Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
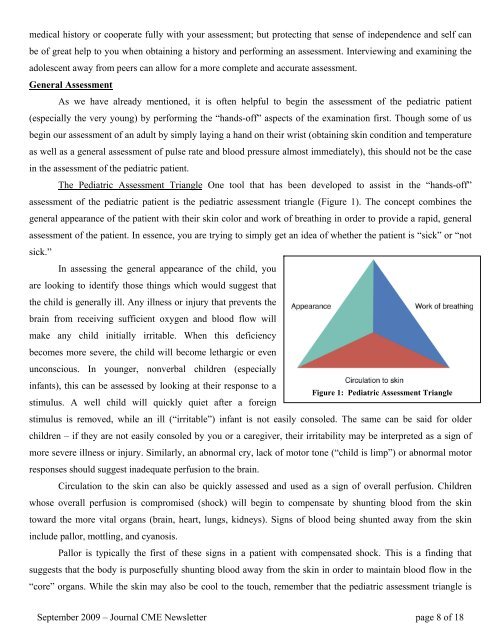
medical history or cooperate fully with your assessment; but protecting that sense of independence and self canbe of great help to you when obtaining a history and performing an assessment. Interviewing and examining theadolescent away from peers can allow for a more complete and accurate assessment.General AssessmentAs we have already mentioned, it is often helpful to begin the assessment of the pediatric patient(especially the very young) by performing the “hands-off” aspects of the examination first. Though some of usbegin our assessment of an adult by simply laying a hand on their wrist (obtaining skin condition and temperatureas well as a general assessment of pulse rate and blood pressure almost immediately), this should not be the casein the assessment of the pediatric patient.<strong>The</strong> Pediatric Assessment Triangle One tool that has been developed to assist in the “hands-off”assessment of the pediatric patient is the pediatric assessment triangle (Figure 1). <strong>The</strong> concept combines thegeneral appearance of the patient with their skin color and work of breathing in order to provide a rapid, generalassessment of the patient. In essence, you are trying to simply get an idea of whether the patient is “sick” or “notsick.”In assessing the general appearance of the child, youare looking to identify those things which would suggest thatthe child is generally ill. Any illness or injury that prevents thebrain from receiving sufficient oxygen and blood flow willmake any child initially irritable. When this deficiencybecomes more severe, the child will become lethargic or evenunconscious. In younger, nonverbal children (especiallyinfants), this can be assessed by looking at their response to aFigure 1: Pediatric Assessment Trianglestimulus. A well child will quickly quiet after a foreignstimulus is removed, while an ill (“irritable”) infant is not easily consoled. <strong>The</strong> same can be said for olderchildren – if they are not easily consoled by you or a caregiver, their irritability may be interpreted as a sign ofmore severe illness or injury. Similarly, an abnormal cry, lack of motor tone (“child is limp”) or abnormal motorresponses should suggest inadequate perfusion to the brain.Circulation to the skin can also be quickly assessed and used as a sign of overall perfusion. Childrenwhose overall perfusion is compromised (shock) will begin to compensate by shunting blood from the skintoward the more vital organs (brain, heart, lungs, kidneys). Signs of blood being shunted away from the skininclude pallor, mottling, and cyanosis.Pallor is typically the first of these signs in a patient with compensated shock. This is a finding thatsuggests that the body is purposefully shunting blood away from the skin in order to maintain blood flow in the“core” organs. While the skin may also be cool to the touch, remember that the pediatric assessment triangle isSeptember 2009 – Journal CME <strong>News</strong>letter page 8 of 18