ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
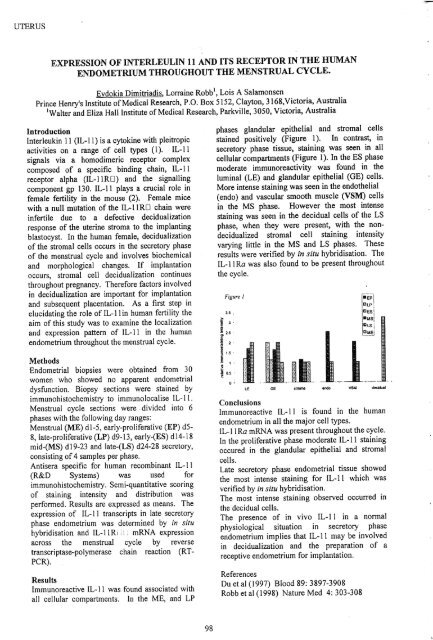
UTERUSUTERUSEXPRESSION OF INTERLEULIN 11 AND ITS RECEPTOR IN THE HUMANENDOMETRIUM THROUGHOUT THE MENSTRUAL CYCLE.Evdokia Dimitriadis, Lorraine Robb l , Lois A SalamonsenPrince Henry's Institute ofMedical Research, P.O. Box 5152, Clayton, 3168,Victoria, Australia'Walter and Eliza Hall Institute ofMedical Research, Parkville, 3050, Victoria, AustraliaIntroductionInterleukin 11 (lL-II) is a cytokine with pleitropicactivities on a range of cell types (1). IL-IIsignals via a homodimeric receptor complexcomposed of a specific binding chain, IL-llreceptor alpha (lL-IIRD) and <strong>the</strong> signallingcomponent gp 130. IL-ll plays a crucial role infemale fertility in <strong>the</strong> mouse (2). Female micewith a null mutation of <strong>the</strong> IL-l1RD chain wereinfertile due to a defective decidualizationresponse of <strong>the</strong> uterine stroma to <strong>the</strong> implantingblastocyst. In <strong>the</strong> human female, decidualizationof <strong>the</strong> stromal cells occurs in <strong>the</strong> secretory phaseof <strong>the</strong> menstrual cycle and involves biochemicaland morphological changes. If implantationoccurs, stromal cell decidualization continuesthroughout pregnancy. There<strong>for</strong>e factors involvedin· decidualization are important <strong>for</strong> implantationand subsequent placentation. As a first step inelucidating <strong>the</strong> role of IL-llin human fertility <strong>the</strong>aim of this study was to examine <strong>the</strong> localizationand expression pattern of IL-l1 in <strong>the</strong> humanendometrium throughout <strong>the</strong> menstrual cycle.MethodsEndometrial biopsies were obtained from 30women who showed no apparent endometrialdysfunction. Biopsy sections were stained byimmunohistochemistry to immunolocalise IL-ll.Menstrual cycle sections were divided into 6phases with <strong>the</strong> following day ranges:Menstrual (ME) d1-5, early-proliferative (EP) d58, late-proliferative (LP) d9-13, early-(ES) d 14-18mid-eMS) d19-23 and late-(LS) d24-28 secretory,consisting of4 samples per phase.Antisera specific <strong>for</strong> human recombinant IL-l 1(R&D Systems) was used <strong>for</strong>immunohistochemistry. Semi-quantitative scoringof staining intensity and distribution wasper<strong>for</strong>med. Results are expressed as means. Theexpression of IL-l1 transcripts in late secretoryphase endometrium was determined by in situhybridisation and IL-llR[ : mRNA expressionacross <strong>the</strong> menstrual cycle by reversetranscriptase-polymerase chain reaction (RTPCR).ResultsImmunoreactive IL-ll was found associated withall cellular compartments. In <strong>the</strong> ME, and LPphases glandular epi<strong>the</strong>lial and stromal cellsstained positively (Figure 1). In contrast, insecretory phase tissue, staining was seen in allcellular compartments (Figure 1). In <strong>the</strong> ES phasemoderate immunoreactivity was found in <strong>the</strong>luminal (LE) and glandular epi<strong>the</strong>lial (GE) cells.More intense staining was seen in <strong>the</strong> endo<strong>the</strong>lial(endo) and vascular smooth muscle (VSM) cellsin .