Fixation with a Cannulated Screw Displaced Scaphoid Fractures ...
Fixation with a Cannulated Screw Displaced Scaphoid Fractures ...
Fixation with a Cannulated Screw Displaced Scaphoid Fractures ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
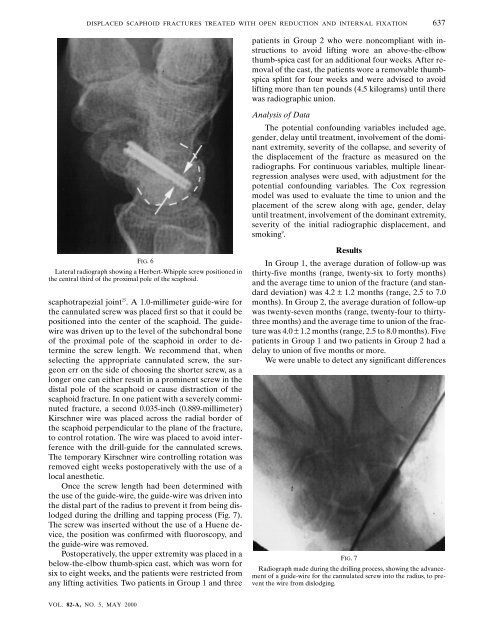
DISPLACED SCAPHOID FRACTURES TREATED WITH OPEN REDUCTION AND INTERNAL FIXATION 637patients in Group 2 who were noncompliant <strong>with</strong> instructionsto avoid lifting wore an above-the-elbowthumb-spica cast for an additional four weeks. After removalof the cast, the patients wore a removable thumbspicasplint for four weeks and were advised to avoidlifting more than ten pounds (4.5 kilograms) until therewas radiographic union.Analysis of DataThe potential confounding variables included age,gender, delay until treatment, involvement of the dominantextremity, severity of the collapse, and severity ofthe displacement of the fracture as measured on theradiographs. For continuous variables, multiple linearregressionanalyses were used, <strong>with</strong> adjustment for thepotential confounding variables. The Cox regressionmodel was used to evaluate the time to union and theplacement of the screw along <strong>with</strong> age, gender, delayuntil treatment, involvement of the dominant extremity,severity of the initial radiographic displacement, andsmoking 9 .FIG. 6Lateral radiograph showing a Herbert-Whipple screw positioned inthe central third of the proximal pole of the scaphoid.scaphotrapezial joint 25 . A 1.0-millimeter guide-wire forthe cannulated screw was placed first so that it could bepositioned into the center of the scaphoid. The guidewirewas driven up to the level of the subchondral boneof the proximal pole of the scaphoid in order to determinethe screw length. We recommend that, whenselecting the appropriate cannulated screw, the surgeonerr on the side of choosing the shorter screw, as alonger one can either result in a prominent screw in thedistal pole of the scaphoid or cause distraction of thescaphoid fracture. In one patient <strong>with</strong> a severely comminutedfracture, a second 0.035-inch (0.889-millimeter)Kirschner wire was placed across the radial border ofthe scaphoid perpendicular to the plane of the fracture,to control rotation. The wire was placed to avoid interference<strong>with</strong> the drill-guide for the cannulated screws.The temporary Kirschner wire controlling rotation wasremoved eight weeks postoperatively <strong>with</strong> the use of alocal anesthetic.Once the screw length had been determined <strong>with</strong>the use of the guide-wire, the guide-wire was driven intothe distal part of the radius to prevent it from being dislodgedduring the drilling and tapping process (Fig. 7).The screw was inserted <strong>with</strong>out the use of a Huene device,the position was confirmed <strong>with</strong> fluoroscopy, andthe guide-wire was removed.Postoperatively, the upper extremity was placed in abelow-the-elbow thumb-spica cast, which was worn forsix to eight weeks, and the patients were restricted fromany lifting activities. Two patients in Group 1 and threeResultsIn Group 1, the average duration of follow-up wasthirty-five months (range, twenty-six to forty months)and the average time to union of the fracture (and standarddeviation) was 4.2 ± 1.2 months (range, 2.5 to 7.0months). In Group 2, the average duration of follow-upwas twenty-seven months (range, twenty-four to thirtythreemonths) and the average time to union of the fracturewas 4.0 ± 1.2 months (range, 2.5 to 8.0 months). Fivepatients in Group 1 and two patients in Group 2 had adelay to union of five months or more.We were unable to detect any significant differencesFIG. 7Radiograph made during the drilling process, showing the advancementof a guide-wire for the cannulated screw into the radius, to preventthe wire from dislodging.VOL. 82-A, NO. 5, MAY 2000