sensitivitiesIf failure to respond after 48 hours: Discuss with senior surgeon +/-MicrobiologyOral switch: Doxycycl<strong>in</strong>e 200mg od PO + Metronidazole 400mg tdsPO [this can be given from onset with addition of gentamic<strong>in</strong> 5mg/kg odIV <strong>for</strong> a m<strong>in</strong>imum of 48 hours (see Trust guidel<strong>in</strong>e) if cl<strong>in</strong>ical conditionallows]1 st choice (community acquired or healthcare associated):Piperacill<strong>in</strong>/Tazobactam (Tazoc<strong>in</strong> ®) 4.5g tds IV + Gentamic<strong>in</strong> 5mg/kgstat IV (see Trust guidel<strong>in</strong>e). Send MRSA screenSevere penicill<strong>in</strong> allergy: Discuss with Microbiology4-7 days total based onCRP/WCC/Obs etcAbscesses andcollections should bedra<strong>in</strong>ed4-7 days total based onCRP/WCC/Obs etc.Treat with<strong>in</strong> ONE hourof diagnosis.Review daily – discusswith Microbiology with<strong>in</strong>next 24 -48 hours• This does not cover Surgical Prophylaxis – there is separate guidance on IaN & on posters <strong>in</strong>anaesthetic rooms.• Source control (i.e. surgery or dra<strong>in</strong>age) is the primary treatment – antibiotics are at best an adjunct.• Severe sepsis def<strong>in</strong>ition from ‘Surviv<strong>in</strong>g Sepsis’: ≥2 SIRS criteriao Temp38.3°Co Heart rate >90 beats/m<strong>in</strong>uteo Respiratory rate >20 breaths/m<strong>in</strong>ute or Pa CO 2 12 x10 9 /L or 5 days without discuss<strong>in</strong>g withMicrobiology.• Antibiotic treatment must be reviewed <strong>in</strong> light of significant cultures and targeted appropriately.<strong>Empirical</strong> <strong>antimicrobial</strong> <strong>therapy</strong> <strong>for</strong> <strong>surgical</strong> <strong><strong>in</strong>fections</strong> <strong>in</strong> <strong>adults</strong> (Version 10. 17.09.12)Approved by the Antimicrobial Stewardship Group: September 18 th 2012Review date: September 2014Page 4 of 4