Report - LifeSciences BC
Report - LifeSciences BC
Report - LifeSciences BC
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
REPORT OF THE PHARMACEUTICAL TASK FORCETO THEHONOURABLE GEORGE ABBOTTMINISTER OF HEALTHPROVINCE OF BRITISH COLUMBIAAPRIL, 2008
April 10, 2008Honourable George AbbottMinister of HealthGovernment of British ColumbiaPO Box 9050, Stn Prov GovtVictoria, <strong>BC</strong> V8W 9E2Dear Minister Abbott:We have the honour to transmit herewith the <strong>Report</strong> of thePharmaceutical Task Force.It has been our privilege to undertake this challenging task. We hopeour conclusions will assist you and the Government of British Columbiain finding a constructive way forward with the evolution ofpharmaceutical policy in our Province.We would be pleased to make ourselves available to discuss our findingswith you in greater detail.Yours truly,Don AvisonChairON BEHALF OF THE PHARMACEUTICAL TASK FORCEGeorge L. Morfitt (Alternate Chair), Susan Paish, QC, Gordon Cross,Dr. Robert Sindelar, Paul Gudaitis, Russell Williams, David Hall,Dr. Mark Schonfeld.
Table of ContentsTask Force Mandate and Membership . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1Managing PharmaCare: The <strong>BC</strong> Context. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2The Role and Objectives of the Pharmaceutical Services Division . . . . . . . . . . . . . . 2Increased Demand and Rising Costs. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3Optimization of the Decision-Making Process for the Listing of Pharmaceuticals. . . . . . . 6Proposed Modifications to the Drug Benefit Committee. . . . . . . . . . . . . . . . . . . . . 10A New Approach to Drug Reviews in British Columbia. . . . . . . . . . . . . . . . . . . . . . 11Recommendations for an Improved Listing Process. . . . . . . . . . . . . . . . . . . . . . . . . 14Procurement and Service Delivery Options . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15Generic Drugs – Call for a Fundamental Shift . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16The Role of Pharmacy. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19More Direct Engagement with Innovative Drug Manufacturers. . . . . . . . . . . . . . . . 20Increased Utilization of Tendering Processes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21Recommendations Regarding Procurement Options . . . . . . . . . . . . . . . . . . . . . . . . 22Building Constructive Relationships . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23The Common Drug Review. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23The Therapeutics Initiative. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25Summary of Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 27SCHEDULE A – Pharmaceutical Task Force Project Charter . . . . . . . . . . . . . . . . . . . . . 30
Task Force Mandate and MembershipIn November, 2007 the Minister of Healthestablished a Pharmaceutical Task Force andinvited recommendations regarding how theMinistry of Health could achieve progress in thefollowing areas:1. optimization of the decision making processfor the listing of pharmaceuticals anddevices to produce timely, transparentdecisions based upon sound science whileappropriately protecting the public interest;2. procurement and service delivery optionsfor pharmaceuticals and medical devicesthat will achieve and maximize value topatients and value for money objectives;3. identification and strengthening of commonobjectives related to patient care and choiceand the building of positive relationsbetween government decision makers andindustry to achieve those objectives;4. the effectiveness of the Common DrugReview process and proposals forimprovements;5. the effectiveness, transparency and futurerole of the Therapeutics Initiative insupporting the listing process of drugs, or amore viable and cost-effective alternative.The membership of the Task Force includedsenior industry representatives from the patentmedicine, medical device and retail pharmacycommunities, the Dean of the Faculty ofPharmaceutical Sciences at the University ofBritish Columbia, the Chief Executive Officer ofthe <strong>BC</strong> Medical Association, two seniorrepresentatives of the Ministry of Health, theformer Auditor General of British Columbia(Alternate Chair) and the President of theUniversity Presidents' Council (Task ForceChair). The Project Charter established to guidethe work of the Task Force is reproduced atSchedule 'A' to this <strong>Report</strong>.The Task Force met on nine occasions fromDecember of 2007 through to late February of2008. Submissions were received from, and inmost cases the Task Force met with, the <strong>BC</strong>Pharmacists Association, the Canadian GenericPharmaceutical Association, the Canadian1Association of Chain Drug Stores, Rx&D ,MEDEC (Canada's Medical Device TechnologyCompanies), the Better PharmaCare Coalition,the Canadian Diabetes Association and the seniorleadership of the research components of theVancouver Coastal Health Research Institute, theChild and Family Research Institute (ProvincialHealth Services Authority), the ProvidenceHealth Care Research Institute and the SeniorAssociate Dean, Research of the Faculty of2Medicine at the University of British Columbia.1The entity which represents Canada's research-based pharmaceutical companies.2The Dean of Medicine, subsequently made himself available to the Task Force to offer further commentary andclarification, particularly with respect to the operations and accountabilities associated with the TherapeuticsInitiative housed within the Faculty of Medicine.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 1APRIL, 2008
In addition to the submissions from thegroups mentioned above, the Task Force metwith representatives of the National CommonDrug Review (video conference) and U<strong>BC</strong>'sTherapeutics Initiative, with the AssistantDeputy Minister in the Ministry of Healthresponsible for administration of thePharmaceutical Services Division (PSD) and theExecutive Director of the Drug Intelligence unit ofthe PSD.The Task Force also heard from Dr. ChrisCorbett of CSCW Systems Corporation (CSCW)who was made available by the Ministry of Healthto discuss the content of a Ministry-sponsoredreview CSCW conducted in respect of the3Province's PharmaCare program in 2003/4.Managing Pharmacare: The <strong>BC</strong> Context1. The Role and Objectives of thePharmaceutical Services DivisionThe Task Force met first with the AssistantDeputy Minister and the Executive Director ofthe Drug Intelligence Unit of the PSD to receivea comprehensive overview of the PSD'sapproach to the administration of pharmaceuticalpolicy, the processes applicable to the evidencebasedreview of submissions for the listing ofnew drug therapies in <strong>BC</strong>, cost pressures facedby the PharmaCare program and on othercomplex factors which influence theenvironment that program administrators andpolicy makers work within. The discussion withsenior representatives of the PSD addressed:the PSD's Mission, Goals and Objectives;baseline information about thepharmaceutical distribution environmentin <strong>BC</strong>;the nature of <strong>BC</strong>'s drug review processesincluding the respective roles of the PSD,the Drug Benefit Committee, theTherapeutics Initiative and how <strong>BC</strong>interacts with related external processessuch as the national Common Drug Review(CDR) and the Patented Medicine PricesReview Board (PMPRB);the demands on the PSD to effectivelymanage the rising costs associated with thePharmaCare program;the impact cost pressures have ondecisions regarding the province'sformulary management system; andstrategies which have been – or likely willbe – deployed to further contain the cost ofpharmaceutical products eligible forreimbursement under British Columbia'sPharmaCare program.3“Findings of the CSCW Review of PharmaCare”, May 2004.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 2APRIL, 2008
The Task Force was informed that the PSDis the product of a substantial reorganization ofwhat had been the Ministry of Health'sPharmaCare Division. These changes, whichhave added substantial new human resourcecapacity to the PSD were, at least in part,responsive to recommendations set out inprevious reports of the Auditor General, (see:“Managing PharmaCare: Slow Progress TowardCost-Effective Drug Use and a SustainableProgram”, March, 2006) and the CSCW Reviewof PharmaCare.The reorganization of the PharmaCareDivision into the substantially more robust PSDhas helped to resolve concerns about the levelof human resources available to the programand also appears to have diminished the level ofsenior staff turnover. The reorganization hasfacilitated the appointment of five executivedirectors with responsibility for DrugIntelligence, Drug Use Optimization, PolicyOutcomes/Evaluation, BusinessManagement/Supplier Relations and the conductof <strong>BC</strong>'s role as a lead jurisdiction with theNational Pharmaceutical Strategy. Theseadditional resources, together with the nature ofthe reorganization of the entity provides room4for optimism that the Ministry of Health willhave the human capacity to be able to addressthe partnership-based engagement strategiesthat this Task Force views as vital to the longertermsustainability of the pharmaceuticalmanagement system in British Columbia.The stated mission of the newly constitutedPSD is to “advance the health of BritishColumbians by supporting optimal drugtherapy.” This mission is guided by the followingcore goals:Goal One – Support citizens to have thebest possible health;Goal Two – Develop the bestpharmaceutical system in the world; andGoal Three – Create the best place towork, with the best people.Support to patients, the provision of highquality unbiased information to healthprofessionals, access to comprehensive drugbenefit programs, acquisition of “the best drugsat the best prices”, the importance ofsustainability, effective stakeholder engagement,continuous improvement, enhanced patientcare and safety were profiled as significantobjectives linked to the PSD's core goals.2. Increased Demand and Rising CostsMuch of the PSD presentation to the TaskForce focused on the cost and budgetingpressures faced by the PharmaCare program.This is not surprising given the extent to whichspending increases within provincial4This includes plans for the hiring of further staff to carry out the expanded mandate of the PSD.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 3 APRIL, 2008
