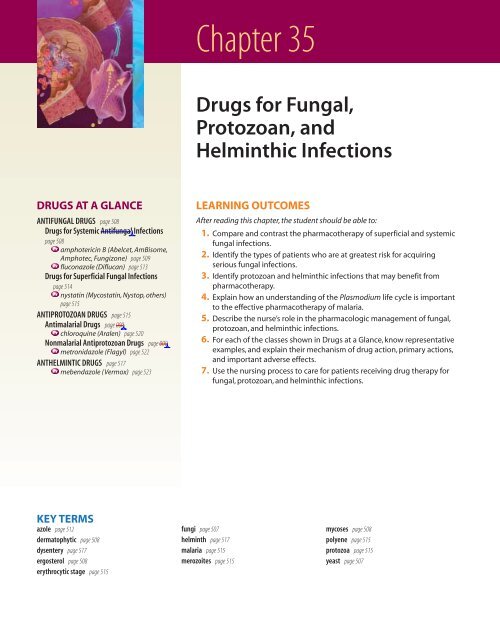
Drugs for Fungal, Protozoan, and Helminthic Infections
Drugs for Fungal, Protozoan, and Helminthic Infections
Drugs for Fungal, Protozoan, and Helminthic Infections
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 508508 Unit 5 The Immune SystemMyNursingKit Doctor Fungus35.2 Classification of Mycoses<strong>Fungal</strong> infections are called mycoses. A simple <strong>and</strong> usefulmethod of classifying mycoses is to consider them as eithersuperficial or systemic.Superficial mycoses affect the scalp, skin, nails, <strong>and</strong> mucousmembranes such as the oral cavity <strong>and</strong> vagina. In mostcases, the fungus invades only the surface layers of these regions.Mycoses of this type are often treated with topicaldrugs because the incidence of adverse effects is much lowerusing this route of administration. Superficial fungal infectionsare sometimes called dermatophytic.Systemic mycoses are those affecting internal organs,typically the lungs, brain, <strong>and</strong> digestive organs. Althoughmuch less common than superficial mycoses, systemicfungal infections affect multiple body systems <strong>and</strong> aresometimes fatal to patients with suppressed immune systems.Mycoses of this type require aggressive oral or parenteralmedications that produce more adverse effectsthan the topical agents.Historically, the antifungal drugs used <strong>for</strong> superficial infectionswere clearly distinct from those prescribed <strong>for</strong> systemicinfections. In recent years, this distinction hasblurred, as some of the newer antifungal agents may be used<strong>for</strong> either superficial or systemic infections. Furthermore,some superficial infections may be treated with oral, ratherthan topical, agents. For example, nail infections are superficial,but are often treated with oral antifungal drugs. Thistherapeutic division between superficial <strong>and</strong> systemic mycosesis still useful, however, since it separates the pharmacotherapyof relatively benign infections (superficial) fromthose that may be life threatening (systemic).35.3 Mechanism of Actionof Antifungal <strong>Drugs</strong>Biologically, fungi are classified as eukaryotes; their cellularstructure <strong>and</strong> metabolic pathways are more similar to thoseof humans than to bacteria. Anti-infectives that are efficaciousagainst bacteria are ineffective in treating mycoses becauseof these differences in physiology. Thus, an entirelydifferent set of agents is needed to eliminate fungal infections.One important difference between fungal cells <strong>and</strong> humancells is the steroid used in constructing plasma membranes.Whereas cholesterol is essential <strong>for</strong> animal cellmembranes, ergosterol is present in fungi. The largest class ofantifungal drugs, the azoles, inhibits ergosterol biosynthesis,causing the fungal plasma membrane to become porous orleaky. Amphotericin B (Fungizone), terbinafine (Lamisil),<strong>and</strong> nystatin (Mycostatin) also act by this mechanism.Some antifungals take advantage of enzymatic differencesbetween fungi <strong>and</strong> humans. For example, in fungi, flucytosine(Ancobon) is converted to the toxic antimetabolite 5-fluorouracil, which inhibits both DNA <strong>and</strong> RNA synthesisin the pathogen. Humans do not have the enzyme necessary<strong>for</strong> this conversion. Indeed, 5-fluorouracil itself is a commonantineoplastic drug (see chapter 37 ).DRUGS FOR SYSTEMIC ANTIFUNGALINFECTIONSSystemic or invasive fungal disease may require intensivepharmacotherapy <strong>for</strong> extended periods. Amphotericin BTABLE 35. 2<strong>Drugs</strong> <strong>for</strong> Systemic Mycoses*Drug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsamphotericin B (Abelcet,AmBisome, Amphotec, Fungizone)IV (conventional <strong>for</strong>m); 0.3–1.5 mg/kg/day, infused over2–4 h (max 1.5 mg/kg/day)Hypokalemia, hypomagnesemia, rash, fever <strong>and</strong> chills,nausea <strong>and</strong> vomiting, anorexia, headacheNephrotoxicity, liver failure, anaphylaxis, cardiac arrest,thrombocytopenia, leukopenia, agranulocytosis, <strong>and</strong>anemiaanidulafungin (Eraxis) IV; loading dose 100 mg on day 1 followed by 50 mg/day Minor allergic reactions such as rash, urticaria, flushingAnaphylaxiscaspofungin acetate (Cancidas)IV; 70 mg infused over 1 h on day 1, followed by 50 mginfused over 1 h qid <strong>for</strong> 30 daysFever, headache, infusion-related phlebitis <strong>and</strong>thrombophlebitisAnaphylaxisflucytosine (Ancobon) PO; 50–150 mg/kg in divided doses Nausea, vomiting, headacheBlood dyscrasias, cardiac toxicity, renal failure,psychosismicafungin (Mycamine)IV; 150 mg/kg/day over 1 h <strong>for</strong> active C<strong>and</strong>ida infection;50 mg/kg/day IV over 1 h <strong>for</strong> C<strong>and</strong>ida prophylaxis*Azole antifungal drugs <strong>for</strong> systemic infections are included in Table 35.3.Italics indicate common adverse effects; underlining indicates serious adverse effects.Headache, nausea, rash, phlebitisLeukopenia, serious allergic reactions, delirium# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 508Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 509Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 509(Abelcet, AmBisome, Amphotec, Fungizone) <strong>and</strong> fluconazole(Diflucan) are drugs of choice. Selected systemic antifungaldrugs are listed in Table 35.2.35.4 Pharmacotherapy ofSystemic <strong>Fungal</strong> DiseasesBecause human immune defenses provide a <strong>for</strong>midable barrierto fungi, serious fungal infections are rarely encounteredin persons with healthy body defenses. The AIDSepidemic, however, has resulted in the frequent clinical occurrenceof previously rare mycoses, such as cryptococcosis<strong>and</strong> coccidioidomycosis. Opportunistic fungal disease inAIDS patients spurred the development of several newdrugs <strong>for</strong> systemic fungal infections over the past 20 years.Others who may experience systemic mycoses include thosepatients receiving prolonged therapy with corticosteroids,experiencing extensive burns, receiving antineoplasticagents, having indwelling vascular catheters, or having recentlyreceived organ transplants. Systemic antifungal drugshave little or no antibacterial activity, <strong>and</strong> pharmacotherapyis sometimes continued <strong>for</strong> several months.There are relatively few drugs available <strong>for</strong> treating systemicmycoses. Amphotericin B has been the preferred drug<strong>for</strong> systemic fungal infections since the 1960s; however, thismedication can cause a number of serious side effects. Thenewer azole drugs such as itraconazole are considerably safer<strong>and</strong> have become drugs of choice <strong>for</strong> less severe infections.Prototype Drug ❘ Amphotericin B (Fungizone, others)Therapeutic Class: Antifungal (systemic type)Pharmacologic Class: PolyeneACTIONS AND USESADVERSE EFFECTSAmphotericin B has a broad spectrum of activity <strong>and</strong> is effective against most ofthe fungi pathogenic to humans; thus, it is a preferred drug <strong>for</strong> most many systemicmycoses. It may also be indicated as prophylactic antifungal therapy <strong>for</strong>patients with severe immunosuppression.It acts by binding to ergosterol in fungalcell membranes, causing them to become permeable or leaky. Because amphotericinB is not absorbed from the GI tract, it is normally given by IV infusion.Topical preparations are available <strong>for</strong> superficial mycoses. Several months ofpharmacotherapy may be required <strong>for</strong> a complete cure. Resistance to amphotericinB is not common.To reduce the toxicity of amphotericin B,the original drug molecule has been<strong>for</strong>mulated with several lipid molecules:■ Liposomal amphotericin B (AmBisome): consists of closed spherical vesicles.Amphotericin B in integrated into the lipid membrane■ Amphotericin B lipid complex (Abelcet): contains amphotericin B complexedwith two phospholipids in a 1:1 ratio■ Amphotericin B cholesteryl sulfate complex (Amphotec): consists of a colloidalsuspension of amphotericin B in a 1:1 ratio with the lipid cholesterylsulfate in microscopic disk-shaped particlesThe principal advantage of the lipid <strong>for</strong>mulations is reduced nephrotoxicity<strong>and</strong> less infusion-related fever <strong>and</strong> chills. The reduced toxicity is believed to bedue to the decreased plasma levels of the drug.ADMINISTRATION ALERTS■ Infuse slowly, because cardiovascular collapse may result if the medicationis infused too rapidly.■ Administer premedication to help decrease the risk of infusion reactions.■ Withhold the drug if the BUN exceeds 40 mg/dL or serum creatinine risesabove 3 mg/dL.■ Pregnancy category BAmphotericin B can produce frequent <strong>and</strong> sometimes serious adverse effects.Many patients develop fever <strong>and</strong> chills, vomiting, <strong>and</strong> headache at the beginningof therapy,which subside as treatment continues.Phlebitis is common duringIV therapy.Some degree of nephrotoxicity is observed in 80% of the patientstaking this drug <strong>and</strong> electrolyte imbalances such as hypokalemia frequently occur.Cardiacarrest,hypotension,<strong>and</strong> dysrhythmias are possible.Because amphotericinB can cause ototoxicity, the nurse should assess <strong>for</strong> hearing loss, vertigo,unsteady gait, or tinnitus.Contraindications: The only contraindication is hypersensitivity to the drug.Caution must be observed when using amphotericin B in patients with renal impairment.INTERACTIONSDrug–Drug: Amphotericin B interacts with many drugs. Concurrent therapy withdrugs that reduce renal function, such as aminoglycosides, vancomycin, or carboplatinis not recommended. Use with corticosteroids, skeletal muscle relaxants, <strong>and</strong> thiazolemay potentiate hypokalemia. Use with digoxin increases the risk of digoxin toxicity inpatients with pre-existing hypokalemia.Lab Tests: Amphotericin B may increase values of the following: serum creatinine,alkaline phosphatase, BUN, aspartate aminotransferase (AST), <strong>and</strong> alanineaminotransferase (ALT); may decrease values <strong>for</strong> serum potassium, calcium, <strong>and</strong>magnesium.Herbal/Food: Unknown.Treatment <strong>for</strong> Overdose: Overdose may result in cardiorespiratory arrest. Nospecific therapy is available; patients are treated symptomatically.