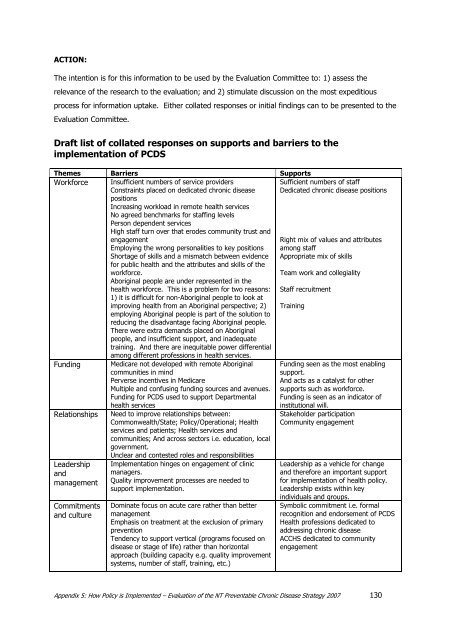
ACTION:The intention is for this information to be used by the <strong>Evaluation</strong> Committee to: 1) assess therelevance of the research to the evaluation; and 2) stimulate discussion on the most expeditiousprocess for information uptake. Either collated responses or initial findings can to be presented to the<strong>Evaluation</strong> Committee.Draft list of collated responses on supports and barriers to theimplementation of <strong>PCD</strong>SThemes Barriers SupportsWorkforce Insufficient numbers of service providersConstraints placed on dedicated chronic diseasepositionsIncreasing workload in remote health servicesNo agreed benchmarks for staffing levelsPerson dependent servicesHigh staff turn over that erodes community trust andengagementEmploying the wrong personalities to key positionsShortage of skills and a mismatch between evidencefor public health and the attributes and skills of theworkforce.Aboriginal people are under represented in thehealth workforce. This is a problem for two reasons:1) it is difficult for non-Aboriginal people to look atimproving health from an Aboriginal perspective; 2)employing Aboriginal people is part of the solution toreducing the disadvantage facing Aboriginal people.There were extra demands placed on Aboriginalpeople, and insufficient support, and inadequatetraining. And there are inequitable power differentialamong different professions in health services.TrainingFundingRelationshipsLeadershipandmanagementCommitmentsand cultureMedicare not developed with remote Aboriginalcommunities in mindPerverse incentives in MedicareMultiple and confusing funding sources and avenues.Funding for <strong>PCD</strong>S used to support Departmentalhealth servicesNeed to improve relationships between:Commonwealth/State; Policy/Operational; <strong>Health</strong>services and patients; <strong>Health</strong> services andcommunities; And across sectors i.e. education, localgovernment.Unclear and contested roles and responsibilitiesImplementation hinges on engagement of clinicmanagers.Quality improvement processes are needed tosupport implementation.Dominate focus on acute care rather than bettermanagementEmphasis on treatment at the exclusion of primarypreventionTendency to support vertical (programs focused ondisease or stage of life) rather than horizontalapproach (building capacity e.g. quality improvementsystems, number of staff, training, etc.)Sufficient numbers of staffDedicated chronic disease positionsRight mix of values and attributesamong staffAppropriate mix of skillsTeam work and collegialityStaff recruitmentFunding seen as the most enablingsupport.And acts as a catalyst for othersupports such as workforce.Funding is seen as an indicator ofinstitutional will.Stakeholder participationCommunity engagementLeadership as a vehicle for changeand therefore an important supportfor implementation of health policy.Leadership exists within keyindividuals and groups.Symbolic commitment i.e. formalrecognition and endorsement of <strong>PCD</strong>S<strong>Health</strong> professions dedicated toaddressing chronic diseaseACCHS dedicated to communityengagementAppendix 5: How Policy is Implemented – <strong>Evaluation</strong> of the <strong>NT</strong> Preventable Chronic Disease <strong>Strategy</strong> 2007 130