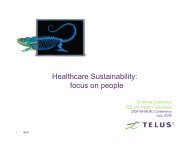
pharmaceutical coverage programs have been5trending in recent years. At the national level,government-supported expenditures onpharmaceutical products now account for 9.6%of health-related spending (see Figure One).The numbers in British Columbia aresomewhat different. <strong>BC</strong> continues to spendless, per capita, than the Canadian average onprescription drugs (based on data available from2006, <strong>BC</strong>'s expenditure level stood at $466 perperson while the national average was $598). Itis important to note, however, that <strong>BC</strong> isexperiencing the highest growth rate in thenumber of new prescriptions (11.4% against anational average of 8.6%) and the third highestgrowth rate in the dollar value of prescriptions.When looked at over the longer term, <strong>BC</strong> hasseen a substantial increase in the cost of6prescription drugs over the past decade. In1996 the province's PharmaCare programspent $372 million on prescription drugs. Theamount increased to $713 million by 2004 andFigure One: Government health expenditure (GHEX) in Canada,1975 to 2005, by use of funds60,00050,000Hospitals & institutionsMillions Current $CDN40,00030,00020,000Professionals10,000Prescription drugs(patented & non-patented)01975 1978 1981 1984 1987 1990 1993 1996 1999 2002 2005Source: Canadian Institute for Health Information (CIHI), 2005Other5Some caution may be required when considering, in isolation, increased costs in pharmaceutical coverage programs. Itis now well established that increased drug expenditures may simply indicate that drug therapies have been successfullydeployed in a manner that may help to alleviate pressures on other aspects of the healthcare system. The BritishColumbia Medical Association in “A Prescription for Quality; Improving Prescription Drug Policy in British Columbia, (July,2007 – see p.14), said this: “As in any area of public policy, increased spending may be a prudent investment, with gains tobe realized in the future. For example, clinical guidelines and chronic disease management programs have increasinglyemphasized drug therapy as a cornerstone to improving health outcomes and controlling costs. Multiple clinical trialssuggest that use of appropriate heart failure drug therapies may be the most effective way to reduce the cost of carewhile reducing morbidity and mortality: drug therapies can reduce hospitalization by 12% to 35%, depending on thedrug (Goldfarb, Weston et. al. 2004). Nonetheless, within finite budgets, increased spending in one area may also offsetexpenditures elsewhere in the healthcare system. The challenge for healthcare policymakers is to determine if and whenthe investment in prescription drugs – particularly in light of continued growth – is worth the expected return.”6This growth rate is substantially consistent with what has taken place in other provinces and other national jurisdictions.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 4APRIL, 2008
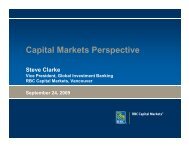
climbed further to more than $900 million forthe 2006/07 fiscal year (see Figure Two).PSD representatives indicated that, facedwith these rising cost pressures, they are lookingat measures to reduce costs and, thereby, tolimit the otherwise predictable trajectory ofspending on pharmaceutical products. WhilePSD representatives were less precise on thispoint in their discussions with the Task Force,7they have indicated in other fora an intention to8realize “projected savings” of $214 million by2010 through a combination of:product agreements with manufacturers ofinnovative drug therapies that will result in“the negotiation of better terms”;cost savings from addressing the linkbetween generic drug rebate programs andretail pharmacies;the increased utilization of tenderingprocesses; andhealth promotion initiatives intended toencourage more appropriate and effectivedrug use by patients.These options, and the sensitiveimplementation issues associated with them, willbe addressed in greater detail later in thisreport.Figure Two: PharmaCare Plan Expenditures ($ millions)Includes both Pharmacare plan and program management expenditure$1,000$900$800$700$600$500$400$300$200$100$01995/95 1996/97 1998/99 2000/01 2002/03 2004/05 2006/07The Ministry of Health and the PSD areright to be concerned about risingpharmaceutical costs. It should be mentionedhere, however, that – with few exceptions – allwho participated in the Task Force processrecognized that affordability and value formoney are, and will remain, key factors thatthose responsible for government'spharmaceutical reimbursement programs mustconsider in making the difficult decisionsregarding whether new drug therapies will belisted for coverage on the provincial formulary.There was also a strong and comprehensiverecognition by most presenters that while thecost of pharmaceuticals must be a key factor,so too must be choice, availability, reliability ofsupply and patient outcomes. Ignoring any of7“Pharmaceutical Policy Reform in British Columbia” (IMS, Provincial Reimbursement Advisor, Vol. 10, Issue 4,November, 2007).8A number of significant patent-protected drug therapies will come off patent in the near term. This factor, of itself,should help to alleviate cost pressures. Encouraging the innovative drug manufacturers to more fully participate in thepost-patent context would be prudent.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 5APRIL, 2008
these factors may potentially result in increasedcosts to the system in the short and long termand adverse patient outcomes. As you will seefrom what follows, the key concerns frompatient groups, from health care practitionersand from industry focused on what is perceivedas an insufficient commitment by the PSD toopenness, transparency and meaningful dialogueon matters of shared interest and concern.Issue One: Optimization of the decisionmakingprocess for the listing ofpharmaceuticals and devices to producetimely, transparent decisions based uponsound science while appropriately protectingthe public interest.During the course of the submissionsprocess several concerns were raised regardingBritish Columbia's existing approach to thelisting of pharmaceuticals and other healthrelatedproducts. The Task Force heardrepeatedly that, despite the increasedadministrative capacity within the PSD, thelisting process remains cumbersome,unnecessarily insular and less efficient than itshould be in providing patients with timelyaccess to coverage for new drug therapies.Industry, particularly those representing theinterests of patented drug manufacturers,enumerated a number of concerns including thefollowing:that the current <strong>BC</strong> process is unreasonablyslow, both by national and by internationalstandards;that British Columbia provides “full listings”for fewer new therapies than otherprovincial jurisdictions and generally takesmuch longer to list;that industry believes they have apartnership role to play “as part of thesolution” to sustainability but that they havefound the PSD to be non-responsive in thisregard. The absence of a constructive andtransparent environment limits the extentof significant international industry9investment in <strong>BC</strong> ;that, despite British Columbia's lead role incalling for a national Common Drug Reviewto improve the quality and efficiency oflisting decisions, <strong>BC</strong>'s average “time tolisting” increased significantly following10CDR implementation ;9For example, it is almost certainly the case that the level of investment by industry in the British Columbia CancerAgency is more modest than what it would be in a more stable environment that placed greater weight on theimportance of innovation.10It must be noted, however, that time to listing decisions, while they remain longer than the national average, havebegun to improve over the past year. The Task Force notes that the quality of the available data in this area is modestand it would be useful to have the benefit of a better mechanism to independently assess <strong>BC</strong>'s time-to-listingperformance to help facilitate continuous quality improvement.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 6 APRIL, 2008