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.PHARMACOKINETICS (IV)Onset: 1–2 hPeak: 1–2 hHalf-life: 24–48 hDuration: 20 h# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 509Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 510510 Unit 5 The Immune SystemNURSING PROCESS FOCUSPATIENTS RECEIVING ANTIFUNGAL DRUGSAssessmentPotential Nursing DiagnosesBaseline assessment prior to administration:■ Underst<strong>and</strong> the reason the drug has been prescribed in order to assess <strong>for</strong>therapeutic effects.■ Obtain a complete health history including neurologic, cardiovascular,respiratory, hepatic or renal disease, <strong>and</strong> the possibility of pregnancy. Obtain adrug history including allergies, including specific reactions to drugs, currentprescription <strong>and</strong> OTC drugs, herbal preparations, <strong>and</strong> alcohol use. Be alert topossible drug interactions.■ Assess signs <strong>and</strong> symptoms of current infection noting location,characteristics, presence or absence of drainage <strong>and</strong> character of drainage,duration, <strong>and</strong> presence or absence of fever or pain.■ Evaluate appropriate laboratory findings (e.g., CBC, electrolytes, urinalysis,culture <strong>and</strong> sensitivity (C&S), hepatic <strong>and</strong> renal function studies).■ Obtain baseline weight <strong>and</strong> vital signs, especially blood pressure <strong>and</strong> pulse.Assessment throughout administration:■ Assess <strong>for</strong> desired therapeutic effects (e.g., diminished signs <strong>and</strong> symptoms ofinfection <strong>and</strong> fever).■ Continue periodic monitoring of CBC, electrolytes, hepatic <strong>and</strong> renal function,<strong>and</strong> C&S.■ Continue to monitor vital signs, especially blood pressure <strong>and</strong> pulse, inpatients on IV antifungals.■ Assess <strong>for</strong> adverse effects: nausea, vomiting, abdominal cramping, diarrhea,malaise, muscle cramping or pain, chills, drowsiness, dizziness, headache,tinnitus, vertigo, flushing, skin rash, urticaria, seizures, hypotension, <strong>and</strong>electrolyte imbalances (e.g., hypokalemia, hypomagnesemia). Hypotension,tachycardia, dysrhythmias, changes in level of consciousness (LOC),diminished urine output, or seizures should be reported immediately.Planning: Patient Goals <strong>and</strong> Expected Outcomes■■■■■■■■Infection (current or risk <strong>for</strong> concurrent bacterial infection)Pain (related to infection)HyperthermiaDeficient Knowledge (drug therapy)Risk <strong>for</strong> Injury (related to adverse drug effects)Risk <strong>for</strong> Deficient Fluid Volume (related to fever, diarrhea caused by adversedrug effects)Risk <strong>for</strong> Decreased Cardiac Output, Ineffective Tissue Perfusion (related toadverse effects of IV antifungals)Risk <strong>for</strong> Noncompliance (related to adverse drug effects, deficient knowledge,or length of therapy)The patient will:■ Experience therapeutic effects (e.g., diminished signs <strong>and</strong> symptoms of infection, decreased fever).■ Be free from, or experience minimal, adverse effects.■ Verbalize an underst<strong>and</strong>ing of the drug’s use, adverse effects, <strong>and</strong> required precautions.■ Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider).ImplementationInterventions <strong>and</strong> (Rationales)Patient <strong>and</strong> Family EducationEnsuring therapeutic effects:■ Continue assessments as described earlier <strong>for</strong> therapeutic effects. (Diminishedfever, pain, or signs <strong>and</strong> symptoms of infection should be noted.)Minimizing adverse effects:■ Continue frequent monitoring of vital signs, especially blood pressure <strong>and</strong>pulse, <strong>and</strong> respiratory rate <strong>and</strong> depth in patients on IV antifungals.Immediately report dysrhythmias, increasing pulmonary congestion,hypotension, or tachycardia. (Cardiovascular abnormalities are possibleadverse effects of IV antifungals. Cardiac <strong>and</strong> respiratory assessment must bemonitored closely to observe <strong>for</strong> adverse effects.)■■Teach the patient on oral antifungals that several months of treatment may berequired.Teach the patient on topical antifungals to complete the entire courseof therapy <strong>and</strong> notify the health care provider if symptoms have not resolved.Instruct the patient on the need <strong>for</strong> frequent monitoring. Explain therationale <strong>for</strong> all monitoring equipment used.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 510Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 511NURSING PROCESS FOCUSInterventions <strong>and</strong> (Rationales)■Continue to monitor periodic lab work: hepatic <strong>and</strong> renal function tests, CBC,urinalysis, culture <strong>and</strong> sensitivity, <strong>and</strong> electrolyte levels. (Antifungals arehepatic <strong>and</strong> renal toxic <strong>and</strong> labs should be monitored frequently. Periodic C&Stests may be ordered if infections are severe or are slow to resolve to confirmappropriate therapy is being delivered. Antifungals, particularly when givenIV, may cause electrolyte imbalances, especially hypokalemia <strong>and</strong>hypomagnesemia, <strong>and</strong> electrolyte replacement may be needed.)■ Weigh the patient daily <strong>and</strong> report a weight gain of 1 kg or more in a 24-hour period. Measure intake <strong>and</strong> output in the hospitalized patient. (Dailyweight is an accurate measure of fluid status <strong>and</strong> takes into account intake,output, <strong>and</strong> insensible losses. Excessive weight gain or edema may indicaterenal dysfunction.)■■■■■■■■Monitor <strong>for</strong> hypersensitivity <strong>and</strong> allergic reactions, especially with the firstdose of IV antifungal. Continue to monitor the patient throughout therapy.(Anaphylactic reactions are possible <strong>and</strong> are most common with the first IVinfusion. A test-dose of a small amount given slowly may be given be<strong>for</strong>emain infusion. Premedication, including antipyretics, antihistamines, <strong>and</strong>antiemetics may be necessary to prevent reactions.)Ensure adequate hydration in patients on oral or IV antifungals. (Antifungaldrugs are renal toxic <strong>and</strong> adequate hydration helps to prevent adverse renaleffects.)Continue to monitor <strong>for</strong> signs of ototoxicity. (Antifungals may causeototoxicity <strong>and</strong> require frequent monitoring to prevent adverse effects.)Continue to monitor <strong>for</strong> hepatic toxicity; e.g., jaundice, RUQ pain, darkenedurine, diminished urine output, tinnitus, vertigo, in patients on IV or oralantifungal therapy. (Antifungals may cause hepatic toxicity <strong>and</strong> requirefrequent monitoring to prevent adverse effects.)Monitor the IV site frequently <strong>for</strong> any signs of extravasation orthrombophlebitis. (IV antifungal medication is irritating to veins. Use acentral line if possible or frequently monitor the IV site. Infusion pumpsmust be used to ensure the proper dosage rate <strong>and</strong> prevent excessive flowrate.)Monitor blood glucose in patients taking ketoconazole. (Ketoconazole mayincrease glucose levels. Diabetic patients may require a change in theirantidiabetic drug routine.)Monitor <strong>for</strong> significant GI effects, including nausea, vomiting, <strong>and</strong> abdominalpain or cramping. Give the drug with food or milk to decrease adverse GIeffects. (Food or milk may decrease GI effects but an antiemetic may also berequired if nausea is severe.)Monitor <strong>for</strong> signs <strong>and</strong> symptoms of secondary infection in topical areas offungal infection, e.g., athlete’s foot. If systemic adverse effects are noted,check the drug dose or administration route the patient is using. (Intenseitching with scratching may introduce bacteria into the area, resulting in asecondary bacterial infection that may require additional antibacterialtherapy.Topical drug amounts are usually insufficiently absorbed to createsystemic effects.)Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 511PATIENTS RECEIVING ANTIFUNGAL DRUGS (Continued)ImplementationPatient <strong>and</strong> Family Education■■■■■■■■■■Teach the patient about the need <strong>for</strong> frequent lab testing. If on oralantifungals at home, instruct the patient on the need <strong>for</strong> periodic lab work.Have the patient taking oral antifungal drugs at home weigh self daily,ideally at the same time of day, <strong>and</strong> record weight along with bloodpressure <strong>and</strong> pulse measurements. Have the patient report significantweight gain.Instruct the patient to promptly report any chills, nausea, tremors, orheadache.Teach the patient to increase fluid intake to 2 L per day if on oralantifungals. Explain the rationale <strong>for</strong> increased IV fluid hydration inpatients on IV antifungals.Teach the patient to immediately report any ringing, humming, orbuzzing in ears, <strong>and</strong> dizziness or vertigo.Teach the patient to immediately report any nausea, vomiting, yellowingof skin or sclera, abdominal pain, light or clay-colored stools, or darkeningof urine.Instruct the patient to immediately report any pain, burning, or rednessat the site of the peripheral IV. Explain the rationale <strong>for</strong> all equipmentused.Teach the diabetic patient to test glucose more frequently, reporting anyconsistent elevations to the health care provider.Teach the patient to take the drug with food or milk but to avoid acidicfoods <strong>and</strong> beverages or carbonated drinks.Teach the patient to report any increasing redness, soreness or pain, orincreasing drainage from affected site.