AHA/ASA Guideline Guidelines for the Prevention of Stroke in ...
AHA/ASA Guideline Guidelines for the Prevention of Stroke in ...
AHA/ASA Guideline Guidelines for the Prevention of Stroke in ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
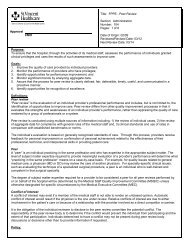
230 <strong>Stroke</strong> January 2011Table 2.Def<strong>in</strong>ition <strong>of</strong> Classes and Levels <strong>of</strong> Evidence Used <strong>in</strong> <strong>AHA</strong> RecommendationsClass IClass IIClass IIaClass IIbClass IIITherapeutic recommendationsLevel <strong>of</strong> Evidence ALevel <strong>of</strong> Evidence BLevel <strong>of</strong> Evidence CDiagnostic recommendationsLevel <strong>of</strong> Evidence ALevel <strong>of</strong> Evidence BLevel <strong>of</strong> Evidence CConditions <strong>for</strong> which <strong>the</strong>re is evidence <strong>for</strong> and/or general agreement that <strong>the</strong> procedure or treatment is useful and effectiveConditions <strong>for</strong> which <strong>the</strong>re is conflict<strong>in</strong>g evidence and/or a divergence <strong>of</strong> op<strong>in</strong>ion about <strong>the</strong> usefulness/efficacy <strong>of</strong> aprocedure or treatmentThe weight <strong>of</strong> evidence or op<strong>in</strong>ion is <strong>in</strong> favor <strong>of</strong> <strong>the</strong> procedure or treatmentUsefulness/efficacy is less well established by evidence or op<strong>in</strong>ionConditions <strong>for</strong> which <strong>the</strong>re is evidence and/or general agreement that <strong>the</strong> procedure or treatment is not useful/effective and<strong>in</strong> some cases may be harmfulData derived from multiple randomized cl<strong>in</strong>ical trials or meta-analysesData derived from a s<strong>in</strong>gle randomized trial or nonrandomized studiesConsensus op<strong>in</strong>ion <strong>of</strong> experts, case studies, or standard <strong>of</strong> careData derived from multiple prospective cohort studies us<strong>in</strong>g a reference standard applied by a masked evaluatorData derived from a s<strong>in</strong>gle grade A study, or one or more case-control studies, or studies us<strong>in</strong>g a reference standardapplied by an unmasked evaluatorConsensus op<strong>in</strong>ion <strong>of</strong> expertsparticipants with transient ischemic stroke, TIA, or <strong>in</strong>tracerebralhemorrhage (ICH) randomized from 3 weeks to 14 months after<strong>the</strong> <strong>in</strong>dex event and followed up <strong>for</strong> 2 to 5 years. No trials tested<strong>the</strong> effects <strong>of</strong> nonpharmacological <strong>in</strong>terventions.Overall, treatment with antihypertensive drugs was associatedwith significant reductions <strong>in</strong> recurrent strokes (relativerisk [RR], 0.76; 95% confidence <strong>in</strong>terval [CI], 0.63 to 0.92),MI (RR, 0.79; 95% CI, 0.63 to 0.98), and all vascular events(RR, 0.79; 95% CI, 0.66 to 0.95). 15 The impact <strong>of</strong> BPreduction was similar <strong>in</strong> <strong>the</strong> restricted group <strong>of</strong> subjects withhypertension and when all subjects, <strong>in</strong>clud<strong>in</strong>g those with andwithout hypertension, were analyzed. Larger reductions <strong>in</strong>systolic BP were associated with greater reduction <strong>in</strong> risk <strong>of</strong>recurrent stroke. The small number <strong>of</strong> trials limited comparisonsbetween antihypertensive medications. Significant reductions<strong>in</strong> recurrent stroke were seen with diuretics aloneand <strong>in</strong> comb<strong>in</strong>ation with ACEIs but not with -blockers orACEIs used alone; none<strong>the</strong>less, statistical power was limited,particularly <strong>for</strong> <strong>the</strong> assessment <strong>of</strong> -blockers, and