Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
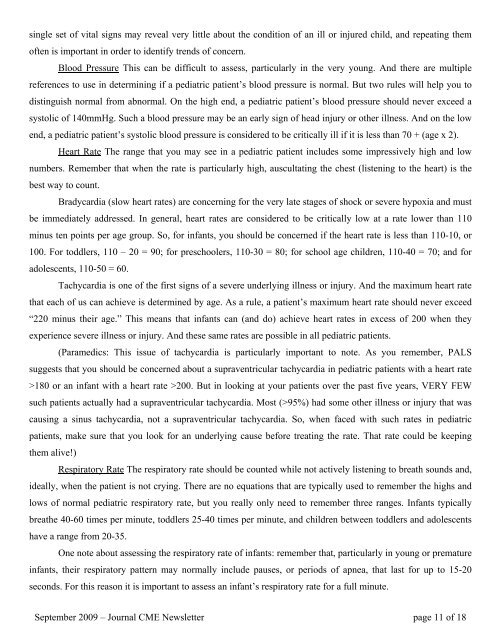
single set of vital signs may reveal very little about the condition of an ill or injured child, and repeating themoften is important in order to identify trends of concern.Blood Pressure This can be difficult to assess, particularly in the very young. And there are multiplereferences to use in determining if a pediatric patient’s blood pressure is normal. But two rules will help you todistinguish normal from abnormal. On the high end, a pediatric patient’s blood pressure should never exceed asystolic of 140mmHg. Such a blood pressure may be an early sign of head injury or other illness. And on the lowend, a pediatric patient’s systolic blood pressure is considered to be critically ill if it is less than 70 + (age x 2).Heart Rate <strong>The</strong> range that you may see in a pediatric patient includes some impressively high and lownumbers. Remember that when the rate is particularly high, auscultating the chest (listening to the heart) is thebest way to count.Bradycardia (slow heart rates) are concerning for the very late stages of shock or severe hypoxia and mustbe immediately addressed. In general, heart rates are considered to be critically low at a rate lower than 110minus ten points per age group. So, for infants, you should be concerned if the heart rate is less than 110-10, or100. For toddlers, 110 – 20 = 90; for preschoolers, 110-30 = 80; for school age children, 110-40 = 70; and foradolescents, 110-50 = 60.Tachycardia is one of the first signs of a severe underlying illness or injury. And the maximum heart ratethat each of us can achieve is determined by age. As a rule, a patient’s maximum heart rate should never exceed“220 minus their age.” This means that infants can (and do) achieve heart rates in excess of 200 when theyexperience severe illness or injury. And these same rates are possible in all pediatric patients.(Paramedics: This issue of tachycardia is particularly important to note. As you remember, PALSsuggests that you should be concerned about a supraventricular tachycardia in pediatric patients with a heart rate>180 or an infant with a heart rate >200. But in looking at your patients over the past five years, VERY FEWsuch patients actually had a supraventricular tachycardia. Most (>95%) had some other illness or injury that wascausing a sinus tachycardia, not a supraventricular tachycardia. So, when faced with such rates in pediatricpatients, make sure that you look for an underlying cause before treating the rate. That rate could be keepingthem alive!)Respiratory Rate <strong>The</strong> respiratory rate should be counted while not actively listening to breath sounds and,ideally, when the patient is not crying. <strong>The</strong>re are no equations that are typically used to remember the highs andlows of normal pediatric respiratory rate, but you really only need to remember three ranges. Infants typicallybreathe 40-60 times per minute, toddlers 25-40 times per minute, and children between toddlers and adolescentshave a range from 20-35.One note about assessing the respiratory rate of infants: remember that, particularly in young or prematureinfants, their respiratory pattern may normally include pauses, or periods of apnea, that last for up to 15-20seconds. For this reason it is important to assess an infant’s respiratory rate for a full minute.September 2009 – Journal CME <strong>News</strong>letter page 11 of 18