the 'silo' approach to PSD budgets does notadequately address, or relate to, thepositive impact that effectivepharmaceutical treatment and expenditurescan have on limiting expenses in other areasof the healthcare system; andthat the existing process for listing givesinsufficient weight to the value of innovationand essentially none to economic11development factors.12The Better PharmaCare Coalition (<strong>BC</strong>P)and the Canadian Diabetes Association (CDA)articulated even stronger views. The <strong>BC</strong>P madethe following observations andrecommendations:patients believe they are being deniedoptimal therapy because PharmaCarecoverage is restricted to “least expensive”or “best deal” drugs and devices withoutsufficiently considering the impact on healthoutcomes of the lowest cost products;that the overlap and duplication innational/provincial drug review and listingprocesses should be substantiallyrationalized with the objective ofsignificantly improving “time to listing”13decisions;<strong>BC</strong> should establish a quick and effectiveprocess at the provincial decision-makinglevel for all drugs/indications that do not fallwithin the scope of the Common DrugReview (includes 'line extensions' or 'newindications' in respect of previouslyapproved drugs);the decision-making processes regardinglisting should be open, transparent andinclusive with an increased role for patientengagement and for the participation ofdisease specialists;specific action should be taken to addressthe disproportionately higher costs paid forgeneric drugs in British Columbia relative towhat is paid in other jurisdictions with“savings” re-directed to investments in newinnovative drugs that “merit listing on the<strong>BC</strong> PharmaCare drug reimbursement11Senior PSD staff confirmed that they do not consider economic development factors to fall within their mandate. Thismay well be accurate but it must also be understood, given that all listing decisions are ultimately determined through thePSD, that this means broader economic factors beyond cost management of the PSD budget (e.g. prosperity andeconomic development indicators) are not addressed by anyone.12The Better PharmaCare Coalition represents the interests of Arthritis Consumer Experts, the Arthritis Society(<strong>BC</strong>/Yukon Division), <strong>BC</strong> Lung Association, <strong>BC</strong> Schizophrenia Society, Canadian Arthritis Patients Alliance, CanadianSociety of Intestinal Research, Canadian Association of Retired Persons, Heart and Stroke Foundation (<strong>BC</strong>/Yukon), theKidney Foundation of Canada (<strong>BC</strong>), Mood Disorders Association of <strong>BC</strong>, MS Society (<strong>BC</strong> Division), Parkinson Society ofBritish Columbia and the Osteoporosis Society of Canada (<strong>BC</strong> Division).13The BPC proposes that British Columbia should complete formulary listing decisions not more than three monthsfollowing a “recommendation to list” from the Common Drug Review.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 7 APRIL, 2008
14formulary”; and<strong>BC</strong> should benchmark the cost, efficiencyand effectiveness of the PharmaCareinfrastructure against the performance ofother jurisdictions.The Canadian Diabetes Association's (theCDA) submission made many points similar innature to those expressed by the BPC but calledfor PharmaCare to be renewed throughlegislation that would include the followingcomponents:stronger transparency and accountability bygiving patients a role in formulary listingdecisions;increased patient access to all safe andeffective medications, devices and suppliesavailable for sale in Canada;removal of unnecessary paperwork fordoctors;increased roles for pharmacists and theirexpertise in medication therapy and chronicdisease care;inclusion of the relevant disease experts indecisions on disease specific listings;responsiveness to the views of BritishColumbians on the social aspects of drugpolicies and priorities; andachievement of the greatest savingspossible for <strong>BC</strong> taxpayers by counting allcosts and benefits across the <strong>BC</strong>healthcare system from increasing accessto safe and effective medications, devicesand supplies.Other groups who participated in the TaskForce process made recommendations thatwere focused on strengthening the recognitionof health and life sciences research as keydrivers of improved health outcomes. Thisview was strongly articulated by the seniorrepresentatives of the Vancouver CoastalHealth Authority (VCHA), Providence HealthCare (Providence) and Provincial HealthServices Authority (PHSA) research instituteswho called for the development of what theydescribed as a “healthier climate” forincreased engagement of pharmaceuticalresearch and investment in British Columbiaand the development of a culture of innovationoriented towards improved health outcomesfor patients. These research experts contendthat the historical, and current, approaches tolisting decisions in <strong>BC</strong> have been unreasonably15restrictive in this regard.14The high cost of generic drugs in British Columbia, and options to address this, is considered later in this report, (seepages 16-19). It should be observed, however, that some Task Force members were struck by how little attention thisarea of potentially substantial savings has received compared the province's Reference-Based Pricing program where thelevel of “savings” is relatively modest. (see: <strong>Report</strong> of the Reference Drug Program Consultation Panel to theHonourable Sindi Hawkins, Minister of Health Planning, British Columbia, April, 2002)15These research experts were particularly critical of what they regard as a narrow and restrictive approach used by theTherapeutics Initiative. They further suggest that the Therapeutics Initiative has been insulated from robust peer reviewexpected of academic organizations and from the rigours of competitive funding models.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 8 APRIL, 2008
The Task Force agrees and has concludedthat the current process for the evidence-basedreview of pharmaceutical products consideredfor listing in British Columbia can, and must, beimproved. With the process of reorganizing andstrengthening the Pharmaceutical ServicesDivision now substantially complete, priorityattention should be directed to the revitalization16of the drug review listing process and thisshould be carried out in a manner consistentwith government's objective of developing “thebest pharmaceutical system in the world.” In sodoing, a plan needs to be developed with a focuson addressing the timeliness of decision-making,the reduction of unnecessary duplication,improved transparency, the enhanceddeployment of a wider array of peer-respectedspecialized expertise and a meaningful andcredible commitment to stakeholderengagement.The need for a new, more responsive,system will become even more apparent as wemove towards a greatly enhanced level of“personalized medicine” where professionalswill be more able to select the most appropriatedrug for particular genotypes of patients. Thistrend towards use of “the right drug, at the righttime for the right patient” could, if managedproperly, have a very significant impact on levelsof hospitalization, the reduction of adverse drugreactions and improved quality of life forpatients suffering from chronic illnesses. Theseoutcomes will not only produce tangibleimprovements in patient outcomes, but byreducing demands on the health care systemcaused by ineffective or inappropriate drugs,will also have an impact on the overall costs ofthe health care system. Experts agree that, inthe future, there will be less emphasis on“blockbuster, one-size fits all” therapeutics as agreater number of therapies will be targeted tomore specifically meet the needs of particularpatient groups. This will require a much morerobust approach to evidence-based evaluation,to listing decisions and to the relatedmanagement of pharmaceutical expenditures.Many of the changes the PSD has made throughtheir recent reorganization have the potential, ifmanaged wisely, to provide the foundationnecessary to respond to these anticipatedchanges.The Task Force was not persuaded thatmodifications to the PharmaCare program, orto the listings process, can only be achievedthrough legislation, nor that reimbursementshould be made available in respect of “all safeand effective medications, devices and suppliesavailable for sale in Canada.” On the contrary,we believe any necessary changes to the reviewand listing process can best be achieved through16This proposal is not new. The March, 2004 CSCW Review of PharmaCare had identified “an urgent need for theimplementation of a comprehensive, transparent, administrative system for the generation and ongoing managementof the PharmaCare Formulary.” That review recommended the development of a new Formulary ManagementSystem that would engage the participation of stakeholders and strengthen the role of PharmaCare (now the PSD)as the “system integrator.”THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 9 APRIL, 2008