(Continued)# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 511Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 512512 Unit 5 The Immune SystemNURSING PROCESS FOCUSInterventions <strong>and</strong> (Rationales)Patient underst<strong>and</strong>ing of drug therapy:■ Use opportunities during administration of medications <strong>and</strong> duringassessments to discuss the rationale <strong>for</strong> drug therapy, desired therapeuticoutcomes, most common adverse effects, parameters <strong>for</strong> when to call thehealth care provider, <strong>and</strong> any necessary monitoring or precautions.(Using timeduring nursing care helps to optimize <strong>and</strong> rein<strong>for</strong>ce key teaching areas.)Patient self-administration of drug therapy:■ When administering medications, instruct the patient <strong>and</strong>/orfamily/caregiver in proper self-administration techniques. (Properadministration will increase the effectiveness of the drug.)PATIENTS RECEIVING ANTIFUNGAL DRUGS (Continued)ImplementationEvaluation of Outcome CriteriaPatient <strong>and</strong> Family Education■■The patient <strong>and</strong>/or family/caregiver should be able to state the reason <strong>for</strong>the drug; appropriate dose <strong>and</strong> scheduling; what adverse effects toobserve <strong>for</strong> <strong>and</strong> when to report; <strong>and</strong> the anticipated length of medicationtherapy.Teach the patient to take oral or topical antifungal medication as follows:■ Complete the entire course of therapy unless otherwise instructed.Several months of oral therapy may be required to adequately treat theinfection.■ Avoid or eliminate alcohol while on oral antifungals to avoid hepaticcomplications.■ Dissolve oral antifungal lozenges (troches) in mouth or rinse with liquidsafter meals <strong>and</strong> at bedtime. If dentures are worn, remove them be<strong>for</strong>eusing the drug <strong>and</strong> leave out overnight. Swish the liquid drug aroundmouth <strong>and</strong> hold in the mouth at least 2 minutes be<strong>for</strong>e expectorating.Do not swallow unless instructed to do so <strong>and</strong> do not rinse the mouthwith water afterwards.■ Do not use occlusive dressings when topical antifungals are used. Applya thin, even layer to the affected area.■ Allow affected skin areas to air dry <strong>and</strong> wear loose-fitting <strong>and</strong>“breathable” fabric clothes to allow adequate ventilation. Gently cleanseareas with mild soap <strong>and</strong> water <strong>and</strong> avoid vigorous scrubbing.Evaluate the effectiveness of drug therapy by confirming that patient goals <strong>and</strong> expected outcomes have been met (see “Planning”).See Tables 35.2, 35.3, <strong>and</strong> 35.4 <strong>for</strong> a list of drugs to which these nursing actions apply.Although rarely used as monotherapy, flucytosine (Ancobon)is sometimes combined with amphotericin B in thepharmacotherapy of severe c<strong>and</strong>idiasis. Flucytosine cancause immunosuppression <strong>and</strong> liver toxicity, <strong>and</strong> resistancehas become a major problem.A newer class of antifungals called echinoc<strong>and</strong>ins has beenadded to the treatment options <strong>for</strong> systemic mycoses. Thefirst drug in this class, caspofungin, has become an importantalternative to amphotericin B in the treatment of aspergillosis.Approved in 2006, anidulafungin (Eraxis) isapproved <strong>for</strong> invasive c<strong>and</strong>idiasis. The echinoc<strong>and</strong>ins areless nephrotoxic than amphotericin B <strong>and</strong> have fewer seriousadverse effects.AZOLESThe azole drugs consist of two different chemical classes,the imidazoles <strong>and</strong> the triazoles. Azole antifungal drugs interferewith the biosynthesis of ergosterol, which is essential<strong>for</strong> fungal cell membranes. Depleting fungal cells ofergosterol impairs their growth. The azole drugs are listedin Table 35.3.35.5 Pharmacotherapywith the Azole AntifungalsThe azole class is the largest <strong>and</strong> most versatile group of antifungals.These agents have a broad spectrum <strong>and</strong> are usedto treat nearly any systemic, cutaneous, or superficial fungalinfection. Fluconazole (Diflucan), itraconazole (Sporanox),ketoconazole (Nizoral), <strong>and</strong> voriconazole (Vfend) are used<strong>for</strong> both systemic <strong>and</strong> topical infections. The remainder ofthe azoles are prescribed <strong>for</strong> superficial infections.Ketoconazole is available only orally, <strong>and</strong> is the most hepatotoxicof the azoles. Itraconazole has begun to replace ketoconazolein the therapy of systemic mycoses because it isless hepatotoxic <strong>and</strong> may be given either orally or intravenously.It also has a broader spectrum of activity than theother systemic azoles. Clotrimazole (Mycelex, others) is apreferred drug <strong>for</strong> superficial fungal infections of the skin,vagina, <strong>and</strong> mouth.The systemic azole drugs have a spectrum of activity similarto that of amphotericin B, are considerably less toxic,<strong>and</strong> have the major advantage that they can be administeredorally. Because of these characteristics, azoles have replacedamphotericin B in the pharmacotherapy of less# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 512Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 513Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 513TABLE 35. 3 Azole AntifungalsDrug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsbutoconazole (Femstat) Topical; 1 applicator intravaginally at bedtime <strong>for</strong> 3 days Oral <strong>and</strong> parenteral routes:clotrimazole (FemCare, Gyne-Lotrimin,Mycelex, others)econazole (Spectazole)fluconazole (Diflucan)itraconazole (Sporanox)ketoconazole (Nizoral)miconazole (Micatin, Monistat, Cruex, others)oxiconazole (Oxistat)sertaconazole (Ertaczo)sulconazole nitrate (Exelderm)terconazole (Terazol)tioconazole (Vagistat)voriconazole (Vfend)Topical; apply bid <strong>for</strong> 4 wk; <strong>for</strong> vaginal mycoses, insert 1 applicatorintravaginally at bedtime <strong>for</strong> 7 daysTopical; apply bid <strong>for</strong> 4 wkPO/IV; 200–400 mg on day 1, then 100–200 mg/day <strong>for</strong> 2–4 wkPO; 200 mg/day; may increase to 200 mg bid (max: 400 mg/day)PO; 200–400 mg/dayTopical; apply once or twice daily to affected areaTopical; apply bid <strong>for</strong> 2–4 wkTopical; apply daily in the evening <strong>for</strong> 2 moTopical; 2% cream bid <strong>for</strong> 4 wkTopical; apply once or twice daily <strong>for</strong> 2–6 wkTopical; 1 applicator intravaginally at bedtime <strong>for</strong> 3–7 wkTopical; 1 applicator intravaginally at bedtime <strong>for</strong> 1 dayIV; 6 mg/kg every 12 h on day 1, then 4 mg/kg every 12 h; mayreduce to 3 mg/kg every 12 h if not toleratedItalics indicate common adverse effects; underlining indicates serious adverse effects.Fever, chills, rash, dizziness, drowsiness, nausea,vomiting, diarrheaHepatotoxicity, anaphylaxis, blood dyscrasiasTopical route:Drying of skin, stinging sensation atapplication site, pruritus, urticaria, contactdermatitisNo serious adverse effectsPrototype DrugTherapeutic Class: Antifungal❘ Fluconazole (Diflucan)Pharmacologic Class: Inhibitor of fungal cell membrane synthesis; azoleFluconazole causes few serious adverse effects. Nausea, vomiting, <strong>and</strong> diarrheaare reported at high doses. Unlike ketoconazole, hepatotoxicity is rare with fluconazole,althoughpatients with hepatic impairment should be monitored care-ACTIONS AND USESADVERSE EFFECTSLike other azoles, fluconazole acts by interfering with the synthesis of ergosterol.Fluconazole, however, offers several advantages over other systemic antifungals.It is rapidly <strong>and</strong> completely absorbed when given orally, <strong>and</strong> it isparticularly effective against C<strong>and</strong>ida albicans. Unlike itraconazole (Sporanox) fully.<strong>and</strong> ketoconazole (Nizoral), fluconazole is able to penetrate most body membranesto reach infections in the CNS, bone, eye, urinary tract, <strong>and</strong> respiratorytract.A major disadvantage of fluconazole is its relatively narrow spectrum of activity.Although it is effective against C<strong>and</strong>ida albicans, it may not be effectiveagainst non–albicans C<strong>and</strong>ida species, which account <strong>for</strong> a significant percentageof opportunistic fungal infections.ADMINISTRATION ALERTS■ Do not mix IV fluconazole with other drugs.■ Pregnancy category CPHARMACOKINETICSOnset: UnknownPeak: 2 hHalf-life: 20–50 hDuration: UnknownStevens–Johnson syndrome has been reported in patients withimmunosuppression.Contraindications: Fluconazole is contraindicated in patients with hypersensitivityto the drug. Coadministration with cisapride is contraindicated. Becausemost of the drug is excreted by the kidneys, it should be used cautiously in patientswith pre-existing kidney disease.INTERACTIONSDrug–Drug: Use of fluconazole with warfarin may cause increased risk <strong>for</strong> bleeding.Hypoglycemia may result if fluconazole is administered concurrently with certain oralhypoglycemics, including glyburide. Fluconazole levels may be decreased withconcurrent rifampin or cimetidine use.The effects of fentanyl, alfentanil, ormethadone may be prolonged with concurrent administration of fluconazole.Lab Tests: Values <strong>for</strong> AST, ALT, <strong>and</strong> alkaline phosphatase may be increased.Herbal/Food: UnknownTreatment of Overdose: There is no specific treatment <strong>for</strong> overdose.Dialysis canbe used to lower the serum drug level.