The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
The Management of Congenital Muscular Dystrophy ... - Cure CMD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
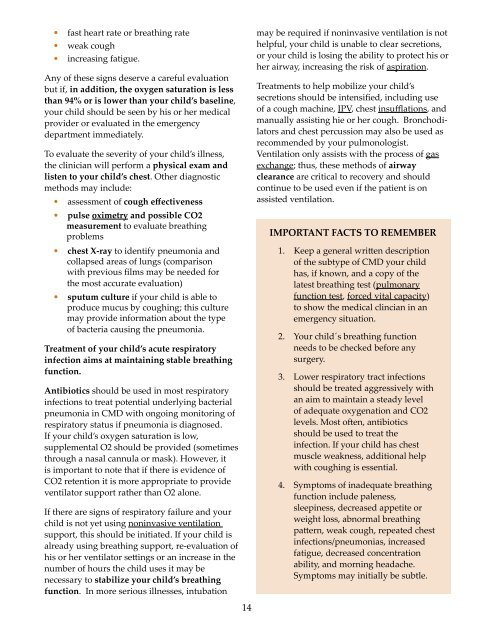
• fast heart rate or breathing rate• weak cough• increasing fatigue.Any <strong>of</strong> these signs deserve a careful evaluationbut if, in addition, the oxygen saturation is lessthan 94% or is lower than your child’s baseline,your child should be seen by his or her medicalprovider or evaluated in the emergencydepartment immediately.To evaluate the severity <strong>of</strong> your child’s illness,the clinician will perform a physical exam andlisten to your child’s chest. Other diagnosticmethods may include:• assessment <strong>of</strong> cough effectiveness• pulse oximetry and possible CO2measurement to evaluate breathingproblems• chest X-ray to identify pneumonia andcollapsed areas <strong>of</strong> lungs (comparisonwith previous films may be needed forthe most accurate evaluation)• sputum culture if your child is able toproduce mucus by coughing; this culturemay provide information about the type<strong>of</strong> bacteria causing the pneumonia.Treatment <strong>of</strong> your child’s acute respiratoryinfection aims at maintaining stable breathingfunction.Antibiotics should be used in most respiratoryinfections to treat potential underlying bacterialpneumonia in <strong>CMD</strong> with ongoing monitoring <strong>of</strong>respiratory status if pneumonia is diagnosed.If your child’s oxygen saturation is low,supplemental O2 should be provided (sometimesthrough a nasal cannula or mask). However, itis important to note that if there is evidence <strong>of</strong>CO2 retention it is more appropriate to provideventilator support rather than O2 alone.If there are signs <strong>of</strong> respiratory failure and yourchild is not yet using noninvasive ventilationsupport, this should be initiated. If your child isalready using breathing support, re-evaluation <strong>of</strong>his or her ventilator settings or an increase in thenumber <strong>of</strong> hours the child uses it may benecessary to stabilize your child’s breathingfunction. In more serious illnesses, intubationmay be required if noninvasive ventilation is nothelpful, your child is unable to clear secretions,or your child is losing the ability to protect his orher airway, increasing the risk <strong>of</strong> aspiration.Treatments to help mobilize your child’ssecretions should be intensified, including use<strong>of</strong> a cough machine, IPV, chest insufflations, andmanually assisting hie or her cough. Bronchodilatorsand chest percussion may also be used asrecommended by your pulmonologist.Ventilation only assists with the process <strong>of</strong> gasexchange; thus, these methods <strong>of</strong> airwayclearance are critical to recovery and shouldcontinue to be used even if the patient is onassisted ventilation.IMPORTANT FACTS TO REMEMBER1. Keep a general written description<strong>of</strong> the subtype <strong>of</strong> <strong>CMD</strong> your childhas, if known, and a copy <strong>of</strong> thelatest breathing test (pulmonaryfunction test, forced vital capacity)to show the medical clincian in anemergency situation.2. Your child´s breathing functionneeds to be checked before anysurgery.3. Lower respiratory tract infectionsshould be treated aggressively withan aim to maintain a steady level<strong>of</strong> adequate oxygenation and CO2levels. Most <strong>of</strong>ten, antibioticsshould be used to treat theinfection. If your child has chestmuscle weakness, additional helpwith coughing is essential.4. Symptoms <strong>of</strong> inadequate breathingfunction include paleness,sleepiness, decreased appetite orweight loss, abnormal breathingpattern, weak cough, repeated chestinfections/pneumonias, increasedfatigue, decreased concentrationability, and morning headache.Symptoms may initially be subtle.14