Allergic coNtAct DermAtitis of the foot - The Dermatologist
Allergic coNtAct DermAtitis of the foot - The Dermatologist
Allergic coNtAct DermAtitis of the foot - The Dermatologist
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Allergen FocusIn this column, we highlight ACDand explore top relevant allergens, regional-and topic-based dermatitis presentationsand clinical tips and pearls fordiagnosis and treatment.<strong>Allergic</strong> Contact Dermatitis <strong>of</strong> <strong>the</strong> FootFoot dermatitis can be a chronic andrecalcitrant condition. Disability frompainful fissures and impaired gait maybe seen. Active dermatitis may lead to aweakened cutaneous barrier, which increases<strong>the</strong> potential risk for infection.Occupational implications also exist, inthat many patients require protective<strong>foot</strong>wear for employment. If an allergyto this protective barrier equipment develops,<strong>the</strong> patient may be forced to seeko<strong>the</strong>r employment.When discussing ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong>,<strong>the</strong>re is a relatively stable microenvironment<strong>of</strong> contactants, composed principally<strong>of</strong> rubber compounds and accelerators,chromates, adhesives, dyes andretained contaminants, such as topicalmedicaments. 9-13 Table 1 highlights<strong>the</strong> most common <strong>of</strong> <strong>the</strong>se allergens.In cultures that tend to favor <strong>the</strong> use<strong>of</strong> <strong>foot</strong>wear, <strong>the</strong> shoe and sock encapsulatethis microenvironment and are<strong>the</strong> source <strong>of</strong> potential allergens. Studieshave estimated that <strong>the</strong> prevalence <strong>of</strong><strong>foot</strong> dermatitis due to shoes ranges from3.3% to 11.7% <strong>of</strong> patch-test patients. 14<strong>The</strong> development <strong>of</strong> ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> isfavored by friction and <strong>the</strong> hot, humidenvironment within <strong>the</strong> shoe. 15While this may initially appearstraightforward, one realizes on closerinspection that <strong>the</strong> anatomy <strong>of</strong> <strong>foot</strong>wearis quite complex. <strong>The</strong> approach t<strong>of</strong>ootwear can be simplified by consideringfive separate systems: (1) uppers orstraps, (2) soles, (3) insoles, (4) adhesivesand (5) heel and toe stiffeners. 16<strong>The</strong> upper or strap is <strong>the</strong> component<strong>of</strong> <strong>the</strong> <strong>foot</strong>wear that attaches to <strong>the</strong> soleand covers <strong>the</strong> dorsal <strong>foot</strong>. Lea<strong>the</strong>r isTable 1. Top Allergens 14,18AllergenMercaptobenzothiazoleMercapto MixThiuram MixCarba MixMixed Dialkyl ThioureasDithiodimorpholineBlack Rubber MixPotassium DichromateGlutaraldehydeFormaldehydep-tert-butylphenol formaldehyde resin (PTBFR)ColophonyEthyl/Methyl AcrylateDiaminodiphenylmethanecommonly utilized and may <strong>the</strong>reforebe a source <strong>of</strong> chromate exposure, dependingon how <strong>the</strong> lea<strong>the</strong>r was tanned.Some types <strong>of</strong> lea<strong>the</strong>r undergo a multisteptanning process. This process maystart with chromate tanning and involvesubsequent tanning with formaldehydeor glutaraldehyde. 12,16 In a retrospectiveanalysis published in 2007 by <strong>the</strong> NorthAmerican Contact Dermatitis Group(NACDG), potassium dichromate wasfound to be <strong>the</strong> second-most frequentshoe-related allergen. Only <strong>the</strong> adhesivep-tert-butylphenol-formaldehyde resinFoot dermatitis can be a chronic and recalcitrant condition.Disability from painful fissures and impaired gait may be seen.Active dermatitis may also lead to a weakened cutaneousbarrier, which increases <strong>the</strong> potential risk for infection.Occupational implications also exist, in that many patientsrequire protective <strong>foot</strong>wear for <strong>the</strong>ir employment.NickelPreservatives(PTBFR) was more frequently positiveon patch testing. 