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.MyNursingKit Mechanism in Action: Fluconazole# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 513Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 514514 Unit 5 The Immune SystemMyNursingKit World Health Organizationserious systemic fungal infections. Topical <strong>for</strong>mulations areavailable <strong>for</strong> superficial mycoses, although they may also begiven by the oral route <strong>for</strong> these infections.The most common adverse effects of the systemic azolesare nausea <strong>and</strong> vomiting; severe nausea may require dose reductionor the concurrent administration of an antiemetic.Anaphylaxis <strong>and</strong> rash have been reported. Fatal druginducedhepatitis has occurred with ketoconazole, thoughthe incidence is rare <strong>and</strong> has not been reported with theother systemic azoles. Azoles may affect glycemic control indiabetic patients. Various reproductive abnormalities havebeen reported with systemic azoles, including menstrual irregularities,gynecomastia in men, <strong>and</strong> a decline in testosteronelevels. Decreased libido <strong>and</strong> temporary sterility inmen are other potential side effects. The azoles should beused with caution in pregnant patients.DRUGS FOR SUPERFICIALFUNGAL INFECTIONSSuperficial mycoses are generally not severe <strong>and</strong> patients areoften treated with topical agents. Selected agents used totreat superficial mycoses are listed in Table 35.4.35.6 Superficial <strong>Fungal</strong> <strong>Infections</strong>Superficial fungal infections of the hair, scalp, nails, <strong>and</strong> themucous membranes of the mouth <strong>and</strong> vagina are rarelymedical emergencies. <strong>Infections</strong> of the nails <strong>and</strong> skin, <strong>for</strong> example,may be ongoing <strong>for</strong> months or even years be<strong>for</strong>e apatient seeks treatment. Unlike systemic fungal infections,superficial infections may occur in any patient, not justthose who have suppressed immune systems. For example,about 75% of all adult women experience vulvovaginal c<strong>and</strong>idiasisat least once in their lifetime. Athlete’s foot (tineapedis) <strong>and</strong> jock itch (tinea cruris) are two commonly experiencedskin mycoses.Antifungal drugs applied topically are much safer thantheir systemic counterparts because penetration into thedeeper layers of the skin or mucous membranes is poor, <strong>and</strong>only small amounts are absorbed into the circulation. Adverseeffects are generally minor <strong>and</strong> limited to the regionbeing treated. Burning or stinging at the site of application,drying of the skin, rash, or contact dermatitis are the mostfrequent side effects from the topical agents.Many medications <strong>for</strong> superficial mycoses are available asover-the-counter (OTC) creams, gels, powders, <strong>and</strong> ointments.If the infection has grown into the deeper skin layers,oral antifungal drug therapy may be indicated. Extensive superficialmycoses may be treated with both oral <strong>and</strong> topicalantifungal agents to ensure that the infection is eliminatedfrom deeper skin or mucous membrane layers.Selection of a particular antifungal agent is based on thelocation of the infection <strong>and</strong> characteristics of the lesion.Griseofulvin (Fulvicin) is an inexpensive, older agent givenby the oral route that is indicated <strong>for</strong> mycoses of the hair,skin, <strong>and</strong> nails that have not responded to conventional topicalpreparations. Itraconazole (Sporanox) <strong>and</strong> terbinafine(Lamisil) are oral preparations that have the advantage ofaccumulating in nail beds, allowing them to remain activemany months after therapy is discontinued. Miconazole <strong>and</strong>TABLE 35. 4Selected <strong>Drugs</strong> <strong>for</strong> Superficial Mycoses*Drug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsbutenafine (Mentax) Topical; apply daily <strong>for</strong> 4 wk <strong>for</strong> tineas Drying of skin, stinging sensation at application site,ciclopirox cream, gel, shampoo (Loprox)pruritus, urticaria, contact dermatitisTopical; apply cream bid 4 weeks <strong>for</strong> tineasor nail lacquer (Penlac)Granulocytopenia (griseofulvin), cholestatic hepatitisTopical; apply lacquer to nail 48 wks <strong>for</strong> onychomycoses(oral terbinafine), neutropenia (oral terbinafine)griseofulvin (Fulvicin)naftifine (Naftin)nystatin: topical powder (Mycostatin,Nystop); oral suspension (Nilstat); capsule(Bio-Statin); cream, ointment (Mycostatin,Nystex)terbinafine (Lamisil)tolnaftate (Aftate,Tinactin)undecylenic acid (Fungi-Nail,Gordochom, others)PO; 500 mg microsize or 330–375 mg ultramicrosize daily <strong>for</strong>tineas <strong>and</strong> onychomycosesTopical; apply cream daily or gel bid <strong>for</strong> 4 wk <strong>for</strong> tineasPO; 500,000–1,000,000 units tidIntravaginal; 1–2 tablets daily <strong>for</strong> 2 wkTopical; apply once daily or bid 7 wk <strong>for</strong> tineasPO; 250 mg daily 6–12 wk <strong>for</strong> onychomycosesTopical; apply bid <strong>for</strong> 4–6 wkTopical; apply once or twice daily*Azole antifungal drugs <strong>for</strong> superficial infections are included in Table 35.3.Italics indicate common adverse effects; underlining indicates serious adverse effects.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 514Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 515Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 515Prototype DrugTherapeutic Class: Topical antifungal❘ Nystatin (Mycostatin, Nystop, others)Pharmacologic Class: PolyeneACTIONS AND USESADVERSE EFFECTSNystatin binds to sterols in the fungal cell membrane, causing leakage of intracellularcontents as the membrane becomes weakened. Although it belongs tothe same chemical class as amphotericin B, the polyenes, nystatin is availablein a wider variety of <strong>for</strong>mulations, including cream, ointment, powder, tablet,<strong>and</strong> lozenge. Too toxic <strong>for</strong> parenteral administration, nystatin is primarily usedtopically <strong>for</strong> c<strong>and</strong>ida infections of the vagina, skin, <strong>and</strong> mouth. It may also beused orally to treat c<strong>and</strong>idiasis of the intestine, because it travels through the GI INTERACTIONStract without being absorbed.Drug–Drug: UnknownLab Tests: UnknownADMINISTRATION ALERTS■ Apply with a swab to the affected area in infants <strong>and</strong> children, as swishingis difficult or impossible.■ For oral c<strong>and</strong>idiasis, the drug should be swished in the mouth <strong>for</strong> at least 2minutes.■ Pregnancy category C (oral preparations) or A (topical preparations)When given topically, nystatin produces few adverse effects other than minorskin irritation. There is a high incidence of contact dermatitis, related to thepreservatives found in some of the <strong>for</strong>mulations.When given orally,it may causediarrhea, nausea, <strong>and</strong> vomiting.Contraindications: The only contraindication is hypersensitivity to the drug.Herbal/Food: UnknownTreatment of Overdose: There is no specific treatment <strong>for</strong> overdose.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.PHARMACOKINETICSOnset: RapidPeak: UnknownHalf-life: UnknownDuration: 6–12 hclotrimazole are OTC drugs of choice <strong>for</strong> vulvovaginal c<strong>and</strong>idainfections, although several other medications areequally effective. Some of the therapies <strong>for</strong> vulvovaginalc<strong>and</strong>idiasis require only a single dose. Tolnaftate <strong>and</strong> undecylenicacid are frequently used to treat athlete’s foot <strong>and</strong>jock itch.PROTOZOAN INFECTIONSProtozoa are single-celled organisms that inhabit water, soil,<strong>and</strong> animal hosts. Although only a few of the more than20,000 species cause disease in humans, they cause significantmorbidity <strong>and</strong> mortality in Africa, South America,Central America, <strong>and</strong> Asia. Travelers to these continentsmay acquire these infections overseas <strong>and</strong> bring them backto the United States <strong>and</strong> Canada. These parasites oftenthrive in conditions where sanitation <strong>and</strong> personal hygieneare poor <strong>and</strong> population density is high. In addition, protozoaninfections often occur in patients who are immunocompromised,such as those in the advanced stages of AIDSor who are receiving antineoplastic drugs. Agents <strong>for</strong> malarialinfections are listed in Table 35.5.35.7 Pharmacotherapy of MalariaDrug therapy of protozoan infections is difficult because ofthe parasites’ complicated life cycles, during which they maychange <strong>for</strong>m <strong>and</strong> travel to infect distant organs. When facedwith adverse conditions, protozoans can <strong>for</strong>m cysts that allowthe pathogen to survive in harsh environments, <strong>and</strong> infectother hosts. When cysts occur inside the host, theparasite is often resistant to pharmacotherapy. With few exceptions,antibiotic, antifungal, <strong>and</strong> antiviral drugs are ineffectiveagainst protozoans.Malaria is caused by four species of the protozoanPlasmodium. Although rare in the United States <strong>and</strong>Canada, malaria is the second most common fatal infectiousdisease in the world, with 300 to 500 million cases occurringannually.Malaria begins with a bite from an infected femaleAnopheles mosquito, which is the carrier <strong>for</strong> the parasite.Once inside the human host, Plasmodium multiplies in theliver <strong>and</strong> trans<strong>for</strong>ms into progeny called merozoites. About 14to 25 days after the initial infection, the merozoites are releasedinto the blood. The merozoites infect red blood cells,which eventually rupture, releasing more merozoites, <strong>and</strong>causing severe fever <strong>and</strong> chills. This phase is called theerythrocytic stage of the infection. Plasmodium can remain in alatent state in body tissues <strong>for</strong> extended periods. Relapsesmay occur months, or even years, after the initial infection.The life cycle of Plasmodium is shown in ➤ Figure 35.1.Pharmacotherapy of malaria attempts to interrupt thecomplex life cycle of Plasmodium. Although successful earlyin the course of the disease, therapy becomes increasingly# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 515Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 516516 Unit 5 The Immune SystemTABLE 35. 