References1. Dunham, H., Ministerial Statement: Preventable Chronic Disease <strong>Strategy</strong> <strong>NT</strong> LegislativeAssembly, 8th Assembly, First Session, 10th Aug, Parliamentary Record No18,. 1999, <strong>NT</strong>Legislative Assembly: Darwin.2. <strong>NT</strong>DHCS, Annual Report 2005-2006. 2007, Northern Territory Department of <strong>Health</strong> andCommunity Services.3. Li, S.Q., S. Guthridge, E.T. d'Espaiget, and B. Paterson, From Infancy to Youngadulthood: <strong>Health</strong> status in the <strong>NT</strong>. 2007, Dept <strong>Health</strong> and Community Services: Darwin.4. OCPE, Northern Territory Public Sector Indigenous Employment & Career Development<strong>Strategy</strong> 2002-2006: Progress Report for the period of July 2005 to December 2005,Office of the Commissioner of Public Employment. Retrieved 26.6.2007http://www.nt.gov.au/ocpe/indigenous/progressreports/iecdsprogrepjuldec2005.pdf5. ABS, Social circumstances of Aboriginal and Torres Strait Islander Peoples: Populationcharacteristics, Australian Social Trends, Cat No 4102.0. 2005b, Aust Bureau of Statistics:Canberra.6. ABS, Housing and Infrastructure in Aboriginal and Torres Strait Islander Communities,Australia 2006, Australian Bureau of Statistics. Retrieved 27.6.2007http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/E4705677FB7487A2CA2572BF001962CE/$File/47100_2006.pdf7. Bailie, R., D. Si, M. Dowden, and K. Lonergan, Audit and Best Practice for ChronicDisease: Project Final Report. 2007, Menzies School of <strong>Health</strong> Research and TheCooperative Research Centre for Aboriginal <strong>Health</strong>: Darwin8. <strong>NT</strong>DHCS, Preventable chronic disease strategy statistical report 2000. 2001,Epidemiology Branch and Aboriginal <strong>Health</strong>, Community <strong>Health</strong> and Hospital ServicesUnit, Territory <strong>Health</strong> Services: Darwin.9. Weeramanthri TS and L. Clark, Chronic diseases in The health and welfare ofTerritorians, W.G. Condon JR, Arnold L, Editor. 2001, Territory <strong>Health</strong> Services: Darwin.p. 97-104.10. Dunham, H., Ministerial Statement: Preventable Chronic Disease <strong>Strategy</strong> <strong>NT</strong> LegislativeAssembly, 8th Assembly, First Session, 10th Aug, Parliamentary Record No18. 1999, <strong>NT</strong>Legislative Assembly: Darwin.11. Byron P, Zhao Y, and S. Guthridge, Medicare and Pharmaceutical Benefits Scheme usagepatterns in the Northern Territory 1993/94 to 2003/04. 2005, <strong>NT</strong> Department of <strong>Health</strong>and Community Services: Darwin.12. Weeramanthri, T., S. Hendy, C. Connors, D. Ashbridge, C. Rae, M. Dunn, M. Fittock, J.Cleary, L. O'Donaghue, S. Morton, and N. Swanson, The Northern Territory PreventableChronic Disease <strong>Strategy</strong> - promoting an integrated and life course approach to chronicdisease in Australia. Australian <strong>Health</strong> Review, 2003. 26(3): p. 31-42.13. Weeramanthri, T., S. Morton, S. Hendy, C. Connors, C. Rae, and D. Ashbridge, <strong>NT</strong>Preventable Chronic Disease <strong>Strategy</strong> - Overview and Framework, Northern TerritoryDepartment of <strong>Health</strong> and Community Services. Retrieved 17 January14. Weeramanthri, T. and K. Edmond, Northern Territory Preventable Chronic Disease<strong>Strategy</strong> - the Evidence Base, Territory <strong>Health</strong> Services. Retrieved 17 January15. Australian Government, Budget Paper 1996-97. <strong>Health</strong>. Retreived June 8 2005. 1997.16. Weeramanthri, T., C. Connors, et al., Chronic disease guidelines and the IndigenousCoordinated Care Trials. Australian <strong>Health</strong> Review, 2002. 25(2): p. 1-6.References – <strong>Evaluation</strong> of the <strong>NT</strong> Preventable Chronic Disease <strong>Strategy</strong> 2007 131
- Page 1 and 2:
Pty LtdABN 82 147 637 101AN EVALUAT
- Page 3 and 4:
TABLE OF CONTENTSList of figuresLis
- Page 5 and 6:
6.6 Indigenous workforce 996.7 Prev
- Page 7 and 8:
List of AbbreviationsABCDACCHOsACIC
- Page 9 and 10:
ACKNOWLEDGEMENTSWe would like to ac
- Page 11 and 12:
However the extraordinary number of
- Page 13 and 14:
the establishment of the Sunrise He
- Page 15 and 16:
RECOMMENDATIONSGeneral recommendati
- Page 17 and 18:
Exploration of joint funding arrang
- Page 19 and 20:
CHAPTER 1. INTRODUCTION1.1 Backgrou
- Page 21 and 22:
Choosing the 5 chronic conditionsTh
- Page 23 and 24:
Table 1.1Key Result Areas + Best Bu
- Page 25 and 26:
prior to the launch of NTPCDS, such
- Page 27 and 28:
Year * Action Outcome1999 S NT Prev
- Page 29 and 30:
Year * Action Outcome2005 P Aborigi
- Page 31 and 32:
CHAPTER 2.EVALUATION METHODOLOGYThe
- Page 33 and 34:
2.2 Evaluation StagesThe NTPCDS eva
- Page 35 and 36:
chronic disease activities funded t
- Page 37 and 38:
internal project team. It was very
- Page 39 and 40:
Situation at Baseline1. The Guideli
- Page 41 and 42:
3.1.2 Patient information and recal
- Page 43 and 44:
Ferret Miwatj, Numbulwar, Marngarr,
- Page 45 and 46:
Medicare information is not for pub
- Page 47 and 48:
was in place in Central Australia i
- Page 49 and 50:
What orientation and ongoing traini
- Page 51 and 52:
programs focus on chronic disease p
- Page 53 and 54:
The information collected as part o
- Page 55 and 56:
Assessment against objectiveMost se
- Page 57 and 58:
career development, and retention i
- Page 59 and 60:
are. Indigenous employment is NTDH&
- Page 61 and 62:
NTDH&CS Programs that encourage Hea
- Page 63 and 64:
2002 Aboriginal and Torres Strait I
- Page 65 and 66:
delivering any prevention and healt
- Page 67 and 68:
The Community Services Division - A
- Page 69 and 70:
1 x AHW Central Australia 2001 S100
- Page 71 and 72:
One clinic stated it had no care pl
- Page 73 and 74:
Identifies priority practices to in
- Page 75 and 76:
There has been a significant growth
- Page 77 and 78:
about 25 per cent of the hospital b
- Page 79 and 80:
The level of funding provided by th
- Page 81 and 82:
Central Australia and two zones cur
- Page 83 and 84:
The diabetes education teams at HLN
- Page 85 and 86:
maintenance group for people with l
- Page 87 and 88:
Rebates for participating or arrang
- Page 89 and 90:
Use of Medicine Programmes. Althoug
- Page 91 and 92:
CHAPTER 4. CLINICAL OUTCOMES OF THE
- Page 93 and 94:
improvements have been made to serv
- Page 95 and 96:
A recent ten-year follow-up of a co
- Page 97 and 98: The NTDH&CS also collect birthweigh
- Page 99 and 100: Figure 5.3 Vaccination coverage for
- Page 101 and 102: It is also important to note that k
- Page 103 and 104: eported that 50 per cent of the Ind
- Page 105 and 106: The current action plan identifies
- Page 107 and 108: The availability and cost of health
- Page 109 and 110: Hoy et al in 1995-2000 (100) , and
- Page 111 and 112: 5.6 Best practice management5.6.1 P
- Page 113 and 114: disease care in urban areas regardi
- Page 115 and 116: PCIS was developed by NTDH&CS as th
- Page 117 and 118: emote staff can access training and
- Page 119 and 120: In the Top End there appeared to be
- Page 121 and 122: APPENDIX 1EVALUATION OF THE NT PREV
- Page 123 and 124: 2.10 Generally speaking, on a scale
- Page 125 and 126: 4.4 Briefly recount any anecdotes y
- Page 127 and 128: 5.9 Generally speaking, on a scale
- Page 129 and 130: Section 8 • Summary questions8.1
- Page 131 and 132: Preventable Chronic Disease Program
- Page 133 and 134: Year Type Background What is it? /
- Page 135 and 136: Year Type Background What is it? /
- Page 137 and 138: An important background to this stu
- Page 139 and 140: New beliefs do not replace the old,
- Page 141 and 142: Other services are provided to the
- Page 143 and 144: ecame the main priority in many peo
- Page 145 and 146: to be healthy, how to get rid of di
- Page 147: (Draft Version - © August 2006 Jan
- Page 151 and 152: 35. Smith, J.D., Progress report fo
- Page 153 and 154: Research Centre for Aboriginal Heal
- Page 155: 114. Senior, K., 'A Gudbala Laif? h