14<strong>The</strong> sole <strong>of</strong> a shoe is <strong>the</strong> base. <strong>The</strong>chemical composition <strong>of</strong> <strong>the</strong> sole dependson <strong>the</strong> type <strong>of</strong> shoe; lea<strong>the</strong>r, neoprene,polyurethane and various types <strong>of</strong>rubber are commonly used. Neopreneis oil-resistant and commonly foundin <strong>the</strong> sole <strong>of</strong> occupational <strong>foot</strong>wear. 16LocationRubberRubberRubberRubberRubberRubberRubberLea<strong>the</strong>rLea<strong>the</strong>rLea<strong>the</strong>rAdhesivesAdhesivesAdhesivesPolyurethaneLace eyelets, bucklesBiocidesWhile overall <strong>the</strong> single most commonshoe allergen in North America appearsto be PTBFR followed by chromate,taken as a group, rubber additives causea greater number <strong>of</strong> reactions. 14 In o<strong>the</strong>rwords, rubber-related chemicals are <strong>the</strong>most common shoe allergen categoryoverall. This group includes carba mix,thiuram mix, mercaptobenzothiazole(MBT), mercapto mix, mixed dialkylthioureas, dithiodimorpholine (DTDM)and black rubber mix.<strong>The</strong> insole provides cushion and archsupport. <strong>The</strong> composition <strong>of</strong> <strong>the</strong> insolemay be lea<strong>the</strong>r, polyurethane, neopreneor a composite <strong>of</strong> rubber or paper fibers.Composite fiber insoles are cheaperand may be found in less expensive<strong>foot</strong>wear. <strong>The</strong>se fibers are typically heldtoge<strong>the</strong>r by a resinous glue. To preventmicrobial degradation <strong>of</strong> <strong>the</strong>se fibers, abiocides (preservative) is also typicallyadded. 16 Insoles <strong>of</strong> a shoe come in directcontact with <strong>the</strong> sock and plantar<strong>foot</strong> region. While <strong>the</strong> plantar <strong>foot</strong> is innatelyresistant to ACD (because to <strong>the</strong>relatively thick skin <strong>of</strong> this region), <strong>the</strong>reare several key factors that can lead tosensitization. Potential sensitizing haptens<strong>of</strong> <strong>the</strong> insole may be released withheat, friction and sweat over time. Becausemost socks are porous, potentialallergens leached from <strong>the</strong> insole infil-November 2012 | <strong>The</strong> <strong>Dermatologist</strong> ® | www.<strong>the</strong>-dermatologist.com 21
Allergen FocusTable 2. Differential Diagnosis <strong>of</strong> <strong>Allergic</strong> Contact Dermatitis <strong>of</strong> <strong>the</strong> Foot 18,19Diagnosis Clinical Presentation CommentsACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> (upper/strap) Dorsal <strong>foot</strong> dermatitis sparing <strong>the</strong> interdigital spaces. Classic “shoe pattern dermatitis”ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> (insole) Plantar dermatitis sparing <strong>the</strong> plantar arch and proximal creases <strong>of</strong> <strong>the</strong> toes. Typically spares areas most involved in palmoplantar pustulosis.ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> (sole)Can present as plantar dermatitis or as localized plaques <strong>of</strong> dermatitis on <strong>the</strong>thighs/buttock in patients with a habit <strong>of</strong> sitting with <strong>the</strong>ir legs folded and<strong>the</strong>ir feet underneath <strong>the</strong>m.ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> (stiffeners) Dermatitis involving <strong>the</strong> dorsal toes and heels. Major differential for heel involvement is irritant dermatitis.ACD <strong>of</strong> <strong>the</strong> <strong>foot</strong> (adhesives)Irritant dermatitisMay present with dorsal <strong>foot</strong> dermatitis, plantar dermatitis or heel and toedermatitis.Parched and glazed appearance <strong>of</strong> skin with fine scaling that favors <strong>the</strong> heelsor bridges <strong>the</strong> dorsal toes and <strong>foot</strong> in an “apron pattern.”Heel irritant dermatitis is seen more <strong>of</strong>ten with frequent wearing<strong>of</strong> open back shoes such as flip flops. <strong>The</strong> apron pattern ismore <strong>of</strong>ten seen with atopic dermatitis.Atopic Dermatitis Favors <strong>the</strong> dorsal <strong>foot</strong> in childhood and <strong>the</strong> palmoplantar skin in adulthood. Look for o<strong>the</strong>r atopic stigmata such as Dennie-Morgan lines,allergic shinners, and hyperlinear <strong>the</strong>nar eminences.Nummular DermatitisJuvenile Plantar DermatosisPompholyxDyshidrotic EczemaPsoriasisPalmoplantar pustulosisPityriasis rubra pilarisTinea pedisDiscrete, coin-shaped crusted plaques on <strong>the</strong> dorsal <strong>foot</strong>.Smooth and glazed appearance with fine scaling localized to <strong>the</strong> plantar aspect<strong>of</strong> <strong>the</strong> fore<strong>foot</strong> and toes with sparing <strong>of</strong> <strong>the</strong> interdigital spaces.Severe sudden outbreaks <strong>of</strong> intensely pruritic vesicles symmetrically on <strong>the</strong>palms, soles and lateral aspects <strong>of</strong> <strong>the</strong> digits.Similar to pompholyx but more <strong>of</strong> a subacute to chronic clinical presentationra<strong>the</strong>r than an acute sudden outbreak.Well-demarcated, ery<strong>the</strong>matous plaques with micaceous scale can be seen on<strong>the</strong> dorsal <strong>foot</strong>. Plantar lesions tend to be more hyperkeratotic and <strong>of</strong>ten havea pustular quality. Nail pitting.Bilateral and symmetric ery<strong>the</strong>matous plaques studded with minute pustuleson <strong>the</strong> central palms and soles.Salmon-orange appearing hyperkeratosis <strong>of</strong> <strong>the</strong> plantar <strong>foot</strong> extending up <strong>the</strong>sides in <strong>the</strong> so-called “sandal pattern.” Rarely associated with nail pitting.Dull ery<strong>the</strong>ma and fine scale on <strong>the</strong> sole and sides <strong>of</strong> <strong>the</strong> feet in a “moccasinor sandal pattern.” May see similar fine scaling on one palm giving a “onehand, two feet pattern.”Also known as dermatitis plantaris sicca or “sweaty sockdermatitis.”Keratoderma blenorrhagicum is a plantar eruption characteristic<strong>of</strong> reactive arthritis (Reiter Syndrome).Associated with smoking and thyroid disorders. Likely a localizedacral variant <strong>of</strong> psoriasis.KOH positive for dermatophyte hyphae is diagnostic.T. mentagrophytes can produce a bullous tinea that favors <strong>the</strong>plantar arch.trate <strong>the</strong> textile matrix easily. This createsa reservoir <strong>of</strong> potential allergens indirect contact with <strong>the</strong> skin <strong>of</strong> <strong>the</strong> <strong>foot</strong>for prolonged periods <strong>of</strong> time. <strong>The</strong>normally robust cutaneous barrier <strong>of</strong><strong>the</strong> plantar <strong>foot</strong> may also be diminishedbecause <strong>of</strong> o<strong>the</strong>r conditions like eczemaor dermatophyte infection.Adhesives are necessary in <strong>the</strong> majority<strong>of</strong> <strong>foot</strong>wear for assembly. <strong>The</strong>seglues are used to attach <strong>the</strong> insole to<strong>the</strong> sole and to bind various