Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
Continuing Medical Education - News & Information - The Regional ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
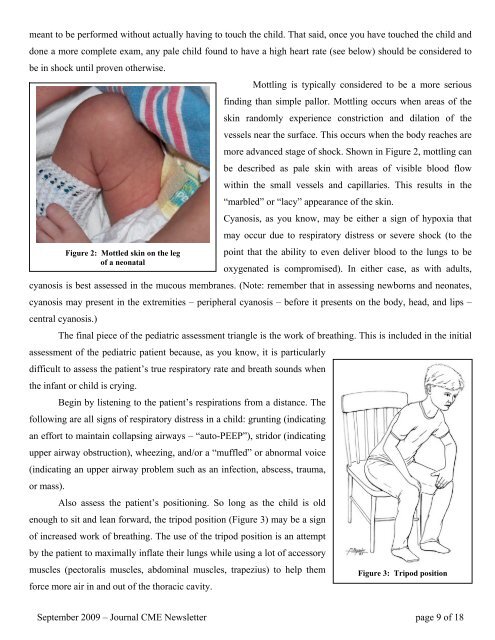
meant to be performed without actually having to touch the child. That said, once you have touched the child anddone a more complete exam, any pale child found to have a high heart rate (see below) should be considered tobe in shock until proven otherwise.Mottling is typically considered to be a more seriousfinding than simple pallor. Mottling occurs when areas of theskin randomly experience constriction and dilation of thevessels near the surface. This occurs when the body reaches aremore advanced stage of shock. Shown in Figure 2, mottling canbe described as pale skin with areas of visible blood flowwithin the small vessels and capillaries. This results in the“marbled” or “lacy” appearance of the skin.Cyanosis, as you know, may be either a sign of hypoxia thatmay occur due to respiratory distress or severe shock (to theFigure 2: Mottled skin on the leg point that the ability to even deliver blood to the lungs to beof a neonataloxygenated is compromised). In either case, as with adults,cyanosis is best assessed in the mucous membranes. (Note: remember that in assessing newborns and neonates,cyanosis may present in the extremities – peripheral cyanosis – before it presents on the body, head, and lips –central cyanosis.)<strong>The</strong> final piece of the pediatric assessment triangle is the work of breathing. This is included in the initialassessment of the pediatric patient because, as you know, it is particularlydifficult to assess the patient’s true respiratory rate and breath sounds whenthe infant or child is crying.Begin by listening to the patient’s respirations from a distance. <strong>The</strong>following are all signs of respiratory distress in a child: grunting (indicatingan effort to maintain collapsing airways – “auto-PEEP”), stridor (indicatingupper airway obstruction), wheezing, and/or a “muffled” or abnormal voice(indicating an upper airway problem such as an infection, abscess, trauma,or mass).Also assess the patient’s positioning. So long as the child is oldenough to sit and lean forward, the tripod position (Figure 3) may be a signof increased work of breathing. <strong>The</strong> use of the tripod position is an attemptby the patient to maximally inflate their lungs while using a lot of accessorymuscles (pectoralis muscles, abdominal muscles, trapezius) to help them Figure 3: Tripod positionforce more air in and out of the thoracic cavity.September 2009 – Journal CME <strong>News</strong>letter page 9 of 18