The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
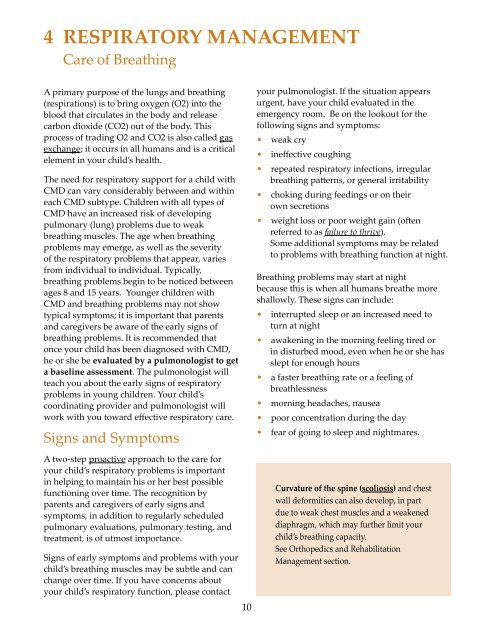
4 Respiratory <strong>Management</strong>Care <strong>of</strong> BreathingA primary purpose <strong>of</strong> the lungs and breathing(respirations) is to bring oxygen (O2) into theblood that circulates in the body and releasecarbon dioxide (CO2) out <strong>of</strong> the body. Thisprocess <strong>of</strong> trading O2 and CO2 is also called gasexchange; it occurs in all humans and is a criticalelement in your child’s health.<strong>The</strong> need for respiratory support for a child with<strong>CMD</strong> can vary considerably between and withineach <strong>CMD</strong> subtype. Children with all types <strong>of</strong><strong>CMD</strong> have an increased risk <strong>of</strong> developingpulmonary (lung) problems due to weakbreathing muscles. <strong>The</strong> age when breathingproblems may emerge, as well as the severity<strong>of</strong> the respiratory problems that appear, variesfrom individual to individual. Typically,breathing problems begin to be noticed betweenages 8 and 15 years. Younger children with<strong>CMD</strong> and breathing problems may not showtypical symptoms; it is important that parentsand caregivers be aware <strong>of</strong> the early signs <strong>of</strong>breathing problems. It is recommended thatonce your child has been diagnosed with <strong>CMD</strong>,he or she be evaluated by a pulmonologist to geta baseline assessment. <strong>The</strong> pulmonologist willteach you about the early signs <strong>of</strong> respiratoryproblems in young children. Your child’scoordinating provider and pulmonologist willwork with you toward effective respiratory care.Signs and SymptomsA two-step proactive approach to the care foryour child’s respiratory problems is importantin helping to maintain his or her best possiblefunctioning over time. <strong>The</strong> recognition byparents and caregivers <strong>of</strong> early signs andsymptoms, in addition to regularly scheduledpulmonary evaluations, pulmonary testing, andtreatment, is <strong>of</strong> utmost importance.Signs <strong>of</strong> early symptoms and problems with yourchild’s breathing muscles may be subtle and canchange over time. If you have concerns aboutyour child’s respiratory function, please contact10your pulmonologist. If the situation appearsurgent, have your child evaluated in theemergency room. Be on the lookout for thefollowing signs and symptoms:• weak cry• ineffective coughing• repeated respiratory infections, irregularbreathing patterns, or general irritability• choking during feedings or on theirown secretions• weight loss or poor weight gain (<strong>of</strong>tenreferred to as failure to thrive).Some additional symptoms may be relatedto problems with breathing function at night.Breathing problems may start at nightbecause this is when all humans breathe moreshallowly. <strong>The</strong>se signs can include:• interrupted sleep or an increased need toturn at night• awakening in the morning feeling tired orin disturbed mood, even when he or she hasslept for enough hours• a faster breathing rate or a feeling <strong>of</strong>breathlessness• morning headaches, nausea• poor concentration during the day• fear <strong>of</strong> going to sleep and nightmares.Curvature <strong>of</strong> the spine (scoliosis) and chestwall deformities can also develop, in partdue to weak chest muscles and a weakeneddiaphragm, which may further limit yourchild’s breathing capacity.See Orthopedics and Rehabilitation<strong>Management</strong> section.