components<strong>of</strong> <strong>the</strong> shoe top toge<strong>the</strong>r. <strong>The</strong>y area major source <strong>of</strong> shoe allergy. As mentioned,<strong>the</strong> primary relevant shoe adhesivefound on patch testing to cause<strong>foot</strong> dermatitis is <strong>the</strong> phenolic resinPTBFR. PTBFR has been shown toaccount for 10% to 20% <strong>of</strong> allergic reactionsto <strong>foot</strong>wear. 15,16 It has been usedas an additive in rubber glues since <strong>the</strong>1950s and is ideally suited for <strong>foot</strong>wearmanufacturing due to its strong adhesionto both lea<strong>the</strong>r and rubber. 17Heel and toe stiffeners are alsoknown as counters. This component <strong>of</strong><strong>the</strong> shoe is meant to retain <strong>the</strong> overallshape <strong>of</strong> <strong>the</strong> shoe while streng<strong>the</strong>ning<strong>the</strong> heel and toe. Stiffeners have aspectrum <strong>of</strong> complexity, ranging from asimple layer <strong>of</strong> inert adhesive to a complexweb <strong>of</strong> polyester or cotton. Similarto insoles, stiffeners can be a source <strong>of</strong>exposure to rubber compounds, adhesivesand biocides. 16Differential Diagnosis<strong>The</strong> differential diagnosis for an eczematouseruption <strong>of</strong> <strong>the</strong> <strong>foot</strong> can beclinically challenging. A categorical approachis helpful. <strong>The</strong> majority <strong>of</strong> casescan be sorted into one <strong>of</strong> <strong>the</strong> followingprinciple categories: (1) exogenousdermatitis, (2) endogenous dermatitis,(3) acral papulosquamous entities, (4)infectious entities and (5) hybrid dermatitis.18,19 Table 2 highlights this differentialdiagnosis.Exogenous dermatitis includes bothirritant and allergic contact dermatitis.<strong>The</strong> morphology <strong>of</strong> this group is <strong>the</strong>prototypical spectrum <strong>of</strong> acute, subacuteand chronic eczematous eruptions. Itis typical to see a poorly demarcated,spreading, ery<strong>the</strong>matous and edematous,papulovesicular eruption. However, as<strong>the</strong> lesions progress along <strong>the</strong> spectrumto a more chronic state, <strong>the</strong>re is morescaling and lichenification, which cancause some confusion clinically with<strong>the</strong> papulosquamous eruptions. Symptomatologyis useful in that pruritusfavors an allergic etiology and burningand stinging are more <strong>of</strong>ten seen withirritant etiologies. Finally, regional distributionis important to note. <strong>The</strong> clas-22 November 2012 | <strong>The</strong> <strong>Dermatologist</strong> ® | www.<strong>the</strong>-dermatologist.com
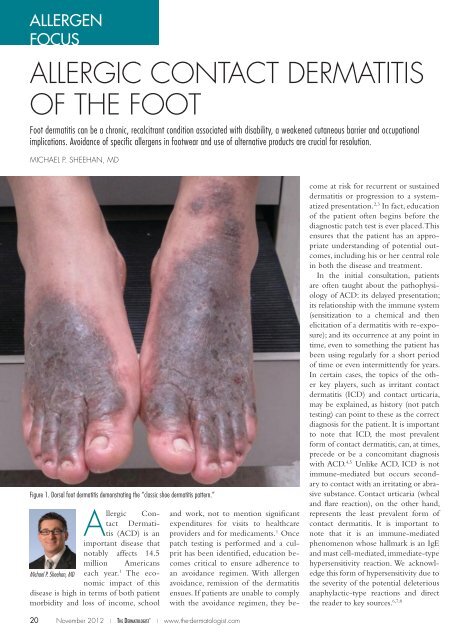
sic “shoe pattern dermatitis” on <strong>the</strong> <strong>foot</strong>is suggestive <strong>of</strong> allergic contact dermatitis(Figure 1). This pattern shows aneczematous process involving <strong>the</strong> dorsal<strong>foot</strong> and ankle with notable sparing <strong>of</strong><strong>the</strong> inter-digital spaces. <strong>The</strong>re is <strong>of</strong>tena relative symmetry, but one side maybe more heavily affected than <strong>the</strong> o<strong>the</strong>r.Spreading <strong>of</strong> <strong>the</strong> process up <strong>the</strong> anklesover time is also a clue to ACD. Thisis particularly true in <strong>the</strong> setting <strong>of</strong> achronic, stable, well-localized dermatitisthat <strong>the</strong>n shifts to become poorly localizedand spreading.Endogenous dermatitis is <strong>of</strong>ten <strong>the</strong>most difficult to separate from allergiccontact dermatitis. This category includesatopic <strong>foot</strong> dermatitis, nummular<strong>foot</strong> dermatitis, juvenile plantar dermatosisand <strong>the</strong> pompholyx-dyshidrosisspectrum. In many cases, <strong>the</strong> diagnosis<strong>of</strong> endogenous dermatitis is one <strong>of</strong> exclusion,made only after a negative patchtest has been performed to help rule outallergic contact dermatitis.Acral papulosquamous entities maybe easily diagnosed if typical stigmataare seen elsewhere on <strong>the</strong> patient. However,if involvement is limited to <strong>the</strong>feet, <strong>the</strong>re can be significant morphologicoverlap with chronic eczematousprocesses. Acral psoriasis, palmoplantarpustulosis and pityriasis rubra pilarisfall into this category. In a study in<strong>the</strong> International Journal <strong>of</strong> Dermatology,70 patients suspected <strong>of</strong> having allergiccontact dermatitis <strong>of</strong> <strong>the</strong> <strong>foot</strong> underwentpatch testing; 30 were given a finaldiagnosis <strong>of</strong> psoriasis. 20Infectious entities <strong>of</strong> <strong>the</strong> feet aretypically less likely to be misdiagnosedas contact dermatitis, with one majorexception. Dermatophyte infection caneasily be missed and should always beconsidered in <strong>the</strong> differential diagnosis<strong>of</strong> a patient with a possible contact dermatitis<strong>of</strong> <strong>the</strong> <strong>foot</strong>.Hybrid dermatitis is a clinically usefulterm that takes into account <strong>the</strong> factthat many patients have multifactorialdisease. It is <strong>of</strong>ten <strong>the</strong> case that a patientmay be atopic with a component <strong>of</strong> irritantdermatitis and superimposed allergiccontact dermatitis. Utilizing <strong>the</strong>term “hybrid dermatitis” brings int<strong>of</strong>ocus <strong>the</strong> need to address all underlyingfactors to ensure clinical success. Similarto <strong>the</strong> endogenous group, this diagnosisis typically only made after <strong>the</strong> completion<strong>of</strong> a full work-up, including comprehensivepatch testing.Practical Aspects <strong>of</strong> Patch TestingAs discussed above, <strong>the</strong> differential diagnosis<strong>of</strong> <strong>foot</strong> dermatitis can be a challenge.Patch testing is <strong>the</strong> gold standardfor making <strong>the</strong> diagnosis <strong>of</strong> allergic contactdermatitis. Most patch test expertsadvocate an approach that utilizes anexpanded series, including testing components<strong>of</strong> <strong>the</strong> patient’s own <strong>foot</strong>wearand socks. <strong>The</strong> most common allergenshave been listed in Table 1.While management <strong>of</strong> ACD <strong>of</strong> <strong>the</strong><strong>foot</strong> can be challenging, <strong>the</strong> majority<strong>of</strong> patients should be able to attainsustained improvement or resolution<strong>of</strong> <strong>the</strong>ir symptoms if proper patch testingis carried out and relevant allergensare avoided. 12 To maximize <strong>the</strong> yield <strong>of</strong>patch testing, it is important to recognizewhich patterns <strong>of</strong> <strong>foot</strong> dermatitisare most likely to show relevant positivereactions. For example, <strong>the</strong> previouslymentioned “classic shoe dermatitis pattern”with dorsal <strong>foot</strong> involvement is <strong>the</strong><strong>foot</strong> pattern most likely to show relevantpositive reactions on patch testing. 