meaningful engagement with stakeholders, theuse of the very best evidence and through clearpolicy direction from government.On the cost side, value for money andsustainability will continue to be core guidingprinciples. Program administrators with thePSD will be required, as they are now, to makedifficult decisions regarding which therapies andproducts will, or will not, be listed for coverageunder the provincial formulary. These decisions,however, can – and should – be informed by asubstantially enhanced level of engagement withknowledgeable disease specialists, with otherhealth professionals, with patientrepresentatives and with industry. Thisincreased commitment to engagement ofstakeholder interests in the drug review andlisting process will also be central to theimplementation of more effective strategies toimprove drug utilization management. Thegreatest opportunities for sustainable innovationin the system will likely occur at the intersectionof diverse thought that may come from sucheffective engagement.Proposed Modifications to the DrugBenefit CommitteeAt present, one of the most significant rolesin <strong>BC</strong>'s listing process is carried out by the DrugBenefit Committee (D<strong>BC</strong>), an arm's lengthentity that provides advice to government onwhether, and to what extent, drug therapiesshould be listed for coverage under thePharmaCare program. The Task Force sees therole of the D<strong>BC</strong> as key to the management ofan effective and respected program but wouldoffer a number of recommendations regardingproposed improvements in respect of themembership, transparency and operations ofthe D<strong>BC</strong>.It is important to note that the Ministry ofHealth and the PSD have already recognizedthat changes to the membership of the D<strong>BC</strong> areboth necessary and appropriate. Prior to theinitiation of the Task Force process the PSDalready had plans to move ahead with theappointment of a public member to the D<strong>BC</strong>.Action to address this issue was held inabeyance awaiting the outcome of the work ofthis Task Force.The Task Force is of the view thatgovernment's intention to expand, or alter, D<strong>BC</strong>membership to increase the level of publicengagement is appropriate but the addition of asingle public member will not be sufficient tomeet that goal. The appointment of not lessthan three public members, selected through a17process external to the PSD , would be bothmore appropriate and consistent with what theMinistry of Health has already done withrespect to the governance of the Medical18Services Commission. This step would bemore compatible with modern governancepractices, would provide for increased publicand patient engagement and would substantially17The Board Resourcing Office may be the most appropriate agency to carry out this role.18The appointment process would be different in nature than the one currently in place for the Medical ServicesCommission.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 10 APRIL, 2008
assist in addressing accountability andtransparency expectations. In addition, the TaskForce recommends that the D<strong>BC</strong> should bereconstituted as the “Drug Benefit Council” tomore appropriately reflect the arms length19position it is expected to play.The D<strong>BC</strong> could also benefit from lookingmore closely at some of the operational reformswhich have been implemented by the nationalCommon Drug Review following externalreviews conducted in respect of that entity. TheCDR has put in place timeline expectations andhas increased “feedback loops” with industryregarding their submissions and with clinicians toensure they have the benefit of the fullinformation necessary to assist them inproviding the best possible advice to provinces.The Task Force also notes that the D<strong>BC</strong>could be further strengthened if at least one ofthe public members has broad economicexpertise to supplement existing economiccapacity currently limited to the more narrow20discipline of health economics.A New Approach to Drug Reviews inBritish ColumbiaDuring the course of the Task Force processconsiderable discussion was dedicated towhether British Columbia could – or should –develop a new approach to more effectivelysupport the work of the Drug BenefitCommittee.While the Therapeutics Initiative has servedan important role in the past it is now widelyregarded as being in need of either substantialrevitalization or replacement. The Task Forceregards replacement as the better option. TheTask Force consistently heard that the existingprovincial review processes and, morespecifically, the Therapeutics Initiative, confinereview to a relatively small community of21experts and, as a result, the array of potentialexpertise that could be deployed to considerthe merits of listing submissions is not as broad,nor as deep, as it ought to be.A session with the senior leadership of theTherapeutics Initiative, despite impressive19This would also help to better differentiate the roles of the D<strong>BC</strong> and the DRRC.20One of the three proposed public positions on the D<strong>BC</strong> could be utilized to add this capacity.21The Therapeutics Initiative has seen relatively modest staffing turnover and several of the newer participants weretrained within the program. The existing PSD approach to conflict of interest guidelines are also so restrictive in thatthey exclude participation by disease-specific specialists who likely have the most to offer on the potential value of newtherapies. An expanded approach would facilitate the engagement of expertise of other entities including, but not limitedto, the Centre for Applied Health Research, the Centre for Infectious Inflammatory and Immunologic Disease, the Centrefor Molecular Medicine and Therapeutics and other highly regarded academic groups.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 11 APRIL, 2008
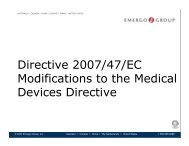
contributions from Drs. Ken Bassett and ColinDormuth, did not leave the Task Force with thecomfort necessary to suggest that theTherapeutics Initiative is well-positioned tomeet the current and future public interestneeds of the province. Accordingly, werecommend a new approach that wouldsubstantially increase the level of expertiseavailable to support effective and timely drug22reviews , increase transparency and improvethe quality of information required to properlysupport the role of the D<strong>BC</strong>.The proposed new approach wouldestablish a Drug Review Resource Committeethat would be responsible for the maintenance23of a much larger open registry of experts toparticipate in Drug Coverage Review Teams (seeChart One). These DCRT's, with expertiseappropriate to the therapeutic area underconsideration, would critically review theapplicable literature, clinical studies, submissionsand, where applicable, reports of the CommonDrug Review in order to provide the D<strong>BC</strong> and,ultimately, the PSD with the best possible advice– both therapeutic and economic – as towhether a product should be listed forcoverage. This proposed mechanism, which issubstantially based upon <strong>BC</strong>'s panel-basedutilization of experts similar to what exists in theprovincial labour relations context, would alsoprovide for the increased participation ofdisease-specific experts, a group that the TaskForce views as an underutilized asset in the24current decision-making process.The Task Force also suggests that arevitalized process should also make provisionfor a greater degree of pre-submission andpost-submission engagement between PSD staffand industry applicants to ensure thatsubmissions are as complete as possible and, inaddition, to substantially improve budget impactinformation that the D<strong>BC</strong> and the PSD willrequire in order to make the most appropriaterecommendations and decisions possible. Theintroduction of an appeal mechanism would alsobe a useful addition for Government to considerin working towards an improved process.22Maintaining the requirement for the input of therapeutic and clinical expertise in the review process will remainimportant. In this regard, it is anticipated that experts currently involved in work with the Therapeutics Initiative wouldbe encouraged to be active participants in the proposed new process.23The registry could also include participation by experts external to British Columbia.24Participation would be subject to compliance with appropriate conflict of interest guidelines.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 12 APRIL, 2008
DCRTSubmissionof FindingsChart One: Submission Review ProcessDRUG BENEFIT COUNCILBroad membership with relevant decision making expertise- transparent appointment process- robust conflict of interest terms for each member for each submission,including bias- proper governanceEstablishes Drug Review Resource Committee (DRRC)Reviews & recommends acceptance or rejection of DCRT findings to PSDDrug Review Resource Committee(Sub-committee of the D<strong>BC</strong>)Maintains open registry of experts; therapeutic indications, economics, clinical practiceMembership: 4 members from D<strong>BC</strong>, 1 year rotation plus PSD’s DIDSelect 5 experts for each drug file to sit on a Drug Coverage Review TeamDCRT DCRT DCRT DCRT DCRTDrug Coverage Review Teams (DCRT)Mandate:Review file for recommendation- critically review and appraise relevant literature- review manufacturers submission- review CDR file (if available)If required, gathers inputs from other sources, experts or stakeholdersMembership structure from DRRC Registry: Chair plus 4 team members<strong>Report</strong>s to the Drug Benefit CouncilD<strong>BC</strong>Recommendation toMinistry of HealthPSDDrugIntelligenceDirector(DID)Drug FileAllocationTHE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 13APRIL, 2008