5 Selected <strong>Drugs</strong> <strong>for</strong> MalariaDrug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsartemether/lumefantrine (Coartem) PO; 4 tablets twice daily <strong>for</strong> 3 days with food Headache, dizziness, anorexia, fever, arthralgia,myalgia, nauseaHypersensitivity, QT prolongationatovaquone <strong>and</strong> proguanil (Malarone)PO <strong>for</strong> prophylaxis; 1 tablet/day starting 1–2 days be<strong>for</strong>e travel,<strong>and</strong> continuing until 7 days after returnPO <strong>for</strong> treatment; 4 tablets/day <strong>for</strong> 3 daysNausea, vomiting, abdominal pain, diarrhea,headache, myalgiaNeutropenia, hypotensionchloroquine (Aralen) PO; 600 mg initial dose, then 300 mg/wk Nausea, vomiting <strong>and</strong> diarrhea; visual changes,including blurred vision, photophobia <strong>and</strong> difficultyfocusinghydroxychloroquine (Plaquenil)(see page 743 <strong>for</strong> the PrototypeDrug box)mefloquine (Lariam)primaquineFor acute attacks: PO; 620 mg initial dose, then 310 mg at 6, 18,<strong>and</strong> 28 hFor prophylaxis: PO; 310 mg starting 2 wk be<strong>for</strong>e travel <strong>and</strong>continuing 4–6 wk following returnPO; Prevention: begin 250 mg once a week <strong>for</strong> 4 wk, then 250 mgevery other weekTreatment: 1,250 mg as a single doseFor acute attacks: PO; 15 mg/day <strong>for</strong> 2 wkFor prophylaxis: PO; 15 mg/day following return <strong>for</strong> 14 daysHemolytic anemia in patients with G6PD deficiency;irreversible retinal damageVomiting, nausea, diarrhea, myalgia, dizziness,anorexia, abdominal painAV block, bradycardia, tachycardia, psychosisVomiting, nausea, diarrhea, myalgia, headache,anorexia, abdominal painHemolytic anemia in patients with G6PD deficiencypyrimethamine (Daraprim) PO; 25 mg once a week <strong>for</strong> 10 wk Vomiting, nausea, diarrhea, myalgia, abdominal painMegaloblastic anemia, leukopenia,thrombocytopeniaquinine (Quinamm)For acute attacks: PO; 650 mg tid 3 daysFor prophylaxis: 325 mg bid 6 wkVomiting, nausea, diarrheaCinchonism (tinnitus, ototoxicity, vertigo, fever, visualimpairment), hypothermia, coma, cardiovascularcollapse, agranulocytosisItalics indicate common adverse effects; underlining indicates serious adverse effects.difficult as the parasite enters different stages of its life cycle.Goals of antimalarial therapy include the following:● Prevention of the disease: Prevention of malaria is thebest therapeutic option, because the disease is verydifficult to treat after it has been acquired. The Centers<strong>for</strong> Disease Control <strong>and</strong> Prevention (CDC)recommends that travelers to infested areas receiveprophylactic antimalarial drugs prior to <strong>and</strong> duringtheir visit, <strong>and</strong> <strong>for</strong> 1 week after leaving. Chloroquine(Aralen) is the drug of choice, unless travel is to aregion known to have a high incidence of chloroquineresistantstrains.● Treatment of acute attacks: <strong>Drugs</strong> are used to interruptthe erythrocytic stage <strong>and</strong> eliminate the merozoites fromred blood cells. Treatment is most successful if begunimmediately after symptoms are recognized.Chloroquine (Aralen) is the classic antimalarial <strong>for</strong>treating the acute stage, although resistance has becomea major clinical problem. Other medications areprescribed in regions of the world where chloroquineresistance is prevalent.● Prevention of relapse: <strong>Drugs</strong> are given to eliminate thelatent <strong>for</strong>ms of Plasmodium residing in the liver.Primaquine phosphate is one of the few drugs able toeliminate hepatic cysts <strong>and</strong> achieve a total cure.In 2009, the FDA approved the use of a fixed dose combinationof artemether/lumefantrine (Coartem) to treat acute,uncomplicated malaria infections. Artemether is preparedfrom substances obtained from the Chinese herb Artemisaannua, which had been known to have antimalarial properties<strong>for</strong> over a thous<strong>and</strong> years. Lumefantrine extends the halflifeof the combination drug. Coartem is significant becauseit is very effective <strong>and</strong> offers an additional option <strong>for</strong> treatingchloroquine-resistant infections. This drug is approved <strong>for</strong>treatment, not prevention, of malaria.35.8 Pharmacotherapy ofNonmalarial <strong>Protozoan</strong> <strong>Infections</strong>Although infection by Plasmodium is the most significantprotozoan disease worldwide, infections caused by otherprotozoans affect significant numbers of people in endemic# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 516Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 517Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 517123Infected mosquitobites person.Plasmodiumtravels to liver.Merozoites divideinside hepatocytes.1245Merozoites arereleased tobloodstreamcausing fever<strong>and</strong> chills.Merozoites enterred blood cells.36Mosquito bitesperson <strong>and</strong>becomes infectedto restart cycle.465➤ Figure 35.1 Life cycle of PlasmodiumTREATING THE DIVERSE PATIENTG6PD Deficiency <strong>and</strong> AntimalarialsG6PD (glucose-6-phosphate dehydrogenase) deficiency is a genetic disorderfound in approximately 10% of African Americans <strong>and</strong> in 5% to 10% of SephardicJews, Greeks, Iranians, Filipinos, <strong>and</strong> Chinese. It is the most common genetic enzymedefect, occurring in over 400 million people worldwide. It is believed thatpeople with this deficiency in their red blood cells may have some natural immunityto malaria.Without G6PD,chloroquine <strong>and</strong> other antimalarial drugs impair themetabolism of red blood cells <strong>and</strong> may cause acute intravascular hemolysis.If thisdeficiency is suspected, the patient should be tested be<strong>for</strong>e treatment is initiated.Other drugs that should be avoided by patients with G6PD deficiency include thefluoroquinone antibiotics,sulfonamides,<strong>and</strong> phenytoin (Dilantin).areas. These infections include amebiasis, toxoplasmosis, giardiasis,cryptosporidiosis, trichomoniasis, trypanosomiasis,<strong>and</strong> leishmaniasis. <strong>Protozoan</strong>s can invade nearly anytissue in the body. For example, Plasmodia prefer erythrocytes,Giardia the colon, <strong>and</strong> Entamoeba travels to the liver.Like Plasmodium infections, the nonmalarial protozoaninfections occur more frequently in areas where publicsanitation is poor <strong>and</strong> population density is high. Drinkingwater may not be disinfected be<strong>for</strong>e consumption <strong>and</strong>may be contaminated with pathogens from human waste.In such regions, parasitic infections are endemic <strong>and</strong> contributesignificantly to mortality, especially in children,who are often more susceptible to the pathogens. Severalof these infections occur in severely immunocompromisedpatients. Each of the organisms has unique differencesin its distribution pattern <strong>and</strong> physiology. Descriptionsof common nonmalarial protozoan infections aregiven in Table 35.6.One such protozoan infection, amebiasis, affects morethan 50 million people <strong>and</strong> causes 100,000 deaths worldwide.Caused by the protozoan Entamoeba histolytica,amebiasisis common in Africa, Latin America, <strong>and</strong> Asia.Although primarily a disease of the large intestine, where itcauses ulcers, E. histolytica can invade the liver <strong>and</strong> create abscesses.The primary symptom of amebiasis is amebicdysentery, a severe <strong>for</strong>m of diarrhea. <strong>Drugs</strong> used to treat amebiasisinclude those that act directly on amoebas in the intestine<strong>and</strong> those that are administered <strong>for</strong> their systemic effectson the liver <strong>and</strong> other organs. <strong>Drugs</strong> <strong>for</strong> amebiasis <strong>and</strong> othernonmalarial protozoan infections are listed in Table 35.7.Although several treatment options are available,metronidazole (Flagyl) has been the traditional drug ofchoice <strong>for</strong> nonmalarial protozoan infections. In 2005,tinidazole (Tindamax) was approved by the FDA <strong>for</strong> treatmentof trichomoniasis, giardiasis, <strong>and</strong> amebiasis. This drugis very similar to metronidazole but has a longer duration ofaction that allows <strong>for</strong> less frequent dosing.DRUGS FOR HELMINTHIC INFECTIONSHelminths consist of various species of parasitic worms, whichhave more complex anatomy, physiology, <strong>and</strong> life cycles thanthe protozoans. Diseases due to these pathogens affect morethan 2 billion people worldwide, <strong>and</strong> are quite common in# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 517Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 518518 Unit 5 The Immune SystemNURSING PROCESS FOCUSPATIENTS RECEIVING PHARMACOTHERAPY FOR PROTOZOANOR HELMINTHIC INFECTIONSAssessmentPotential Nursing DiagnosesBaseline assessment prior to administration:■ Underst<strong>and</strong> the reason the drug has been prescribed in order to assess <strong>for</strong>therapeutic effects.