The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
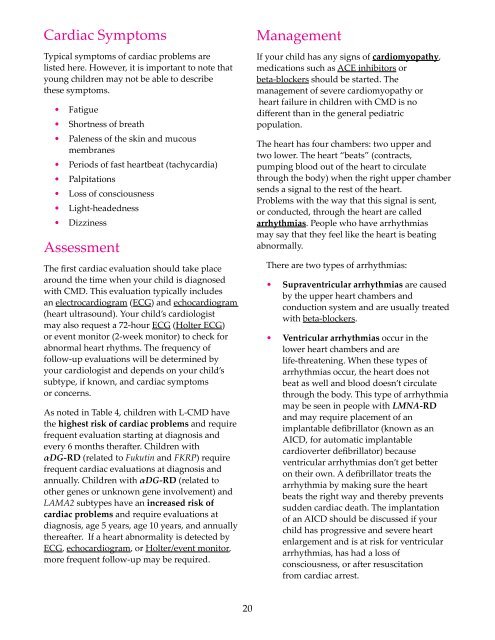
Cardiac SymptomsTypical symptoms <strong>of</strong> cardiac problems arelisted here. However, it is important to note thatyoung children may not be able to describethese symptoms.• Fatigue• Shortness <strong>of</strong> breath• Paleness <strong>of</strong> the skin and mucousmembranes• Periods <strong>of</strong> fast heartbeat (tachycardia)• Palpitations• Loss <strong>of</strong> consciousness• Light-headedness• DizzinessAssessment<strong>The</strong> first cardiac evaluation should take placearound the time when your child is diagnosedwith <strong>CMD</strong>. This evaluation typically includesan electrocardiogram (ECG) and echocardiogram(heart ultrasound). Your child’s cardiologistmay also request a 72-hour ECG (Holter ECG)or event monitor (2-week monitor) to check forabnormal heart rhythms. <strong>The</strong> frequency <strong>of</strong>follow-up evaluations will be determined byyour cardiologist and depends on your child’ssubtype, if known, and cardiac symptomsor concerns.As noted in Table 4, children with L-<strong>CMD</strong> havethe highest risk <strong>of</strong> cardiac problems and requirefrequent evaluation starting at diagnosis andevery 6 months therafter. Children withαDG-RD (related to Fukutin and FKRP) requirefrequent cardiac evaluations at diagnosis andannually. Children with αDG-RD (related toother genes or unknown gene involvement) andLAMA2 subtypes have an increased risk <strong>of</strong>cardiac problems and require evaluations atdiagnosis, age 5 years, age 10 years, and annuallythereafter. If a heart abnormality is detected byECG, echocardiogram, or Holter/event monitor,more frequent follow-up may be required.<strong>Management</strong>If your child has any signs <strong>of</strong> cardiomyopathy,medications such as ACE inhibitors orbeta-blockers should be started. <strong>The</strong>management <strong>of</strong> severe cardiomyopathy orheart failure in children with <strong>CMD</strong> is nodifferent than in the general pediatricpopulation.<strong>The</strong> heart has four chambers: two upper andtwo lower. <strong>The</strong> heart “beats” (contracts,pumping blood out <strong>of</strong> the heart to circulatethrough the body) when the right upper chambersends a signal to the rest <strong>of</strong> the heart.Problems with the way that this signal is sent,or conducted, through the heart are calledarrhythmias. People who have arrhythmiasmay say that they feel like the heart is beatingabnormally.<strong>The</strong>re are two types <strong>of</strong> arrhythmias:• Supraventricular arrhythmias are causedby the upper heart chambers andconduction system and are usually treatedwith beta-blockers.• Ventricular arrhythmias occur in thelower heart chambers and arelife-threatening. When these types <strong>of</strong>arrhythmias occur, the heart does notbeat as well and blood doesn’t circulatethrough the body. This type <strong>of</strong> arrhythmiamay be seen in people with LMNA-RDand may require placement <strong>of</strong> animplantable defibrillator (known as anAICD, for automatic implantablecardioverter defibrillator) becauseventricular arrhythmias don’t get betteron their own. A defibrillator treats thearrhythmia by making sure the heartbeats the right way and thereby preventssudden cardiac death. <strong>The</strong> implantation<strong>of</strong> an AICD should be discussed if yourchild has progressive and severe heartenlargement and is at risk for ventriculararrhythmias, has had a loss <strong>of</strong>consciousness, or after resuscitationfrom cardiac arrest.20