Recommendations for an Improved Listing ProcessRecommendation One:Priority attention should be focused ondevelopment of an enhanced FormularyManagement System together withimproved stakeholder engagement andappeal mechanisms. This work shouldbe led by the Pharmaceutical ServicesDivision and include meaningfulengagement with stakeholders, includingpatients, healthcare professionals,disease specialists, research leaders andindustry.Recommendation Two:The Ministry of Health should act toestablish new target review/listingdecision guidelines with the goal ofsubstantially improving BritishColumbia's performance on time-tolistingdecisions. Progress on this frontmust be publicly reported andconsistently benchmarked against theperformance of other jurisdictions.Recommendation Three:The Drug Benefit Committee should bereconstituted as the “Drug BenefitCouncil” to more appropriately reflectthe arms length role it is expected tocarry out in the review processesapplicable to consideration of newtherapies.Recommendation Four:The Ministry of Health should establisha new Drug Review ResourceCommittee to carry out the drugsubmission review role currentlyperformed by the TherapeuticsInitiative. This new DRRC should alsoprovide for a registry of experts thatwill substantially widen the array ofexpertise available to offer advice andrecommendations on the therapeuticvalue and cost-effectiveness of newdrug therapies.Recommendation Five:The membership of the D<strong>BC</strong> shouldbe modified to include the participationof at least three public membersselected through a process external tothe PSD. Government may also wishto consider ensuring that at least onemember of the D<strong>BC</strong> has broadeconomic expertise to supplement theexisting expertise that is focused morenarrowly on health economics.Recommendation Six:No members of the TherapeuticsInitiative or, in the alternative, noparticipant in a Drug Coverage ReviewTeam should participate as members inthe work of the Drug Benefit Council.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 14 APRIL, 2008
Issue Two: Procurement and servicedelivery options for pharmaceuticals andmedical devices that will achieve andmaximize value to patients and value formoney objectives.It is important to note that all participants inthe Task Force process and, for the most part,those who provided submissions to the TaskForce, recognize the importance of sustainabilitypressures facing health care generally.Accordingly, the need for efficient and effectiveprocurement and service delivery options is wellunderstood.In exploring options for change the TaskForce considered:the current approach to acquisition andreimbursement policies that apply togeneric drug products;the fundamental role played by pharmacistsand pharmacies and the need to ensure thatany new approaches or policies regardingprocurement will not produce unintendedadverse consequences in the servicedelivery relationship between patients andpharmacists and also the pharmaceuticalsupply chain;the potential value of more directengagement and, where applicable,negotiation between the PSD and themanufacturers of patent-protected drugtherapies; andthe need for a cautious approach in theimplementation of possible costcontainmentstrategies including morerobust utilization of tendering processes.Effectively addressing any – or all – of theseareas will require a very substantial degree ofdirect and meaningful engagement by the PSDwith the various stakeholders whose interestswill be most deeply impacted by any changes toexisting arrangements. Patients must certainlybe at the forefront of any engagementprocesses, but the PSD will also need toundertake direct dialogue and, whereapplicable, negotiations with other partiesincluding the patent-protected/innovative drugmanufacturers, the generic drug companies,community pharmacy and the pharmacistprofession.While effective and meaningful engagementby the PSD will be essential, all parties mustunderstand that the sustainability pressuresfacing the PharmaCare program, and healthcare more generally, are very real. Governmentwill be compelled to act with a higher degree ofunilateralism unless the interested parties areable to create innovative more sustainableprocurement mechanisms and/or achieve areasonable degree of consensus onmodifications to pricing and procurement25options within a reasonable period of time.25The previously mentioned Corbett Review had called for this kind of engaged stakeholder negotiation process in Mayof 2004. It would be regrettable if that fundamental step in an improved process was simply skipped in favour of aunilateral approach driven by budget targets. It must again be mentioned that, to be successful, those stakeholder/PSDnegotiations must address price and, as importantly, what each of the stakeholders can do to work effectively withGovernment to implement more sustainable disease management initiatives.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 15 APRIL, 2008
Generic Drugs – Call for aFundamental ShiftThe complexity of existing practices inrespect of product cost, rebates, allowances andreimbursement strategies associated withgeneric drugs proved to be an area thatoccupied a significant amount of the time andattention of the Task Force. There is littledoubt that this is an area where significantsavings for PharmaCare can be achieved. Therewill, however, be a clear need for a cautious,thoughtful and stakeholder engaged approach toreduce the likelihood of unintended adverseimpact on care delivery on the patientpharmacistrelationship, on the preservation ofan effective and efficient supply chain, and withrespect to value-added contributions ofmanufacturers. This will be addressed ingreater detail below.It is first important to state clearly thatgeneric drug products play an essential role inthe provision of an effective and sustainablehealthcare “eco-system”. All stakeholders,including the innovative drug manufacturers,supported this view. All parties also recognizedthat generic drug products represent a keycomponent in effectively managing drugformularies and costs.Generic drugs have attracted an increasinglysignificant level of the “market share” ofpharmaceutical products. In British Columbiageneric drugs represented approximately 26% ofall PharmaCare expenditures in 2006. Thenumber is expected to increase to approximately52% by 2012 resulting, in large measure, fromthe number of innovative drugs that will “comeoff patent” during that period of time.Despite the important role played by genericdrugs, there are several areas of concern thatwarrant attention if the Province is to besuccessful in generating savings, efficientlyredirecting resources and in making certain thatappropriate accountabilities have been put inplace regarding the provision of services topatients. These concerns include the following:the price paid for generic drugs in Canada issignificantly higher than in other countries.A report by the Patented Medicines PriceReview Board (PMPRB) in June, 2006concluded that Canadian prices for genericdrugs were substantially higher than in 10 of2611 comparator jurisdictions;26PMPRB, June 2006, “Canadian and Foreign Price Trends”. Other studies finding Canadian generic drugs prices to behigh in comparison to other countries include: i) Palmer D'Angelo Consulting Inc, August 2002, “Generic Drug Prices: ACanada US comparison” PDCI <strong>Report</strong> Series, available at:www.pdci.on.ca/pdf/Generic%20Pricing%20Study%20Final%20<strong>Report</strong>.pdf; ii) PMPRB, November 2002, “A Study OfThe Prices Of The Top Selling Multiple Source Medicines In Canada”, available at: www.pmprbcepmb.gc.ca/CMFiles/study-e22SHF-8292005-2710.pdf;iii) Brett Skinner, August 2004, “Generic Drugopoly: Why Non-Patented Prescription Drugs Cost More In Canada Than In The United States And Europe”, available at:www.fraserinstitute.ca/admin/books/files/GenericDrugopoly.pdf; iv) Brett Skinner, February 2005, “Canada's Drug PriceParadox: The Unexpected Losses Caused By Government Interference In Pharmaceutical Markets”, available at:www.fraserinstitute.ca/admin/books/chapterfiles/Jun05ffparadox.pdf; and v)PMPRB, October 2006, “Trends in CanadianSales and Market Structure”. Both PMPRB reports are available at: www.pmprb-cepmb.gc.ca/english/view.asp?x=805.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 16 APRIL, 2008
the 2006 PMPRB report also estimated that,if Canadian generic prices were adjusted toreflect compatibility with prices paid incomparator jurisdictions, Canadian pricesshould have been 32.5% lower than what27they actually were;the procurement relationships betweengeneric drug manufactures, retailpharmacies and government (as the partyresponsible for the reimbursement topatients in respect of generic drug costs) iscomplex and has been distorted by industrypractices in relation to rebates andprofessional allowances;reimbursement to pharmacies has generallybeen based upon invoices which reflect themaximum allowable price for genericproducts. Rebates appear to be based uponthe gap between the net cost of the genericproduct to pharmacies and the maximumallowable price eligible for reimbursement.The average level of rebate has been28estimated to be in the range of 40%.It is not tenable to maintain practices whichresult in provincial reimbursement plans, such asPharmaCare, paying an artificially high price forgeneric drug products particularly in light of thefact that the generic “share” of the market willsoon reach 50% of all prescriptions. As a result,action is clearly necessary to address this issue.The nature of that action will require carefulconsideration and a thoughtful implementationplan.In considering how to proceed, Governmentmay wish to consider a range of options from thenegotiation of a new, more rational, set ofarrangements with generic drug manufacturersand with other interested parties through to amore unilateral legislative response that wouldmake clear the outside limits of government'sfunding obligations in respect of reimbursement29for generic pharmaceuticals.Ontario and Quebec have both opted for thelegislative option with initiatives that limitreimbursement on multi-source generic productsto not more than 50 percent of the cost of brandname products in the same class. This actiongenerated immediate and significant savings onthe price of generics, but it also causedconsiderable confusion and uncertainty in otherareas including the provision of pharmacy-basedcognitive and other direct services to patients, aswell as ongoing confusion in respect of theadministration of the legislative requirements. Itwould also appear that the management of thechanges also had a significant and adverse impacton community based pharmacies.27In dollar terms, this would equate to $1.47 billion based upon 2005 expenditures (See: Federal/Provincial/TerritorialMinisterial Task Force, June 2006, “National Pharmaceuticals Strategy Progress <strong>Report</strong>”, available at: www.hcsc.gc.ca/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/2006-nps-snpp/2006-nps-snpp_e.pdf).2829Canadian Generic Drug Sector Study, Competition Bureau of Canada, October, 2007.A thirty percent rebate level on generic drugs in British Columbia (and that number is likely conservative given what isknown about industry practice) generates approximately $230 million which could be secured as “savings” orredeployed, in whole or in part, to provide for patient services at the pharmacy level.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 17 APRIL, 2008