■ Obtain a complete health history including neurologic, cardiovascular,respiratory, hepatic or renal disease, <strong>and</strong> the possibility of pregnancy. Obtaina drug history including allergies, including specific reactions to drugs,current prescription <strong>and</strong> OTC drugs, herbal preparations, <strong>and</strong> alcohol use. Bealert to possible drug interactions.■ Assess signs <strong>and</strong> symptoms of current infection <strong>and</strong> assess family membersor others living in the home.■ Obtain a travel history, noting dates of travel <strong>and</strong> note when currentsymptoms started in relation to travel (i.e., be<strong>for</strong>e, during, or after travel).■ Evaluate appropriate laboratory <strong>and</strong> diagnostic test findings (e.g., CBC, C&S,fecal ova <strong>and</strong> parasites, hepatic <strong>and</strong> renal function studies, ECG asappropriate).Assessment throughout administration:■ Assess <strong>for</strong> desired therapeutic effects (e.g., diminished diarrhea, chills, fever,muscle pain).■ Continue periodic monitoring of CBC, hepatic <strong>and</strong> renal function, C&S, fecalova <strong>and</strong> parasites, <strong>and</strong> ECG as appropriate.■ Assess <strong>for</strong> adverse effects: nausea, vomiting, abdominal cramping, increasingdiarrhea, drowsiness, dizziness, paresthesias, metallic taste, darkened urine,dysrhythmias, <strong>and</strong> palpitations. Severe diarrhea, especially containingmucus, blood, or pus; yellowing of sclera or skin; decreased urine output;numbness of extremities; seizures; dysrhythmias; hypotension; <strong>and</strong>tachycardia should be reported immediately.Planning: Patient Goals <strong>and</strong> Expected OutcomesThe patient will:■ Experience therapeutic effects (e.g., diminished signs <strong>and</strong> symptoms of infection, decreased fever <strong>and</strong> malaise).■ Be free from, or experience minimal, adverse effects.■ Verbalize an underst<strong>and</strong>ing of the drug’s use, adverse effects, <strong>and</strong> required precautions.■ Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider).Interventions <strong>and</strong> RationalesEnsuring therapeutic effects:■ Continue assessments as described earlier <strong>for</strong> therapeutic effects.(Diminished fever, pain, diarrhea, or signs of infection should begin soonafter taking the first dose <strong>and</strong> continue to improve.The health care providershould be notified if signs of infection remain after 3 days or if the entirecourse of treatment has been taken <strong>and</strong> signs of infection are still present.)Minimizing adverse effects:■ Continue to monitor vital signs, especially temperature if fever is present.Report undiminished fever or changes in level of consciousness to the healthcare provider immediately. (Fever should begin to diminish within 1 to 3days after starting the drug. Continued fever may be a sign of worseninginfection, adverse drug effects, or antibiotic resistance.)Implementation■■■■■■■■DiarrheaNauseaDeficient Fluid Volume (related to diarrhea, vomiting)FatigueImbalanced Nutrition, Less Than Body RequirementsPain (related to diarrhea, abdominal cramping, muscle pain)Impaired Skin Integrity (related to diarrhea)Deficient Knowledge (related drug therapy)Patient <strong>and</strong> Family Education■ Teach the patient to report a fever that does not diminish below 100°Fwithin 3 days, increasing signs <strong>and</strong> symptoms of infection, or symptomsthat remain present after taking the entire course of the drug.■ Teach the patient to not stop the antibacterial when “feeling better” but totake the entire course of the antibacterial; do not share doses with otherfamily members with similar symptoms; <strong>and</strong> return to the provider ifsymptoms have not resolved after the entire course of therapy.■Teach the patient to immediately report a fever that does not diminishbelow 100°F, or per parameters, or changes in behavior or LOC to thehealth care provider.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 518Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 520520 Unit 5 The Immune SystemNURSING PROCESS FOCUSInterventions <strong>and</strong> RationalesPatient self-administration of drug therapy:■ When administering medications, instruct the patient <strong>and</strong>/orfamily/caregiver in proper self-administration techniques followed by returndemonstration. (Proper administration increases the effectiveness of thedrug.)PATIENTS RECEIVING PHARMACOTHERAPY FOR PROTOZOANOR HELMINTHIC INFECTIONS (Continued)ImplementationEvaluation of Outcome CriteriaPatient <strong>and</strong> Family Education■Teach the patient to take the medication as follows:■ Complete the entire course of therapy unless otherwise instructed.■ Avoid or eliminate alcohol. Some medications (e.g., metronidazole)cause significant reactions when taken with alcohol <strong>and</strong> alcoholincreases adverse GI effects of many drugs.■ Take the drug with food or milk but avoid acidic beverages. If instructedto take the drug on an empty stomach, take with a full glass of water.■ Take the medication as evenly spaced throughout each day as feasible.■ Increase overall fluid intake while taking the antibacterial drug.■ Discard outdated medications or those no longer in use. Reviewmedicine cabinet twice a year <strong>for</strong> old medications.Evaluate the effectiveness of drug therapy by confirming that patient goals <strong>and</strong> expected outcomes have been met (see “Planning”).See Tables 35.5, 35.7, <strong>and</strong> 35.8 <strong>for</strong> a list of drugs to which these nursing actions apply.Prototype DrugTherapeutic Class: Antimalarial agent❘ Chloroquine (Aralen)Pharmacologic Class: Heme complexing agentACTIONS AND USESADVERSE EFFECTSDeveloped to counter the high incidence of malaria among American soldiers inthe Pacific Isl<strong>and</strong>s during World War II,chloroquine has been the prototype medication<strong>for</strong> the prophylaxis <strong>and</strong> treatment of malaria <strong>for</strong> more than 60 years.It iseffective in treating the erythrocytic stage, but has no activity against latentPlasmodium. Both chloroquine <strong>and</strong> the closely related hydroxychloroquine(Plaquenil) are also used off-label <strong>for</strong> the treatment of rheumatic <strong>and</strong> inflammatorydisorders, including lupus erythematosus <strong>and</strong> rheumatoid arthritis.Chloroquine concentrates in the food vacuoles of Plasmodium residing in redblood cells. Once in the vacuoles, it is believed to prevent the metabolism ofheme, which then builds to toxic levels within the parasite.Chloroquine can reduce the high fever of patients in the acute stage in lessthan 48 hours. It also is used to prevent malaria by being administered 2 weeksbe<strong>for</strong>e the patient enters an endemic area <strong>and</strong> continuing 4 to 6 weeks after thepatient leaves. Although chloroquine is a drug of choice, many other agents areavailable, as resistance to chloroquine is common.Lab Tests: UnknownADMINISTRATION ALERTS■ Pediatric dosage should be monitored closely,because children are susceptibleto overdose.■ If administrating IM, inject into a deep muscle <strong>and</strong> aspirate prior to injectingmedication because of its irritating effects to the tissues.■ Pregnancy category CChloroquine exhibits few serious adverse effects at low to moderate doses.Nausea<strong>and</strong> diarrhea may occur.At higher doses,CNS <strong>and</strong> cardiovascular toxicity maybe observed. Symptoms include confusion, convulsions, reduced reflexes, hypotension,<strong>and</strong> dysrhythmias. Chloroquine can cause retinal toxicity, including,blurred vision, photophobia, <strong>and</strong> difficulty focusing.Contraindications: Because chloroquine can cause retinal toxicity, it is contraindicatedin patients with pre-existing retinal or visual field changes.It is alsocontraindicated in patients with renal impairment <strong>and</strong> in those with hypersensitivityto the drug.INTERACTIONSDrug–Drug: Antacids <strong>and</strong> laxatives containing aluminum <strong>and</strong> magnesium c<strong>and</strong>ecrease chloroquine absorption <strong>and</strong> must not be given within 4 hours of each other.Chloroquine may also interfere with the response to rabies vaccine.Herbal/Food: UnknownTreatment of Overdose: Overdose may be fatal. Symptomatic treatment mayinclude anticonvulsants <strong>and</strong> vasopressors <strong>for</strong> shock. Ammonium chloride maybe used to acidify the urine to hasten excretion of chloroquine.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.PHARMACOKINETICSOnset: 8–10 hPeak: 3–4 hHalf-life: 1.5–2 daysDuration: Variable (several days to weeks)# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 520Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 521Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 521TABLE 35. 