ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
ruoounu. nnSlunCIS&UINI-rOSIlnS - the Society for Reproductive ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
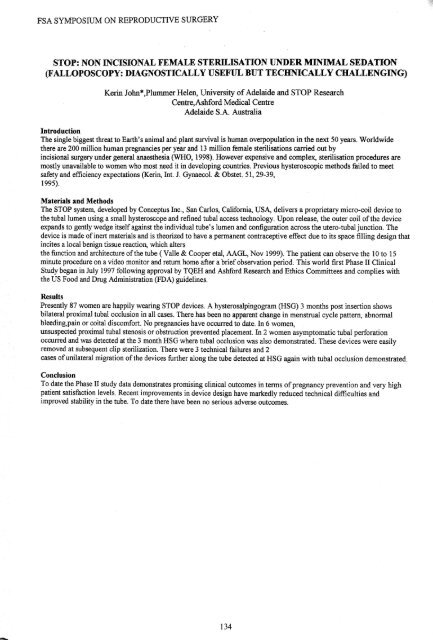
FSA SYMPOSIUM ON REPRODUCTIVE SURGERYFSA SYMPOSIUM ON REPRODUCTIVE SURGERYSTOP: NON INCISIONAL FEMALE STERILISATION UNDER MINIMAL SEDATION(FALLOPOSCOPY: DIAGNOSTICALLY USEFUL BUT TECHNICALLY CHALLENGING)Kerin John*,Plummer Helen, University ofAdelaide and STOP ResearchCentre,Ash<strong>for</strong>d Medical CentreAdelaide S.A. AustraliaIntroductionThe single biggest threat to Earth's animal and plant. survival is human overpopulation in <strong>the</strong> next 50 years. Worldwide<strong>the</strong>re are 200 million human pregnancies per year and 13 million female sterilisations carried out byincisional surgery under general anaes<strong>the</strong>sia (WHO, 1998). However expensive and complex, sterilisation procedures aremostly unavailable to women who most need it in developing countries. Previous hysteroscopic methods failed to meetsafety and efficiency expectations (Kerin, Int. 1. Gynaecol. & Obstet. 51,29-39,1995).Materials and MethodsThe STOP system, developed by Conceptus Inc., San Carlos, Cali<strong>for</strong>nia, USA, delivers a proprietary micro-coil device to<strong>the</strong> tubal lumen using a small hysteroscope and refined tubal access technology. Upon release, <strong>the</strong> outer coil of<strong>the</strong> deviceexpands to gently wedge itselfagainst <strong>the</strong> individual tube's lumen and configuration across <strong>the</strong> utero-tubal junction. Thedevice is made ofinert materials and is <strong>the</strong>orized to have a permanent contraceptive effect due to its space filling design thatincites a local benign tissue reaction, which alters<strong>the</strong> function and architecture of<strong>the</strong> tube (Valle & Cooper etal, AAGL, Nov 1999). The patient can observe <strong>the</strong> 10 to 15minute procedure on a video monitor and return home after a brief observation period. This world first Phase II ClinicalStudy began in July 1997 following approval by TQEH and Ash<strong>for</strong>d Research and Ethics Committees and complies with<strong>the</strong> US Food and Drug Administration (FDA) guidelines.ResultsPresently 87 women are happily wearing STOP devices. A hysterosalpingogram (HSG) 3 months post insertion showsbilateral proximal tubal occlusion in all cases. There has been no apparent change in menstrual cycle pattern, abnormalbleeding,pain or coital discom<strong>for</strong>t. No pregnancies have occurred to date. In 6 women,unsuspected proximal tubal stenosis or obstruction prevented placement. In 2 women asymptomatic tubal per<strong>for</strong>ationoccurred and was detected at <strong>the</strong> 3 month HSG where tubal occlusion was also demonstrated. These devices were easilyremoved at subsequent clip sterilization. There were 3 technical failures and 2cases ofunilateral migration of<strong>the</strong> devices fur<strong>the</strong>r along <strong>the</strong> tube detected at HSG again with tubal occlusion demonstrated.ConclusionTo .date th~ Pha~e II study data deJ?onstrates promising clinical outcomes in terms ofpregnancy prevention and very highpatlent satisfactiOn levels. Recent lmprovements in device design have markedly reduced technical difficulties andimproved stability in <strong>the</strong> tube. To date <strong>the</strong>re have been no serious adverse outcomes.SELECTIVE SALPINGOGRAPHY, TUBAL CATHERISATION AND TRANSCERVICALTUBAL RE-CANALISATIONRobert WoolcottLingard Fertility Centre, Newcastle, New South Wales, 2291Selective salpingography remains a specialised investigation confined to tertiary referral institutions. This is largely due to<strong>the</strong> perceived technical difficulty oftrans-cervical approach to <strong>the</strong> Fallopian tube associated with <strong>the</strong> inability to guide <strong>the</strong>cannula to <strong>the</strong> internal tubal ostia and <strong>the</strong> lack offamiliarity with fluoroscopic image intensification equipment Thetechnique is simple, easy to learn and inexpensive. There are implements available however such as <strong>the</strong> Fallopotorque tubalca<strong>the</strong>terisation set which make it simple <strong>for</strong> almost every clinician with an average knowledge ofuterine anatomy andtechnical skill to per<strong>for</strong>m this procedure. Most clinicians with hospital appointments have access to <strong>the</strong> necessaryfluoroscopic equipment to per<strong>for</strong>m <strong>the</strong> procedure. Equipment and per<strong>for</strong>mance costs are only a fraction ofthat associatedwith laparoscopic or microsurgical procedures. Selective salpingography is superior to laparoscopic dye studies as a test ofFallopian tube patency.A randomised prospective controlled study oflaparoscopic dye studies versus selective salpingography as diagnostic tests offallopian tube patency, involving 278 female patients undergoing investigation ofinfertility, demonstrated selectivesalpingography to be a superior test ofFallopian tube patency. In 16/135 (11.9%) laparoscopies diagnosed proximal tubalocclusion (PTa) versus 5/138 (3.6%) at selective salpingography (p=0.018). Fur<strong>the</strong>rmore, when apparent bilateral proximaltubal occlusion is present as determined by both laparoscopic dye studies and hysterosalpingogram (in combination),selective salpingography will enable <strong>the</strong> demonstration ofpatency in approximately 35% oftubes.There is a potential <strong>the</strong>rapeutic effect ofselective salpingography alone and <strong>the</strong> use of<strong>the</strong> technique permits immediatetreatment ofproximal tubal occlusion. Selective salpingography involving tubal ca<strong>the</strong>terisation with or without wire guidecannulation is deemed by <strong>the</strong> American <strong>Society</strong> of<strong>Reproductive</strong> Medicine to be <strong>the</strong> management ofchoice where PTO ispresent alone without distal tubal disease. (American Fertility <strong>Society</strong>. 1993). There appears to be a significant <strong>the</strong>rapeuticeffect ofselective salpingography alone, which is consistent with apparent benefit ofHSG on pregnancy rates. There isadifferential impact ofselective salpingography, tubal ca<strong>the</strong>terisation and wire guide re-canalisation on pregnancy rates when<strong>the</strong>se procedures are per<strong>for</strong>med sequentially on a single occasion <strong>for</strong> <strong>the</strong> diagnosis and treatment ofapparent PTa. Crudepregnancy rates of20% <strong>for</strong> selective salpingography, 39% <strong>for</strong> tubal ca<strong>the</strong>terisation and 13% <strong>for</strong> wire guide re-canalisationhave been achieved.Falloposcopy is a logical investigative extension ofabnormalities discovered by selective salpingography. Shouldmicrosurgical resection and re-anastomosis be contemplated due to an inability to achieve patency via trans-cervicalmethods <strong>the</strong>n trans-fimbrial salpingoscopy is a wiser method ofendosalpingeal assessment. Apparent proximal tubalocclusion as diagnosed by selective salpingography identifies a sub-group ofpatient at high rsik ofhaving endometriosis.The association between endometriosis and PTa needs fur<strong>the</strong>r investigation. Endometriosis is present in approximately70% ofpatients with proximal occlusion and o<strong>the</strong>rwise normal tubes and PTa is present in 5-10% ofwomen wi<strong>the</strong>ndometriosis.Selective Salpingography should be considered <strong>the</strong> 'gold standard' testofFallopian Tube patency. It has bothdiagnostic and <strong>the</strong>rapeutic advantages over o<strong>the</strong>r methods and as such should be adopted more widely into routine clinicalpractice by general gynaecologists and infertility specialists alike.134135