The Task Force also considered theapproach that was adopted in Nova Scotia toaddress, perhaps more effectively than inOntario and Quebec, the need for a morerational approach to the cost of generics and thedevelopment of more transparent andaccountable arrangements with pharmaciesregarding the provision of quality cognitive, andother, services to patients. The Nova Scotiaapproach, which involved a seven monthnegotiation, provides an example of how acollaborative and effective shared-risk modelcan be developed by government and bystakeholders resulting in significant cost-savingsfor the provincial drug program. The TaskForce recommends that British Columbia adopta collaborative approach similar to the processused in Nova Scotia, but we suggest that theprocess include consideration of options thatwould increase the level of engagement byinnovative drug manufacturers in the postpatentenvironment. A more effective systemmay also necessitate the PSD playing a moredirect role in procurement/acquisition of genericdrugs, but this should not be accomplished in amanner that would negatively impact the level ofservices provided to patients by pharmacists. Ifprudently managed, a new negotiatedarrangement in <strong>BC</strong> should result in moresignificant savings than what was accomplishedin Nova Scotia and a more effectivearrangement than that which resulted from thelegislated approaches in Ontario and Quebec.It must also be mentioned that, in makingtheir submission to the Task Force, theCanadian Generic Pharmaceutical Association(CGPA) invited action to lower thereimbursement level for generic drugs and,further, to restrict “trade spend” on rebatesand allowances. The CGPA called forincreased professional/dispensing fees forpharmacists (this will be addressed in greaterdetail below) as a critical element of anysuccessful reform equation and also sought“first-to-market” incentives for generic drugmanufacturers.The Task Force believes that BritishColumbia should vigorously pursue an overallreduction in the cost of generic drug productsand, further, the development of more rationaltransparent and accountable reimbursementarrangement with pharmacies. Two other keypoints are offered in this regard:1. All parties must understand that theGovernment of British Columbia has alegitimate and pressing interest in achievingthe deployment of effective new costcontainmentinitiatives. If agreementcannot be reached within a reasonableperiod of time – and the benefit of theexperience in Ontario, Quebec and NovaScotia suggests a period of six months, orless, would be sufficient – thenGovernment would have little choice otherthan to take unilateral action to addressthese matters through legislative or othermeans; and2. Given that the CSCW Review ofPharmaCare had made exactly this kind ofTHE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 18 APRIL, 2008
ecommendation for a stakeholdernegotiation process in 2004 to “ensure thatpayments…are fair, appropriate andeffective”, it would not be reasonable forGovernment to now act unilaterally withoutany meaningful effort to negotiate moreacceptable arrangements with the impactedstakeholders.The Role of PharmacyAs will be clear from the preceding section,the Task Force is concerned that, whilesignificant changes are required on a number offronts, it will be important to make certain thatthe essential role of pharmacy and pharmacistsis not compromised through this process ofreform. In fact, we believe that withappropriate consultation and effective multistakeholderengagement this important role canbe enhanced.In many respects, the fiscal focal point ofPharmaCare's relationship with thepharmaceutical supply chain and one of themost important links to effective and accessibleservice delivery to patients is pharmacy. If theprovince's goal is to assure optimal drug therapyand improved outcomes for patients, it will beessential for the PSD to fully engage pharmacy(which is widely viewed as one of the mostaccessible parts of the healthcare system), ininformed and transparent processes to developnew and innovative care practices to improveeffective drug utilization and better patientengagement.The Task Force also shares the view that itwill be necessary for the PSD to enter uponnegotiations with the representatives ofpharmacy to develop and implement a newarrangement for the provision of bothdispensing and other patient-centeredprofessional pharmacy services. Both partieshave, or ought to have, a significant interest inmoving towards a new and more transparentarrangement. For the PSD the goal should beto establish new, more competitive,approaches that will help to containunreasonably high generic prices. For thepharmacy community, decreasing reliance onrebates in favour of clearer understandingswith Government on services provided topatients should be viewed as a much moreappropriate outcome.PharmaCare's reimbursement level hasbeen $8.60 per prescription for a considerableperiod of time. The British ColumbiaPharmacists' Association takes the position that30the real cost is $13.60 per prescription whichis driven by pharmacists spending, on average,one third of their time on professional servicesover and above dispensing. There are twopoints that must be made here as well:1. The PSD has reasonably resisted increasesto the current level of $8.60 perprescription in an environment where it30See: The Activity Based Costing Study Final <strong>Report</strong>, January, 2007, a study jointly sponsored by the <strong>BC</strong> Ministry ofHealth, the Canadian Association of Drug Stores and the British Columbia Pharmacy Association.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 19 APRIL, 2008
was understood that the cost of theseservices were offset by generic rebates andother indirect sources of revenue. In effect,the rebates provided by the generic industryto pharmacy have subsidized the provisionof services provided to patients bypharmacy; and2. If the reimbursement arrangement forgeneric drugs is to be substantially altered,either through negotiation or throughlegislation, it will be essential for the PSD tonegotiate a new arrangement with pharmacyto ensure that high quality patient servicesare sustained and, where possible, improvedwhile also ensuring that the compensationfor pharmacy in respect of the provision ofthese services is reasonable and fair.The Task Force is not indicating that the costof prescriptions should be $13.60 pertransaction. Clearly some adjustment ought tobe put in place but the level should bedetermined through negotiations between theparties. These negotiations should also addressthe scope of, and compensation for, professionalcounseling and other services provided bypharmacy in addition to the dispensing fee. TheJanuary 2007 Activity Based Costing Studyprovides a useful foundation for thecommencement of those discussions.More Direct Engagement with InnovativeDrug ManufacturersAs noted earlier, (see p. 5 above), the PSDhas indicated that one element of theirproposed cost containment initiativecontemplates more direct engagement withmanufacturers to secure product agreementswith “better terms.” The Task Force believesthis proposed approach has considerablepotential but that the PSD would be mostsuccessful if their concept of “better terms”extends beyond economic arrangements to theshared interest that the PSD and industry have,or ought to have, in substantially improvinghealth outcomes for patients.The Task Force heard that innovative drugmanufacturers have developed, or have beeninvolved with, a number of diseasemanagement initiatives in other jurisdictions.From their perspective, improved engagementand a clear and stable operating environmentwould help to create the conditions necessaryfor industry to deploy similar programs inBritish Columbia in partnership with otherhealth care providers. In fact, <strong>BC</strong>'s uniquenessas a platform for improved evidenced-basedpopulation health outcomes is considered byindustry to be a very valuable asset. The TaskForce believes that the province and industryhave much to gain by working more closelytogether to make full and effective use of theresources available to them.If the right conditions for effectiveengagement are to be established, it willremain essential for industry to understand thatthe Province's interest in the containment ofpharmaceutical costs is pressing and substantial.All parties, including the manufacturers ofinnovative drug products, must be prepared toaccept new approaches to shared risk. TheTHE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 20 APRIL, 2008