21Conversely, some patterns are importantto recognize because <strong>of</strong> <strong>the</strong>ir relativelylow yield on patch testing. One suchpattern is symmetric involvement <strong>of</strong>both <strong>the</strong> central palms and plantar feet.This pattern is more likely to be an endogenouseczema or psoriasis and has alower yield on patch testing for relevantpositive reactions.It is also important to know how tointerpret positive results. For example,nickel is a commonly tested and frequentlypositive allergen, but <strong>the</strong> relevance<strong>of</strong> nickel allergy is somewhatunclear when considering <strong>foot</strong> dermatitis.Dimethylglyoxime-positive metalsnaps, fasteners, buckles or islets may berelevant in a patient with <strong>foot</strong> dermatitisand a positive patch test to nickel.Some reports also suggest that systemicnickel exposure in an allergic patientcan present as a dyshidrotic hand and<strong>foot</strong> eczema. 22,23 Outside <strong>of</strong> <strong>the</strong>se twosettings, a positive nickel patch test mayonly represent past sensitization withoutcurrent relevance. Similarly, a positivereaction to fragrance, neomycin,bacitracin or corticosteroid may or mayTable 3. ExPanded Shoe Series 15Allergen FocusAdhesivesp-tert-butylphenol-formaldehyde resinColophonyEpoxy ResinBenzoyl PeroxideDyesParaphenylendiamineDisperse Blue 106 or 124Rubber ComponentsBlack Rubber MixCarba MixMercaptobenzothiazole or Mercapto MixThiourea MixThiuram MixDithiodimorpholineLea<strong>the</strong>r Tanning AgentsPotassium DichromateGlutaraldehydeFormaldehydenot currently be relevant. Evaluation<strong>of</strong> relevance for allergens that are notcore components <strong>of</strong> <strong>foot</strong>wear like <strong>the</strong>above allergens requires that <strong>the</strong> presence<strong>of</strong> retained allergens be excluded.For example, odor-eliminating powdersand sprays may be a source <strong>of</strong> fragranceretention in <strong>foot</strong>wear. Similarly, topicalmedicaments are frequently applied to<strong>the</strong> feet and it is possible for <strong>the</strong>se medicamentsto become embedded into <strong>the</strong>sock and <strong>foot</strong>wear. 24,25When determining what allergensto test, a standard series to screen forcommon shoe allergens and occult allergens,such as those described in <strong>the</strong>previous paragraph, is useful. However,it is also important to expand testingbeyond this standard series. It has beenshown that, in 12.7% <strong>of</strong> patients with<strong>foot</strong> dermatitis, <strong>the</strong> NACDG standardseries failed to identify any relevantallergens. 14 This number <strong>of</strong> non-reactorsis reduced when testing includessamples taken directly from <strong>the</strong> patient’ssocks and shoes. 12,14 Samplescan be taken from <strong>foot</strong>wear with an8-mm punch, <strong>the</strong>reby yielding piecesequal in size to a standard 8-mm Finnchamber. In addition, it is <strong>of</strong>ten helpfulto utilize an expanded shoe series.A good series will adequately screenfor sensitivity to adhesives, dyes, rubbercomponents and lea<strong>the</strong>r tanningagents, which may not be included onsome standard series. Table 3 high-November 2012 | <strong>The</strong> <strong>Dermatologist</strong> ® | www.<strong>the</strong>-dermatologist.com 23
Allergen FocusTable 4. Additional ResourcesFor more information about suppliers who <strong>of</strong>fer preparedexpanded shoe series for patch testing, <strong>the</strong> followingresources may be helpful.1. Allergeaze is an international company that <strong>of</strong>fersindividual & series allergens, patch-test chambers andancillary products. <strong>The</strong>ir website, www.allergeaze.com,can be accessed in English, German and Japanese.2. Chemotechnique is <strong>the</strong> self-described “world leaderin patch testing.” For information about <strong>the</strong>ir products,distributors and more, visit www.chemotechnique.se.3. Dormer Laboratories, Inc. <strong>of</strong>fer information on sites andsources <strong>of</strong> allergen exposure, patch test kits and more.Visit www.dormer.ca/Phy_Pages/PatchTesting.aspx tolearn