Change in the accommodative convergence per unit of ...
Change in the accommodative convergence per unit of ...
Change in the accommodative convergence per unit of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
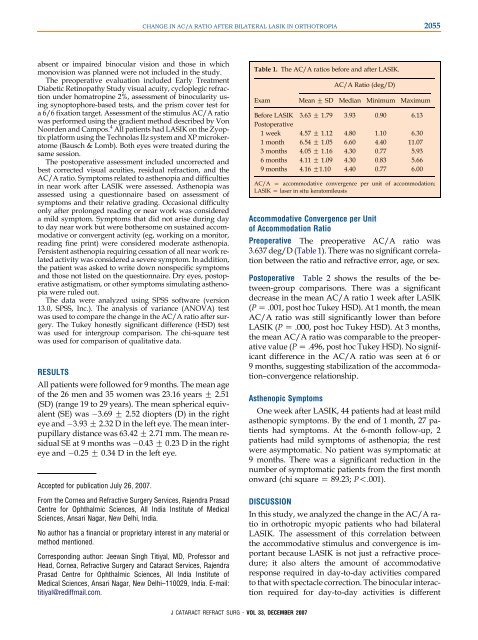
CHANGE IN AC/A RATIO AFTER BILATERAL LASIK IN ORTHOTROPIA2055absent or impaired b<strong>in</strong>ocular vision and those <strong>in</strong> whichmonovision was planned were not <strong>in</strong>cluded <strong>in</strong> <strong>the</strong> study.The preo<strong>per</strong>ative evaluation <strong>in</strong>cluded Early TreatmentDiabetic Ret<strong>in</strong>opathy Study visual acuity, cycloplegic refractionunder homatrop<strong>in</strong>e 2%, assessment <strong>of</strong> b<strong>in</strong>ocularity us<strong>in</strong>gsynoptophore-based tests, and <strong>the</strong> prism cover test fora 6/6 fixation target. Assessment <strong>of</strong> <strong>the</strong> stimulus AC/A ratiowas <strong>per</strong>formed us<strong>in</strong>g <strong>the</strong> gradient method described by VonNoorden and Campos. 4 All patients had LASIK on <strong>the</strong> Zyoptixplatform us<strong>in</strong>g <strong>the</strong> Technolas IIz system and XP microkeratome(Bausch & Lomb). Both eyes were treated dur<strong>in</strong>g <strong>the</strong>same session.The posto<strong>per</strong>ative assessment <strong>in</strong>cluded uncorrected andbest corrected visual acuities, residual refraction, and <strong>the</strong>AC/A ratio. Symptoms related to as<strong>the</strong>nopia and difficulties<strong>in</strong> near work after LASIK were assessed. As<strong>the</strong>nopia wasassessed us<strong>in</strong>g a questionnaire based on assessment <strong>of</strong>symptoms and <strong>the</strong>ir relative grad<strong>in</strong>g. Occasional difficultyonly after prolonged read<strong>in</strong>g or near work was considereda mild symptom. Symptoms that did not arise dur<strong>in</strong>g dayto day near work but were bo<strong>the</strong>rsome on susta<strong>in</strong>ed <strong>accommodative</strong>or convergent activity (eg, work<strong>in</strong>g on a monitor,read<strong>in</strong>g f<strong>in</strong>e pr<strong>in</strong>t) were considered moderate as<strong>the</strong>nopia.Persistent as<strong>the</strong>nopia requir<strong>in</strong>g cessation <strong>of</strong> all near work relatedactivity was considered a severe symptom. In addition,<strong>the</strong> patient was asked to write down nonspecific symptomsand those not listed on <strong>the</strong> questionnaire. Dry eyes, posto<strong>per</strong>ativeastigmatism, or o<strong>the</strong>r symptoms simulat<strong>in</strong>g as<strong>the</strong>nopiawere ruled out.The data were analyzed us<strong>in</strong>g SPSS s<strong>of</strong>tware (version13.0, SPSS, Inc.). The analysis <strong>of</strong> variance (ANOVA) testwas used to compare <strong>the</strong> change <strong>in</strong> <strong>the</strong> AC/A ratio after surgery.The Tukey honestly significant difference (HSD) testwas used for <strong>in</strong>tergroup comparison. The chi-square testwas used for comparison <strong>of</strong> qualitative data.RESULTSAll patients were followed for 9 months. The mean age<strong>of</strong> <strong>the</strong> 26 men and 35 women was 23.16 years G 2.51(SD) (range 19 to 29 years). The mean spherical equivalent(SE) was 3.69 G 2.52 diopters (D) <strong>in</strong> <strong>the</strong> righteye and 3.93 G 2.32 D <strong>in</strong> <strong>the</strong> left eye. The mean <strong>in</strong>terpupillarydistance was 63.42 G 2.71 mm. The mean residualSE at 9 months was 0.43 G 0.23 D <strong>in</strong> <strong>the</strong> righteye and 0.25 G 0.34 D <strong>in</strong> <strong>the</strong> left eye.Accepted for publication July 26, 2007.From <strong>the</strong> Cornea and Refractive Surgery Services, Rajendra PrasadCentre for Ophthalmic Sciences, All India Institute <strong>of</strong> MedicalSciences, Ansari Nagar, New Delhi, India.No author has a f<strong>in</strong>ancial or proprietary <strong>in</strong>terest <strong>in</strong> any material ormethod mentioned.Correspond<strong>in</strong>g author: Jeewan S<strong>in</strong>gh Titiyal, MD, Pr<strong>of</strong>essor andHead, Cornea, Refractive Surgery and Cataract Services, RajendraPrasad Centre for Ophthalmic Sciences, All India Institute <strong>of</strong>Medical Sciences, Ansari Nagar, New Delhi–110029, India. E-mail:titiyal@rediffmail.com.Table 1. The AC/A ratios before and after LASIK.AC/A Ratio (deg/D)Exam Mean G SD Median M<strong>in</strong>imum MaximumBefore LASIK 3.63 G 1.79 3.93 0.90 6.13Posto<strong>per</strong>ative1 week 4.57 G 1.12 4.80 1.10 6.301 month 6.54 G 1.05 6.60 4.40 11.073 months 4.05 G 1.16 4.30 0.77 5.936 months 4.11 G 1.09 4.30 0.83 5.669 months 4.16 G1.10 4.40 0.77 6.00AC/A Z <strong>accommodative</strong> <strong>convergence</strong> <strong>per</strong> <strong>unit</strong> <strong>of</strong> accommodation;LASIK Z laser <strong>in</strong> situ keratomileusisAccommodative Convergence <strong>per</strong> Unit<strong>of</strong> Accommodation RatioPreo<strong>per</strong>ative The preo<strong>per</strong>ative AC/A ratio was3.637 deg/D (Table 1). There was no significant correlationbetween <strong>the</strong> ratio and refractive error, age, or sex.Posto<strong>per</strong>ative Table 2 shows <strong>the</strong> results <strong>of</strong> <strong>the</strong> between-groupcomparisons. There was a significantdecrease <strong>in</strong> <strong>the</strong> mean AC/A ratio 1 week after LASIK(P Z .001, post hoc Tukey HSD). At 1 month, <strong>the</strong> meanAC/A ratio was still significantly lower than beforeLASIK (P Z .000, post hoc Tukey HSD). At 3 months,<strong>the</strong> mean AC/A ratio was comparable to <strong>the</strong> preo<strong>per</strong>ativevalue (P Z .496, post hoc Tukey HSD). No significantdifference <strong>in</strong> <strong>the</strong> AC/A ratio was seen at 6 or9 months, suggest<strong>in</strong>g stabilization <strong>of</strong> <strong>the</strong> accommodation–<strong>convergence</strong>relationship.As<strong>the</strong>nopic SymptomsOne week after LASIK, 44 patients had at least mildas<strong>the</strong>nopic symptoms. By <strong>the</strong> end <strong>of</strong> 1 month, 27 patientshad symptoms. At <strong>the</strong> 6-month follow-up, 2patients had mild symptoms <strong>of</strong> as<strong>the</strong>nopia; <strong>the</strong> restwere asymptomatic. No patient was symptomatic at9 months. There was a significant reduction <strong>in</strong> <strong>the</strong>number <strong>of</strong> symptomatic patients from <strong>the</strong> first monthonward (chi square Z 89.23; P!.001).DISCUSSIONIn this study, we analyzed <strong>the</strong> change <strong>in</strong> <strong>the</strong> AC/A ratio<strong>in</strong> orthotropic myopic patients who had bilateralLASIK. The assessment <strong>of</strong> this correlation between<strong>the</strong> <strong>accommodative</strong> stimulus and <strong>convergence</strong> is importantbecause LASIK is not just a refractive procedure;it also alters <strong>the</strong> amount <strong>of</strong> <strong>accommodative</strong>response required <strong>in</strong> day-to-day activities comparedto that with spectacle correction. The b<strong>in</strong>ocular <strong>in</strong>teractionrequired for day-to-day activities is differentJ CATARACT REFRACT SURG - VOL 33, DECEMBER 2007