<strong>the</strong> MS phase. However <strong>the</strong> most intensestaining was seen in <strong>the</strong> decidual cells of <strong>the</strong> LSphase, when <strong>the</strong>y were present, with <strong>the</strong> nondecidualizedstromal cell staining intensityvarying little in <strong>the</strong> MS and LS phases. Theseresults were verified by in situ hybridisation. TheIL-II Ra was also found to be present throughout<strong>the</strong> cycle.Figure 1LEGEslromaendaVSM[REP-I"ICLPI DEs!111.151j ll:lLS I~decidualConclusionsImmunoreactive IL-ll is found in <strong>the</strong> humanendometrium in all <strong>the</strong> major cell types.IL-ll Ra mRNA was present throughout <strong>the</strong> cycle.In <strong>the</strong> proliferative phase moderate IL-Il stainingoccured in <strong>the</strong> glandular epi<strong>the</strong>lial and stromalcells.Late secretory phase endometrial tissue showed<strong>the</strong> most intense staining <strong>for</strong> IL-II which wasverified by in situ hybridisation.The most intense staining observed occurred in<strong>the</strong> decidual cells.The presence of in vivo IL-II in a normalphysiological situation in secretory phaseendometrium implies that IL-II may be involvedin decidualization and <strong>the</strong> preparation of areceptive endometrium <strong>for</strong> implantation.ReferencesDu et al (1997) Blood 89: 3897-3908Robb et al (1998) Nature Med 4: 303-308INTRAUTERINE SEMINAL PLASMA INDUCES ENDOMETRIALINFLAMMATORY RESPONSE IN GILTSS. O'Leary, D.T. Annstrong, R Kamai and S.A. RobertsonDepartment ofObstetrics and Gynaecology, The University ofAdelaide, Adelaide, SA 5005IntroductionSeminal plasma (SP) has previously been thought tofunction simply as a transport and swvival medium<strong>for</strong> spermatozoa traversing <strong>the</strong> female reproductivetract However, emerging data in rodents nowindicates that factors in SP, most notablytransfonning growth factor beta (TGF~), act toevoke an inflammatory response in <strong>the</strong> uterineendometrium after insemination (1). This responseapPearS to improve implantation through inducingembryotrophic cytokine. expression and promotingimmunological tolerance to paternal transplantationantigens expressed on <strong>the</strong> semi-allogeneic conceptus.In pigs, exposure to seminal constituents has beenshown to improve litter size (2) and to influenceovarian function (3,4), but <strong>the</strong> physiologicalmechanisms mediating this effect are unknown. Theaim of this study was to begin to investigate <strong>the</strong>molecular basis of <strong>the</strong> interaction between SP and<strong>the</strong> female reproductive tract in pigs. Specifically,we have measured <strong>the</strong> acute effect of SP onleukocyte recruitment and o<strong>the</strong>r inflammatoryparameters in <strong>the</strong> uteri ofgilts.Materials and MethodsAt <strong>the</strong> onset ofgonadotrophin-induced oestrus, eightLarge White X Landrace gilts were administeredei<strong>the</strong>r seminal plasma (SP; n=4) or saline (pBS~ n=4)by transcervical infusion~ <strong>Reproductive</strong> tracts wereretrieved at autopsy 36 hours after treatment when<strong>the</strong> weight, luminal fluid content and vascular indexof uteri were scored. Endometrial tissue biopsieswere frozen in ocr and <strong>the</strong> abundance and locationof resident leukocytes were assessed byimmunohistochemical analysis of ethanol-fixedfrozen sections using monoclvnal antibodies specific<strong>for</strong> CD45 (MCAI222), :MIlC class II (MSA3), andmacrophages (HB142). Antibody reactivity (%positivity) was quantified by video image analysis.Fig. 1. The. effect of intrauterine SP infusion onleukocyte populations in <strong>the</strong> endometrium of gilts-'-- .80 -A~70f 60t1 50l:lot'$. 4090..,--------------A'1-. .-1- At II30 T • • PBS20 •A SP10it = P