more.lights an example <strong>of</strong> an expanded shoeseries for patch testing. Several suppliers<strong>of</strong>fer prepared expanded shoe seriesfor patch testing; for more information,see Table 4.Pearls <strong>of</strong> Treatment: Every Dose CountsAs alluded to in <strong>the</strong> preface, one maybe exposed to, and subsequently sensitizedto, a contact allergen like chromatesin shoes for days to years beforedemonstrating <strong>the</strong> clinical picture <strong>of</strong>ACD. With every exposure, <strong>the</strong>re is anincreasing risk <strong>of</strong> reaching a point atwhich <strong>the</strong> immune system meets itsmetaphorical “threshold” and subsequentexposures at this point can lead toelicitation <strong>of</strong> a cutaneous response, suchas <strong>foot</strong> dermatitis. 4,26 Just as repeatedcontact over time led to this immuneresponse, repeated avoidance will be requiredto induce remission.Avoidance <strong>of</strong> specific allergens in<strong>foot</strong>wear can prove to be a tedioustask; however, <strong>the</strong>re are programsavailable to aid in this endeavor. Both<strong>the</strong> Contact Allergen ManagementProgram (CAMP), 27 a service <strong>of</strong>feredthrough <strong>the</strong> American Contact DermatitisSociety (ACDS), and <strong>the</strong> ContactAllergen Replacement Database(CARD), 28 developed by Mayo Clinic,allow a provider to enter a patient’sknown contact allergens and producea “shopping list” <strong>of</strong> products void <strong>of</strong>those particular chemicals. <strong>The</strong> programscan also exclude cross-reactors.<strong>The</strong>se services are particularly invaluablein <strong>the</strong> case <strong>of</strong> occult shoe andsock allergens from retained personalproducts or topical medicaments.Ano<strong>the</strong>r valuable resource availablethrough <strong>the</strong> ACDS is <strong>the</strong> Hand andFoot Dermatitis Alternatives section. 18This information is accessible through<strong>the</strong> ACDS website and includes informationon management pearls. Severalcompanies who <strong>of</strong>fer hypoallergenic<strong>foot</strong>wear are also listed. nDr. Sheehan is with <strong>the</strong> departments <strong>of</strong>dermatology at Indiana University School <strong>of</strong>Medicine and Richard L. Roudenbusch VeteransHospital in Indianapolis, IN, and DermatologyPhysicians, Inc in Columbus, IN.Disclosure: Dr. Sheehan has no conflicts <strong>of</strong> interestto disclose.References1. Bickers DR, Lim HW, Margolis D, et al. <strong>The</strong>burden <strong>of</strong> skin diseases: 2004 a joint project <strong>of</strong><strong>the</strong> American Academy <strong>of</strong> Dermatology and <strong>the</strong>Society for Investigative Dermatology. J Am AcadDermatol. 2006;55(3):490-500.2. Hsu JW, Matiz C, Jacob SE. Nickel allergy: Localized,id and systemic manifestations in children.Pediatr Dermatol. 2011;28(3):276-280.3. Salam TN, Fowler JF Jr. Balsam-related systemiccontact dermatitis. J Am Acad Dermatol.2001;45(3):377-81.4. Nijhawen RI, Matiz C, Jacob SE. Contact dermatitis:From basics to allergodromes. Pediatr Ann.2009;38(2):99-108.5. Militello G, Jacob SE, Crawford GH. <strong>Allergic</strong>contact dermatitis in children. Curr Opin Pediatr.2006;18(4):385–390.6. Valks R, Conde-Salazar L, Cuevas M. <strong>Allergic</strong>contact urticaria from natural rubber latex inhealthcare and non-healthcare workers. ContactDermatitis. 2004;50(4):222-224.7. Walsh ML, Smith VH, King CM. Type 1 andtype IV hypersensitivity to nickel. Australas J Dermatol.2010; 51(4):285-286.8. Gimenez-Arnau A, Maurer M, De La CuadraJ, Maibach H. Immediate contact skin reactions,an update <strong>of</strong> Contact Urticaria, Contact UrticariaSyndrome and Protein Contact Dermatitis-- “A Never Ending Story.” Eur J Dermatol.2010;20(5):552-562. Epub 2010 Aug 23.9. Shackelford KE, Belsito DV. <strong>The</strong> etiology<strong>of</strong> allergic–appearing <strong>foot</strong> dermatitis: A 5-yearretrospective study. J Am Acad Dermatol. 