6 Selected <strong>Protozoan</strong> <strong>Infections</strong>Name of Disease <strong>and</strong><strong>Protozoan</strong> Specie(s) Description Source of InfectionAmebiasisEntamoeba histolyticaPrimarily infects the large intestine, causing severe diarrhea; commonly travels to the liver to <strong>for</strong>mliver abscesses; rarely travels to other organs such as the brain, lungs, or kidneyFecal-contaminated waterCryptosporidiosisCryptosporidium parvumGiardiasisGiardia lambliaMalariaPlasmodium (various species)ToxoplasmosisToxoplasma gondiiTrichomoniasisTrichomonas vaginalisTrypanosomiasisTrypanosoma cruzi (American)Trypanosoma brucei (African)Infects the intestines, causing diarrhea; often seen in immunocompromised patientsInfects the intestines, causing malabsorption, fatigue, <strong>and</strong> abdominal painInfects red blood cells to cause fever, chills, <strong>and</strong> fatigue; some Plasmodia invade the liver <strong>and</strong> othertissues.Can invade any organ; causes a fatal encephalitis in immunocompromised patientsCommon STD that causes vaginitis in females <strong>and</strong> urethritis in malesThe American <strong>for</strong>m (Chagas’ disease) invades cardiac tissue <strong>and</strong> autonomic ganglia; the African<strong>for</strong>m (sleeping sickness) causes fatigue <strong>and</strong> CNS depressionFecal-contaminated water;humans <strong>and</strong> other animalsFecal-contaminated waterBite of female AnophelesmosquitoCongenital transmission; catfecesTransmission through sexualcontact with infected fluidsBite of kissing bug (American)or tsetse fly (African)areas lacking high st<strong>and</strong>ards of sanitation. <strong>Helminthic</strong> infectionsin the United States <strong>and</strong> Canada are neither commonnor fatal, although drug therapy may be indicated. <strong>Drugs</strong>used to treat these infections, the anthelmintics, are listed inTable 35.8.35.9 Pharmacotherapyof <strong>Helminthic</strong> <strong>Infections</strong>Helminths are classified as roundworms (nematodes), flukes(trematodes), or tapeworms (cestodes). The most commonTABLE 35. 7Selected <strong>Drugs</strong> <strong>for</strong> Nonmalarial <strong>Protozoan</strong> <strong>Infections</strong>Drug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsiodoquinol (Yodoxin) PO; 630–650 mg tid <strong>for</strong> 20 days (max: 2 g/day) Nausea, vomiting, headache, dizzinessLoss of vision, agranulocytosis, peripheral neuropathymetronidazole (Flagyl) PO; 250–750 mg tid Dizziness, headache, anorexia, abdominal pain, metallic taste,nauseaSeizures, peripheral neuropathy, transient leukopenianifurtimox (Lampit) PO; 8–10 mg/kg three to four times/day <strong>for</strong> 90–120 days Rash, dizziness, headache, nausea/vomitingSeizures, paresthesia with myalgia, pneumoniaparomomycin (Humatin) PO; 25–35 mg/kg in three divided doses <strong>for</strong> 5–10 days Nausea, vomiting, headache, diarrhea, abdominal crampsOtotoxicity, nephrotoxicitypentamidine (Pentam,NebuPent)sodium stibogluconate(Pentostam)tinidazole (Tindamax)IV/IM; 4 mg/kg/day <strong>for</strong> 14–21 days; infuse over 60 minIM; 20 mg/kg/dayPO; giardiasis: 50 mg/kg in single dose (max: 2 g); amebiasis:2 g/day <strong>for</strong> 3–5 daysCough, bronchospasm, nausea, anorexiaLeukopenia, hypoglycemia, abscess or pain at injection site,hypotension, nephrotoxicityNausea, vomiting, diarrhea, anorexia, cough, substernal painECG changes, pneumonia, blood dyscrasiasAnorexia, metallic taste, <strong>and</strong> nauseaSeizures, peripheral neuropathy, transient leukopeniaItalics indicate common adverse effects; underlining indicates serious adverse effects.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 521Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 522522 Unit 5 The Immune SystemPrototype Drug❘ Metronidazole (Flagyl)Therapeutic Class: Anti-infective, antiprotozoanPharmacologic Class: Agent that disrupts nucleic acid synthesisACTIONS AND USESADVERSE EFFECTSMetronidazole is the prototype drug <strong>for</strong> most <strong>for</strong>ms of amebiasis, being effectiveagainst both the intestinal <strong>and</strong> hepatic stages of the disease. Resistant<strong>for</strong>ms of E. histolytica have not yet emerged as a clinical problem with metronidazoletherapy. Metronidazole is a drug of choice <strong>for</strong> two other protozoan infections:giardiasis <strong>and</strong> trichomoniasis.Metronidazole is unique among antiprotozoan drugs in that it also has antibioticactivity against anaerobic bacteria <strong>and</strong> thus is used to treat a number ofrespiratory, bone, skin, <strong>and</strong> CNS infections.Topical <strong>for</strong>ms of metronidazole (MetroGel,MetroCream, MetroLotion) are used to treat rosacea, a disease characterizedby skin reddening <strong>and</strong> hyperplasia of the sebaceous gl<strong>and</strong>s, particularlyaround the nose <strong>and</strong> face. Off-label uses include the pharmacotherapy ofpseudomembranous colitis <strong>and</strong> Crohn’s disease. Helidac is a combination drugcontaining metronidazole, bismuth, <strong>and</strong> tetracycline that is used to eradicateH. pylori infection associated with peptic ulcer disease.ADMINISTRATION ALERTS■ The extended-release <strong>for</strong>m must be swallowed whole <strong>and</strong> taken on anempty stomach.■ Contraindicated during the first trimester of pregnancy.■ Pregnancy category BAlthough adverse effects occur relatively frequently, most are not seriousenough to cause discontinuation of therapy.The most common adverse effectsof metronidazole are anorexia, nausea, diarrhea, dizziness, <strong>and</strong> headache. Drynessof the mouth <strong>and</strong> an unpleasant metallic taste may be experienced. Althoughrare, metronidazole can cause bone marrow suppression.Contraindications: Metronidazole is contraindicated in patients with trichomoniasisduring the first trimester of pregnancy <strong>and</strong> those with hypersensitivityto the drug. Metronidazole can cause bone marrow suppression; thus, it iscontraindicated <strong>for</strong> patients with blood dyscrasias.INTERACTIONSDrug–Drug: Metronidazole interacts with oral anticoagulants to potentiatehypoprothrombinemia. In combination with alcohol, or other medications that maycontain alcohol, metronidazole may elicit a disulfiram reaction. In patients takinglithium, the drug may elevate lithium levels.Lab Tests: Metronidazole may decrease values <strong>for</strong> AST <strong>and</strong> ALT.Herbal/Food: UnknownTreatment of Overdose: There is no specific treatment <strong>for</strong> overdose.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.PHARMACOKINETICS (PO)Onset: RapidPeak: 1–3 hHalf-life: 6–8 hDuration: Unknownhelminth disease worldwide is ascariasis, which is caused bythe roundworm Ascaris lumbricoides. In the United States,thisworm is most common in the Southeast,<strong>and</strong> primarily infectschildren aged 3 to 8 years, since this group is most likely to beexposed to contaminated soil without proper h<strong>and</strong> washing.Enteriobiasis, an infection by the pinworm Enterobius vermicularis,is the most common helminth infection in the UnitedStates. For ascariasis, oral mebendazole (Vermox) <strong>for</strong> 3 days isTABLE 35. 8Selected <strong>Drugs</strong> <strong>for</strong> <strong>Helminthic</strong> <strong>Infections</strong>Drug Route <strong>and</strong> Adult Dose (max dose where indicated) Adverse Effectsalbendazole (Albenza) PO; 400 mg bid with meals (max: 800 mg/day) Abnormal liver function tests, abdominal pain, nausea,vomitingAgranulocytosis, leukopeniaivermectin (Stromectol) PO; 150–200 mcg/kg as a single dose Fever, pruritus, dizziness, arthralgia, lymphadenopathyAcute allergic or inflammatory responsemebendazole (Vermox) PO; 100 mg as a single dose, or 100 mg bid <strong>for</strong> 3 days Abdominal pain, diarrhea, rashAngioedema, convulsionspraziquantel (Biltricide) PO; 5 mg/kg as a single dose, or 25 mg/kg tid Headache, dizziness, malaise, fever, abdominal painCSF reaction syndromepyrantel (Antiminth, Ascarel, Pin-X,Pinworm Caplets)PO; 11 mg/kg as a single dose (max: 1 g)Nausea, tenesmus, anorexia, diarrhea, feverNo serious adverse effectsItalics indicate common adverse effects; underlining indicates serious adverse effects.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 522Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 523Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 523the st<strong>and</strong>ard treatment. Pharmacotherapy of enterobiasis includesa single dose of mebendazole, albendazole (Albenza)or pyrantel (Antiminth, Ascarel, Pin-X, Pinworm Caplets).Like protozoans, helminths have several stages in their lifecycle, which include immature <strong>and</strong> mature <strong>for</strong>ms. Typically,the immature <strong>for</strong>ms of helminths enter the body throughthe skin or the digestive tract. Most attach to the human intestinaltract, although some species <strong>for</strong>m cysts in skeletalmuscle or in organs such as the liver.Not all helminthic infections require pharmacotherapy,because the adult parasites often die without reinfecting thehost. When the infestation is severe or complications occur,pharmacotherapy is initiated. Complications caused by extensiveinfestations may include physical obstruction in theLIFESPAN CONSIDERATIONSChildhood Play Areas <strong>and</strong> Parasitic <strong>Infections</strong>Pinworms <strong>and</strong> roundworms are more commonly seen in children because manyof their hygiene <strong>and</strong> play habits contribute to the transmission <strong>and</strong> reinfestationof the worms.Instruct parents <strong>and</strong> family members about ways to preventexposure to <strong>and</strong> spread of helminths.Teach children correct h<strong>and</strong> washing techniques,emphasizing cleansing under the nails <strong>and</strong> washing be<strong>for</strong>e eating <strong>and</strong>after using the toilet.Discourage placing h<strong>and</strong>s in mouth <strong>and</strong> biting nails.Do notallow child to scratch the anal area. Make sure that children wear shoes whenplaying outside.Avoid use of s<strong>and</strong>boxes, which can be accessed by dogs or cats;keep s<strong>and</strong>boxes covered when not in use. Cleanse all fruits <strong>and</strong> vegetables be<strong>for</strong>eeating.Change diapers frequently <strong>and</strong> dispose of properly (out of children’sreach).Do not allow children to swim in pools that allow diapered children.Discusswhole-family treatment, particularly in households with several youngchildren, if one family member has an infection.intestine, malabsorption, increased risk <strong>for</strong> secondary bacterialinfections, <strong>and</strong> severe