calciumchannel blockers and angiotens<strong>in</strong> receptor blockers were notevaluated <strong>in</strong> any <strong>of</strong> <strong>the</strong> <strong>in</strong>cluded trials.S<strong>in</strong>ce this meta-analysis, 2 additional large-scale randomizedtrials <strong>of</strong> antihypertensive medications after stroke havebeen published: Morbidity and Mortality After <strong>Stroke</strong>, EprosartanCompared with Nitrendip<strong>in</strong>e <strong>for</strong> Secondary <strong>Prevention</strong>(MOSES), 24 and <strong>Prevention</strong> Regimen <strong>for</strong> Effectively Avoid<strong>in</strong>gSecond <strong>Stroke</strong>s (PRoFESS). 25 In MOSES, 1405 subjectswith hypertension and a stroke or TIA with<strong>in</strong> <strong>the</strong> prior 2 yearswere randomized to eprosartan (an angiotens<strong>in</strong> receptorblocker) or nitrendip<strong>in</strong>e (a calcium channel blocker). 24 BPreductions were similar with <strong>the</strong> 2 agents. Total strokes andTIAs (count<strong>in</strong>g recurrent events) were less frequent amongthose randomized to eprosartan (<strong>in</strong>cidence density ratio, 0.75;95% CI, 0.58 to 0.97), and <strong>the</strong>re was a reduction <strong>in</strong> <strong>the</strong> risk<strong>of</strong> primary composite events (death, cardiovascular event, orcerebrovascular event; <strong>in</strong>cidence density ratio, 0.79; 95% CI,0.66 to 0.96). A reduction <strong>in</strong> TIAs accounted <strong>for</strong> most <strong>of</strong> <strong>the</strong>benefit <strong>in</strong> cerebrovascular events, with no significant difference<strong>in</strong> ischemic strokes, and a more traditional analysis <strong>of</strong>time to first cerebrovascular event did not show a benefit <strong>of</strong>eprosartan. In PRoFESS, 20 332 subjects with ischemicstroke were randomly assigned to telmisartan or placebowith<strong>in</strong> 90 days <strong>of</strong> an ischemic stroke. 25 Telmisartan was notassociated with a reduction <strong>in</strong> recurrent stroke (hazard ratio[HR], 0.95; 95% CI, 0.86 to 1.04) or major cardiovascularevents (HR, 0.94; 95% CI, 0.87 to 1.01) dur<strong>in</strong>g mean 2.5-yearfollow-up. The BP-lower<strong>in</strong>g arm <strong>in</strong> PRoFESS was statisticallyunderpowered. Nonadherence to telmisartan and moreaggressive treatment with o<strong>the</strong>r antihypertensive medications<strong>in</strong> <strong>the</strong> placebo group reduced <strong>the</strong> difference <strong>in</strong> BP between <strong>the</strong>treatment groups (systolic BP differed by 5.4 mm Hg at 1month and 4.0 mm Hg at 1 year) and may have reduced <strong>the</strong>impact <strong>of</strong> treatment on stroke recurrence. Taken toge<strong>the</strong>r, aparticular role <strong>for</strong> angiotens<strong>in</strong> receptor blockers after strokehas not been confirmed.Recommendations1. BP reduction is recommended <strong>for</strong> both prevention <strong>of</strong>recurrent stroke and prevention <strong>of</strong> o<strong>the</strong>r vascularevents <strong>in</strong> persons who have had an ischemic stroke orTIA and are beyond <strong>the</strong> first 24 hours (Class I; Level <strong>of</strong>Evidence A).2. Because this benefit extends to persons with and withouta documented history <strong>of</strong> hypertension, this recommendationis reasonable <strong>for</strong> all patients with ischemicstroke or TIA who are considered appropriate <strong>for</strong> BPreduction (Class IIa; Level <strong>of</strong> Evidence B).3. An absolute target BP level and reduction are uncerta<strong>in</strong>and should be <strong>in</strong>dividualized, but benefit hasbeen associated with an average reduction <strong>of</strong> approximately10/5 mm Hg, and normal BP levels havebeen def<strong>in</strong>ed as