2002;47(5):715–721.10. Holden CR, Gawkrodger DJ. 10 years’ experience<strong>of</strong> patch testing with a shoe series in 230patients: Which allergens are important? ContactDermatitis. 2005;53(1):37–39.11. Nardelli A, Taveirne M, Drieghe J, et al. <strong>The</strong>relation between <strong>the</strong> localization <strong>of</strong> <strong>foot</strong> dermatitisand <strong>the</strong> causative allergens in shoes: A 13-yearretrospective study. Contact Dermatitis. 2005;53(4):201–206.12. Freeman S. Shoe dermatitis. Contact Dermatitis.1997;36(5):247–51.13. Lynde CW, Warshawski L, Mitchell JC.Patch test results with a shoewear screeningtray in 119 patients, 1977-80. Contact Dermatitis.1982;8(6):423–425.14. Warshaw EM, Schram SE, Belsito DV, et al.Shoe allergens: Retrospective analysis <strong>of</strong> crosssectionaldata from <strong>the</strong> North American ContactDermatitis Group, 2001–2004.” Dermatitis.2007;18(4):191-202.15. Rietschel RL, Fowler JF, Fisher AA. “Chapter18.” In: Fisher’s Contact Dermatitis. Philadelphia, PA:Lippincott Williams & Wilkins, 2001. 356-69.16. Taylor JS, Erkek E, Podmore P. Shoes. In: Rycr<strong>of</strong>tRJG, Menne´ T, Frosch PJ, Lepoittevin JP,editors. Contact Dermatitis. 3rd ed. Berlin: Springer;2006. 751–766.17. Malten KE, Rath R, Pastors PH. p-tert-Butylphenolformaldehyde and o<strong>the</strong>r cause <strong>of</strong> shoe dermatitis.Derm Beruf Umwelt. 1983;31(5):149–53.18. American Contact Dermatitis Society. ACDSHand and Foot Dermatitis Alternatives. . Availableat: http://www.contactderm.org/files/public/FOOTDERMATITIS.pdf. Accessibility verifiedOctober 15, 2012.19. James WD, Berger TG, Elston DM, Odom RB.Andrews’ Diseases <strong>of</strong> <strong>the</strong> Skin: Clinical Dermatology.Philadelphia: Saunders Elsevier, 2006.20. Rani Z, Hussain I, Haroon TS. Common allergensin shoe dermatitis: Our experience in Lahore,Pakistan. Int J Dermatol. 2003:42(8):605–607.21. Lazzarini R, Duarte I, Marzagão C. Contactdermatitis <strong>of</strong> <strong>the</strong> feet: A study <strong>of</strong> 53 cases. Dermatitis.2004:15(3):125–130.22. Veien NK, Hattel T, Laurberg G. Low nickeldiet: An open, prospective trial. J Am Acad Dermatol.1993;29(6):1002–1007.23. Veien NK, Hattel T, Justesen O, Nørholm A.Dietary treatment <strong>of</strong> nickel dermatitis. Acta DermVenereol. 1985;65(2):138–142.24. Nedorost S, Kessler M, McCormik T.Allergens retained in clothing. Dermatitis.2007;18(4):212–214.25. Rietschel RL. Role <strong>of</strong> socks in shoe dermatitis.Arch Dermatol. 1984;120(3):398.26. Jacob SE, Herro EM, Taylor J. “Contact Dermatitis:Diagnosis and <strong>The</strong>rapy.” In: Elzouki AY,et al., eds. Textbook <strong>of</strong> Clinical Pediatrics, PediatricDermatology Section, 2nd Edition. Springer-Verlag,Berlin Heidelberg, 2012; Volume 3, Section 9,1467-1476.27. ACDS CAMP. American Contact DermatitisSociety. 2011. Available at: http://www.contactderm.org/i4a/pages/index.cfm?pageid=3489.Accessibility verified October 15, 2012.28. CARD: Contact Allergen ReplacementDatabase. 2012. Available at: http://www.preventice.com/card/.Accessibility verified October15, 2012.Sharon E. Jacob, MDDr. Jacob, <strong>the</strong> SectionEditor <strong>of</strong> Allergen Focus,is Associate ClinicalPr<strong>of</strong>essor <strong>of</strong> Medicine andPediatrics WOS (Dermatology)at <strong>the</strong> University<strong>of</strong> California, San Diego.Disclosure: Dr. Jacob is an investigator for SmartchoiceUSA PREA-2 trial.24 November 2012 | <strong>The</strong> <strong>Dermatologist</strong> ® | www.<strong>the</strong>-dermatologist.com