fatigue. Pharmacotherapy is targetedat killing the parasites locally in the intestine <strong>and</strong>systemically in the tissues <strong>and</strong> organs they have invaded.Some anthelmintics have a broad spectrum <strong>and</strong> are effectiveagainst multiple organisms, whereas others are specific <strong>for</strong> acertain species. Resistance has not yet become a clinicalproblem with anthelmintics.LIFESPAN CONSIDERATIONSParasitic <strong>Infections</strong> in ChildrenMany parasitic infections are common among children,with the national rateshighest among children less than 5 years of age.In public health labs,the mostcommonly diagnosed intestinal parasite is Giardia. Giardiasis cases are associatedwith swimming in contaminated waterways or drinking contaminatedground well water, via contaminated diapers in child-care settings, <strong>and</strong> drinkingwater or consuming raw fruits or vegetables during international travel.Giardia infections may also be difficult to diagnose because stool specimens donot always contain the ova or parasites,although stool antigen testing specificto Giardia is available.Children adopted from countries outside of the United States also have ahigh rate of parasitic infection.Up to 35% of <strong>for</strong>eign-born adopted children arereported to have Giardia lamblia. Environments in which these children havebeen living,particularly orphanages,often provide favorable conditions <strong>for</strong> infectiousdisease. The CDC recommends that internationally adopted childrenundergo examination of at least one stool sample, <strong>and</strong> three stool samples ifGI symptoms are present. Un<strong>for</strong>tunately, evidence has shown that in communitieswhere helminth infections are common,whether in the United States oroverseas,poor nutritional status,anemia,<strong>and</strong> impaired growth <strong>and</strong> learning inchildren result.Prototype DrugTherapeutic Class: Anthelmintic❘ Mebendazole (Vermox)Pharmacologic Class: NoneACTIONS AND USESADVERSE EFFECTSMebendazole is the most widely prescribed anthelmintic in the United States.Itis used in the treatment of a wide range of helminth infections, including thosecaused by roundworm (Ascaris) <strong>and</strong> pinworm (Enterobiasis). As a broadspectrumdrug, it is particularly valuable in mixed helminth infections, whichare common in areas having poor sanitation.It is effective against both the adult<strong>and</strong> larval stages of these parasites. It is poorly absorbed after oral administration,which allows it to retain high concentrations in the intestine. For pinworminfections, a single dose is usually sufficient; other infections require 3 consecutivedays of therapy.Lab Tests: UnknownADMINISTRATION ALERTS■ The drug is most effective when chewed <strong>and</strong> taken with a fatty meal.■ Pregnancy category CBecause so little of the drug is absorbed, mebendazole does not generally causeserious systemic side effects. As the worms die, some abdominal pain, distension,<strong>and</strong> diarrhea may be experienced.Contraindications: The only contraindication is hypersensitivity to the drug.INTERACTIONSDrug–Drug: Carbamazepine <strong>and</strong> phenytoin can increase the metabolism ofmebendazole.Herbal/Food: High-fat foods may increase the absorption of the drug.Treatment of Overdose: There is no specific treatment <strong>for</strong> overdose.Refer to MyNursingKit <strong>for</strong> a Nursing Process Focus specific to this drug.PHARMACOKINETICSOnset: UnknownPeak: 1–7 hHalf-life: 3–9 hDuration: Unknown# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 523Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 524524 Unit 5 The Immune SystemKEY CONCEPTSChapter REVIEWThe numbered key concepts provide a succinct summary of the important points from the corresponding numbered sectionwithin the chapter. If any of these points are not clear, refer to the numbered section within the chapter <strong>for</strong> review.35.1 Fungi have more complex physiology than bacteria <strong>and</strong> areunaffected by most antibiotics. Most serious fungal infectionsoccur in patients with suppressed immune defenses.35.2 <strong>Fungal</strong> infections are classified as superficial (affectinghair, skin, nails, <strong>and</strong> mucous membranes) or systemic (affectinginternal organs).35.3 Antifungal medications act by disrupting aspects ofgrowth or metabolism that are unique to these organisms.35.4 Systemic mycoses affect internal organs <strong>and</strong> may requireprolonged <strong>and</strong> aggressive drug therapy. Amphotericin B(Fungizone) is the traditional drug of choice <strong>for</strong> seriousfungal infections.35.5 The azole class of antifungal drugs has become widelyused in the pharmacotherapy of both systemic <strong>and</strong> superficialmycoses owing to a favorable safety profile.35.6 Antifungal drugs to treat superficial mycoses may be giventopically or orally. They exhibit few serious side effects<strong>and</strong> are effective in treating infections of the skin, nails,<strong>and</strong> mucous membranes.35.7 Malaria is the most common protozoan disease <strong>and</strong> requiresmultidrug therapy owing to the complicated lifecycle of the parasite. <strong>Drugs</strong> may be administered <strong>for</strong> prophylaxis,<strong>and</strong> therapy <strong>for</strong> acute attacks <strong>and</strong> prevention ofrelapses.35.8 Treatment of non-Plasmodium protozoan disease requiresa different set of medications from those used <strong>for</strong>malaria. Other protozoan diseases that may be indications<strong>for</strong> pharmacotherapy include amebiasis, toxoplasmosis,giardiasis, cryptosporidiosis, trichomoniasis, trypanosomiasis,<strong>and</strong> leishmaniasis.35.9 Helminths are parasitic worms that cause significant diseasein certain regions of the world. The goals of pharmacotherapyare to kill the parasites locally <strong>and</strong> to disrupttheir life cycle.NCLEX-RN® REVIEW QUESTIONS1 A patient has been diagnosed with a fungal nail infection.The health care provider has prescribed fluconazole (Diflucan).The nurse will include which of the following inher patient education?1. Drug therapy will be <strong>for</strong> a very short time, probably 2 to4 weeks.2. Carefully inspect all intramuscular injection sites <strong>for</strong>bruising.3. Notify the provider should you come down withsymptoms of a bacterial infection.4. Limit fluid intake to approximately 1,000 mL/day.2 A patient is given a prescription <strong>for</strong> quinine (Quinamm)<strong>for</strong> treatment of malaria. Prior to beginning therapy, thepatient will need to:1. sign a consent <strong>for</strong>m <strong>for</strong> taking this medication.2. have an ECG done.3. stop all other medications <strong>for</strong> 24 hours.4. be admitted to an ICU <strong>for</strong> the first 24 hours of therapy.3 A patient has returned from South America, wheremalaria was contracted. A drug the nurse expects to seeused is:1. proguanil (Paludrine).2. penicillin (Ampicillin).3. rizatriptan (Maxalt).4. chloroquine (Aralen).4 The nurse is providing community education about pinworms<strong>and</strong> roundworms. Which of the following shouldbe included in this teaching? (Select all that apply.)1. H<strong>and</strong> washing is very important in preventing thespread of pinworms <strong>and</strong> roundworms.2. Play habits contribute to the transmission of pinworms<strong>and</strong> roundworms.3. It is important that children wear shoes when playingoutside.4. Children should not be allowed to play in opens<strong>and</strong>boxes.5. Once the child has had worms, reinfestation cannotoccur.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 524Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services
M35_ADAM9811_03_SE_CH35.QXD 12/30/09 11:55 AM Page 525Chapter 35 <strong>Drugs</strong> <strong>for</strong> <strong>Fungal</strong>, <strong>Protozoan</strong>, <strong>and</strong> <strong>Helminthic</strong> <strong>Infections</strong> 5255 A patient, age 32, is started on metronidazole (Flagyl) <strong>for</strong>treatment of a trichomonas vaginal infection. While she ison this medication, she must avoid:1. caffeine.2. acidic juices.3. antacids.4. alcohol.6 Metronidazole (Flagyl) is being used to treat a patient’sGiardia lamblia infection, a protozoal infection of the intestines.Which of the following are appropriate to teachthis patient? (Select all that apply.)1. Metronidazole may leave a metallic taste in the mouth.2. The urine may turn dark amber brown while on themedication.3. The metronidazole may be discontinued once thediarrhea subsides, to minimize adverse effects.4. Taking the metronidazole with food reduces GI upset.5. Current sexual partners do not require treatment <strong>for</strong>this infection.CRITICAL THINKING QUESTIONS1. A nurse is caring <strong>for</strong> a severely immunosuppressed patientwho is on IV amphotericin B (Fungizone). The nurse underst<strong>and</strong>sthat this medication is highly toxic to the patient.What are three priority nursing assessment areas <strong>for</strong>patients on this medication?2. A young female patient recently diagnosed with insulindependentdiabetes has been given a prescription <strong>for</strong>metronidazole (Flagyl) <strong>for</strong> a vaginal yeast infection. Identifypriority teaching <strong>for</strong> this patient.3. A patient is traveling to Africa <strong>for</strong> 3 months <strong>and</strong> is requestinga prescription <strong>for</strong> Malarone to prevent malaria.What premedication assessment must be done <strong>for</strong> thispatient?See Appendix D <strong>for</strong> answers <strong>and</strong> rationales <strong>for</strong> all activities.# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 525Title: Pharmacology <strong>for</strong> Nurses Server: Jobs2C/M/Y/KShort / NormalDESIGN SERVICES OFS4CARLISLEPublishing Services