Task Force was satisfied that there is sufficientrecognition of, and interest in, the shared riskmodel by these stakeholders to warrant furtherserious exploration by the PSD of these options.Increased Utilization of TenderingProcessesThis was likely the most contentious issueconsidered by the Task Force and it wascertainly the area that has caused the greatestlevel of anxiety amongst patient groups andwithin the broader stakeholder community.The Canadian Diabetes Association (CDA)expressed particular concern about amemorandum of understanding signed byAlberta and British Columbia which indicatesthat the two jurisdictions would work togetherto explore the bulk purchase of glucose teststrips with a view towards achieving significantcost savings to the public drug plans in bothjurisdictions. The problem, from the CDAperspective, is that this was being done withlittle or no consultation with the key targetpatient groups and there was considerableconcern that this move would:unreasonably limit patient choice;potentially result in the required use of teststrips that correspond to inferior bloodglucose monitors;lead to a possible decline in diabeteseducation currently available at thepharmacy level;cause further disruption and inconveniencefor a patient group who already experienceconsiderable disruption in their lives; andresult in increased risk of adverse reactionsor declines in quality of care or patientoutcomes that would inevitably shift coststo other parts of the healthcare system.The <strong>BC</strong> Pharmacy Association (<strong>BC</strong>PhA)also expressed substantial concern about thepotential for the increased use of drugtendering. Briefly summarized, their concernsinclude:the reduction in prescribers' optionsinevitably limits options for effectivelymeeting the needs of individual patients;multi-sourced drugs assist in themaintenance of a secure drug supply andthis could be compromised by increasedreliance upon single-source tenderingmechanisms; andthe <strong>BC</strong>PhA shared the concerns of theCDA that single-source tendering couldlead to the required use of inferiorproducts and less effective patientoutcomes.Many of these same concerns werearticulated by the Canadian GenericPharmaceutical Association. From theirperspective tendering carries the followingrisks:a “winner-take-all” environment whichundermines competition;the removal of generic “investments” insupporting community pharmacies andpatient care initiatives;increased vulnerability of product supplyshortages.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 21 APRIL, 2008
The Task Force believes this is an areawhere the PSD will need to proceed with31caution but we believe there is a legitimateplace for tendering as an option in respect ofmeeting some of the procurement needs of theProvince. If Government ultimately elects toproceed with the increased use of tendering,care should be taken to develop tenderingcriteria that will be attentive to the value ofpatient choice, that will avoid the deploymentof older inferior products and, where possible,tendering requirements should be designed tomaintain participation of multiple suppliersperhaps through having variable shares of themarket opportunity determined by the qualityof their respective bids. It is also veryimportant that the tendering process, togetherwith any associated evaluationRecommendations Regarding Procurement OptionsRecommendation Seven:The PSD should initiate a negotiationprocess with drug manufacturers and withrepresentatives of community pharmacy andpharmacists to establish new price andreimbursement arrangements and increasedcompetition in respect of genericpharmaceutical products. If the parties areunable to conclude an acceptable agreementwithin six months the Government shouldmove unilaterally to address the needs ofthe Province through legislation or throughother means.Recommendation Eight:To increase the level of overall fundingtransparency, negotiations with pharmacistsand community pharmacy should providefor a new framework for compensation inrespect of dispensing and other professionalservices provided by pharmacists. Theframework should address thoseprofessional services that can be effectivelyand efficiently provided by pharmacists andshould be linked to transparentaccountability agreements to maintain and,ideally, improve point-of-care services topatients.Recommendation Nine:The PSD should adopt a cautious approachto broadened utilization of tenderingprocesses. The process adopted shouldmirror tendering processes used in otherareas of Government characterized by aprocess that is transparent, fair, open andincludes understandable evaluation criteria.Increased tendering should provide forreasonable levels of patient choice, avoid thedeployment of older inferior products and,where possible, arrangements that providefor participation of multiple suppliers.31The Task Force heard that sole source tendering of glucose strips has been used in New Zealand but there has beensubstantial criticism of the outcomes both with respect to the quality of patient care and in relation to the deployment ofinferior technologies.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 22 APRIL, 2008
criteria/processes, be transparent, clearlycommunicated to all potentially interested partiesand fair. Task Force members further noted thatthe tendering process, a cost controllingprocurement methodology, should not be utilizedas an indirect method to effect clinical outcomes,(for example, tendering to indirectly implementtherapeutic substitution).Issue Three: Strengthening patient careand choice and building positive relationsbetween government decision makers andindustry to achieve those objectives.This aspect of the Task Force mandate hasbeen substantially addressed earlier in this report.Meaningful engagement, transparency inevidence-based decision-making processes and agenuine commitment to a much higher degree ofpartnership-based shared risk arrangements areviewed as the critical elements of a moreconstructive, cost-effective and higher qualitypharmaceutical management system.In many respects, the Task Force processitself has been a useful exercise in thedevelopment of improved relationships and itwould be in the public interest if the PSD andthe various stakeholders continued to buildupon that foundation after the work of the TaskForce is complete. The existing level ofengagement and cooperation between theparties is not sufficient and must be improved.At present stakeholder relations aremanaged almost exclusively by representativesof the PSD. While the Task Force sees this asuseful, and believes it will be important for aneven greater degree of engagement in thefuture, it would also be beneficial if patientgroups and the other key stakeholders had anannual opportunity for an accountability sessionwith the Deputy Minister of Health to discussprogress on improved patient outcomes and thelevel of constructive engagement between theparties.Recommendation Ten:The Deputy Minister of the Ministry of Healthshould commit to participate in an annualaccountability session to hear from patientgroups, from industry and from other keystakeholders regarding improved relationsand the strengthening of the commonobjectives of patient care and choice.Issue Four: The effectiveness of theCommon Drug Review and proposals forimprovement.The Task Force had the benefit of a veryuseful briefing and dialogue with Michael Teirneyof the Common Drug Review who wasforthright and helpful in addressing the status ofthe work conducted by the CDR.We were impressed by the responsivenessof the CDR to recently completed reviews ofthe agency that offered a number ofrecommendations regarding CDR practices andprocedures. It was evident, for example, thatthe CDR had taken steps to improve publicTHE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 23 APRIL, 2008
participation in decision making, toincrease transparency, to facilitate“feedback loops” with industry and toaccelerate the pace of listingrecommendations. In many respects theCDR approach includes severalengagement attributes that could be usedto inform the positive evolution of therelationship between the PSD and keystakeholders.This does not mean that the TaskForce experienced universal support forthe CDR. Industry expressed concernsthat the CDR is disproportionatelyfocused on the cost of new therapies ratherthan on the potential for improved healthoutcomes and that this has resulted in a situationwhere approximately one-half (see Chart Two)of new therapies approved by Health Canadareceive a “recommendation to list” decisionfrom the CDR. According to industry, thisreflects a much lower level of marketengagement opportunity for new therapies inCanada when compared to approval and listingdecisions in other international jurisdictions.Similar concerns were expressed by theCanadian Diabetes Association who criticize theCDR's performance in making new drugtherapies available to Canadians.The Task Force notes that the CDR process,including recommendations to list, or not list,from the CDR's Canadian Expert DrugAdvisory Committee (CEDAC) takes 20-26weeks and that this includes a three weekperiod for manufacturers' comments on CDRreview reports. This commitment toopenness, transparency, engagement and tomuch more efficient decision-making shouldinform similar improvements to the <strong>BC</strong>32process.The Common Drug Review also could, andshould, play a significant role in developing andmaintaining a national data set on keyperformance indicators that would help tofacilitate cross-jurisdictional analysis on matterssuch as time-to-listing, (see: RecommendationTwo, p. 14).Chart TwoCDR Activity to December 31, 2008Number of submissions 115Number of final recommendationsissuedNumber of recommendations to“list”Number of recommendations to“not list”91454632See: <strong>Report</strong> of the Federal Standing Committee on Health, “Prescription Drugs Part 1 – The Common Drug Review:An F/P/T Process”, December 12, 2007.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 24 APRIL, 2008
Recommendation Eleven:Given that <strong>BC</strong> was a lead jurisdiction incalling for the implementation of theCDR, action should be taken to:1. ensure <strong>BC</strong>'s decision-makingprocesses include similar timelinesto those used by the CDR and agreater level of commitment toopenness and transparency; and2. that any unnecessary overlapbetween the CDR and <strong>BC</strong>formulary management systemare reduced to the fullest extentpossible.Issue Five: The effectiveness,transparency and future role of theTherapeutics Initiative in supporting thelisting process of drugs, or a more viable andcost-effective alternative.As will be evident from the section of thisreport dedicated to the identification ofproposed improvements to British Columbia'slisting process, the Task Force recommends thereplacement of the Therapeutics Initiative with anew process that would provide for a muchwider array of expertise to consider thetherapeutic value and cost-effectiveness of newdrug therapies (see: Recommendation Four,p.12). This approach, we believe, is viewed asbeing preferable to the option of endeavoring toinitiate a reform of the Therapeutics Initiative.The Therapeutics Initiative is regarded by mostwho participated in this process, other than thePSD leadership, as narrow, insular and resistantto meaningful stakeholder engagement.If, in the alternative, the Ministry of Healthelects to maintain the existing arrangement(s)substantial reforms will be required to addressthe need for mechanisms more appropriate tomodern concepts of governance andaccountability, the expansion of the scope ofexpertise available to the Therapeutics Initiativeand the elimination of direct engagement byTherapeutics Initiative members in the work ofthe Drug Benefit Committee.Furthermore, if the Therapeutics Initiativeis to continue it will be necessary to take stepsto provide it with a level of financial resourceappropriate to their continuing functions. TheTask Force would also recommend that theirpublic education role should be reassigned to33the new Drug Utilization Branch of the PSD.33Recent steps initiated by the Ministry of Health, (see “Province Promotes Best Practices for Drug Prescribing”, March25, 2008), are a positive step in this regard.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 25 APRIL, 2008
Recommendation Twelve:Subject to Recommendation Four, if theTherapeutics Initiative is maintained,action must be taken in the followingareas:the governance, membership andaccountability standards associatedwith the operation of theTherapeutics Initiative will requiresubstantial improvement;· steps must also be taken to renewand revitalize the panel of expertsthe Therapeutics Initiative reliesupon to discharge its obligations;the function of the TherapeuticsInitiative should be focused ontherapeutic evaluation. Activitiesbeyond that core mandate such aspublic education should bereassigned to the PSD's DrugUtilization Unit where anaccountable process can beimplemented to assure the unbiasedand evidence-based practices;the practice of having members ofthe Therapeutics Initiative alsoparticipating in the work of theDrug Benefits Committee should beterminated.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 26 APRIL, 2008
Summary of RecommendationsAn Improved Drug Review/ListingProcessRecommendation One: Priority attentionshould be focused on development of anenhanced Formulary Management Systemtogether with improved stakeholderengagement and appeal mechanisms. This workshould be led by the Pharmaceutical ServicesDivision and include meaningful engagementwith stakeholders, including patients, healthcareprofessionals, disease specialists, researchleaders and industry.Recommendation Two: The Ministry ofHealth should act to establish new targetreview/listing decision guidelines with the goal ofsubstantially improving British Columbia'sperformance on time-to-listing decisions.Progress on this front must be publicly reportedand consistently benchmarked against theperformance of other jurisdictions.Recommendation Three: The DrugBenefit Committee should be reconstituted asthe “Drug Benefit Council” to moreappropriately reflect the arms length role it isexpected to carry out in the review processesapplicable to consideration of new therapies.Recommendation Four: The Ministry ofHealth should establish a new Drug ReviewResource Committee to carry out the drugsubmission review role currently performed bythe Therapeutics Initiative. This new DRRCshould also provide for a registry of experts thatwill substantially widen the array of expertiseavailable to offer advice and recommendationson the therapeutic value and cost-effectivenessof new drug therapies.Recommendation Five: The membershipof the D<strong>BC</strong> should be modified to include theparticipation of at least three public membersselected through a process external to thePSD. Government may also wish to considerensuring that at least one member of the D<strong>BC</strong>has broad economic expertise to supplementthe existing expertise that is focused morenarrowly on health economics.Recommendation Six: No members ofthe Therapeutics Initiative or, in the alternative,no participant in a Drug Coverage ReviewTeam should participate as members in thework of the Drug Benefit Council.Improved Procurement PracticesRecommendation Seven: The PSDshould initiate a negotiation process with drugmanufacturers and with representatives ofcommunity pharmacy and pharmacists toestablish new price and reimbursementarrangements and increased competition inrespect of generic pharmaceutical products. Ifthe parties are unable to conclude anacceptable agreement within six months theGovernment should move unilaterally toaddress the needs of the Province throughlegislation or through other means.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 27 APRIL, 2008
Recommendation Eight: To increase thelevel of overall funding transparency,negotiations with pharmacists and communitypharmacy should provide for a new frameworkfor compensation in respect of dispensing andother professional services provided bypharmacists. The framework should addressthose professional services that can beeffectively and efficiently provided bypharmacists and should be linked to transparentaccountability agreements to maintain and,ideally, improve point-of-care services topatients.Recommendation Nine: The PSD shouldadopt a cautious approach to broadenedutilization of tendering processes. The processadopted should mirror tendering processes usedin other areas of Government characterized bya process that is transparent, fair, open andincludes understandable evaluation criteria.Increased tendering should provide forreasonable levels of patient choice, avoid thedeployment of older inferior products and,where possible, arrangements that provide forparticipation of multiple suppliers.BuildingPositive and ProductiveRelationshipsRecommendation Ten: The DeputyMinister of the Ministry of Health shouldcommit to participate in an annual accountabilitysession to hear from patient groups, fromindustry and from other key stakeholdersregarding improved relations and thestrengthening of the common objectives ofpatient care and choice.Improving the Common DrugReview ProcessRecommendation Eleven: Given that <strong>BC</strong>was a lead jurisdiction in calling for theimplementation of the CDR, action should betaken to:1.ensure <strong>BC</strong>'s decision-making processesinclude similar timelines to those used bythe CDR and a greater level ofcommitment to openness andtransparency; and2.that any unnecessary overlap between theCDR and <strong>BC</strong> formulary managementsystem are reduced to the fullest extentpossible.Replacing or Reconstituting theTherapeutics InitiativeRecommendation Twelve: Subject toRecommendation Four, if the TherapeuticsInitiative is maintained, action must be taken inthe following areas:the governance, membership andaccountability standards associated withthe operation of the Therapeutics Initiativewill require substantial improvement;steps must also be taken to renew andrevitalize the panel of experts theTherapeutics Initiative relies upon todischarge its obligations;THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 28 APRIL, 2008
the function of the Therapeutics Initiativeshould be focused on therapeuticevaluation. Activities beyond that coremandate such as public education should bereassigned to the PSD's Drug UtilizationUnit where an accountable process can beimplemented to assure the unbiased andevidence-based practices;the practice of having members of theTherapeutics Initiative also participating inthe work of the Drug Benefits Committeeshould be terminated.THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 29 APRIL, 2008
THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 30 APRIL, 2008
THE REPORT OF PHARMACEUTICAL POLICY RECOMMENDATIONS FOR THE MINISTRY OF HEALTH 31 APRIL, 2008