Mims et al, Anti elevation syndrome after anterior transposition of the ...
Mims et al, Anti elevation syndrome after anterior transposition of the ...
Mims et al, Anti elevation syndrome after anterior transposition of the ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
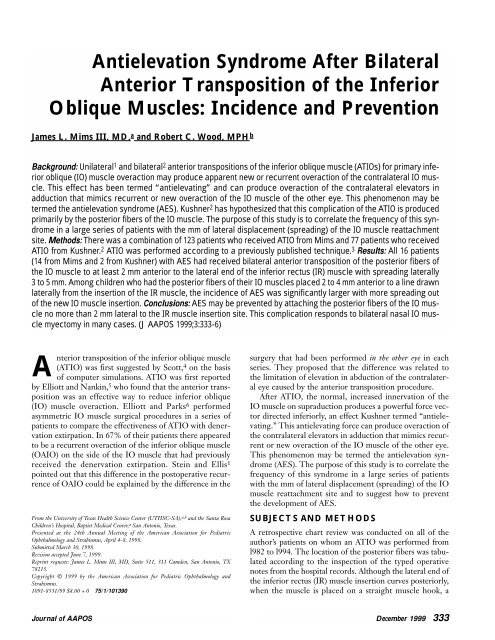
<strong>Anti</strong><strong>elevation</strong> Syndrome After Bilater<strong>al</strong>Anterior Transposition <strong>of</strong> <strong>the</strong> InferiorOblique Muscles: Incidence and PreventionJames L. <strong>Mims</strong> III, MD, a and Robert C. Wood, MPH bBackground: Unilater<strong>al</strong> 1 and bilater<strong>al</strong> 2 <strong>anterior</strong> <strong>transposition</strong>s <strong>of</strong> <strong>the</strong> inferior oblique muscle (ATIOs) for primary inferioroblique (IO) muscle overaction may produce apparent new or recurrent overaction <strong>of</strong> <strong>the</strong> contr<strong>al</strong>ater<strong>al</strong> IO muscle.This effect has been termed “antielevating” and can produce overaction <strong>of</strong> <strong>the</strong> contr<strong>al</strong>ater<strong>al</strong> elevators inadduction that mimics recurrent or new overaction <strong>of</strong> <strong>the</strong> IO muscle <strong>of</strong> <strong>the</strong> o<strong>the</strong>r eye. This phenomenon may b<strong>et</strong>ermed <strong>the</strong> anti<strong>elevation</strong> <strong>syndrome</strong> (AES). Kushner 2 has hypo<strong>the</strong>sized that this complication <strong>of</strong> <strong>the</strong> ATIO is producedprimarily by <strong>the</strong> posterior fibers <strong>of</strong> <strong>the</strong> IO muscle. The purpose <strong>of</strong> this study is to correlate <strong>the</strong> frequency <strong>of</strong> this <strong>syndrome</strong>in a large series <strong>of</strong> patients with <strong>the</strong> mm <strong>of</strong> later<strong>al</strong> displacement (spreading) <strong>of</strong> <strong>the</strong> IO muscle reattachmentsite. M<strong>et</strong>hods: There was a combination <strong>of</strong> 123 patients who received ATIO from <strong>Mims</strong> and 77 patients who receivedATIO from Kushner. 2 ATIO was performed according to a previously published technique. 3 Results: All 16 patients(14 from <strong>Mims</strong> and 2 from Kushner) with AES had received bilater<strong>al</strong> <strong>anterior</strong> <strong>transposition</strong> <strong>of</strong> <strong>the</strong> posterior fibers <strong>of</strong><strong>the</strong> IO muscle to at least 2 mm <strong>anterior</strong> to <strong>the</strong> later<strong>al</strong> end <strong>of</strong> <strong>the</strong> inferior rectus (IR) muscle with spreading later<strong>al</strong>ly3 to 5 mm. Among children who had <strong>the</strong> posterior fibers <strong>of</strong> <strong>the</strong>ir IO muscles placed 2 to 4 mm <strong>anterior</strong> to a line drawnlater<strong>al</strong>ly from <strong>the</strong> insertion <strong>of</strong> <strong>the</strong> IR muscle, <strong>the</strong> incidence <strong>of</strong> AES was significantly larger with more spreading out<strong>of</strong> <strong>the</strong> new IO muscle insertion. Conclusions: AES may be prevented by attaching <strong>the</strong> posterior fibers <strong>of</strong> <strong>the</strong> IO muscleno more than 2 mm later<strong>al</strong> to <strong>the</strong> IR muscle insertion site. This complication responds to bilater<strong>al</strong> nas<strong>al</strong> IO musclemyectomy in many cases. (J AAPOS 1999;3:333-6)Anterior <strong>transposition</strong> <strong>of</strong> <strong>the</strong> inferior oblique muscle(ATIO) was first suggested by Scott, 4 on <strong>the</strong> basis<strong>of</strong> computer simulations. ATIO was first reportedby Elliott and Nankin, 5 who found that <strong>the</strong> <strong>anterior</strong> <strong>transposition</strong>was an effective way to reduce inferior oblique(IO) muscle overaction. Elliott and Parks 6 performedasymm<strong>et</strong>ric IO muscle surgic<strong>al</strong> procedures in a series <strong>of</strong>patients to compare <strong>the</strong> effectiveness <strong>of</strong> ATIO with denervationextirpation. In 67% <strong>of</strong> <strong>the</strong>ir patients <strong>the</strong>re appearedto be a recurrent overaction <strong>of</strong> <strong>the</strong> inferior oblique muscle(OAIO) on <strong>the</strong> side <strong>of</strong> <strong>the</strong> IO muscle that had previouslyreceived <strong>the</strong> denervation extirpation. Stein and Ellis 1pointed out that this difference in <strong>the</strong> postoperative recurrence<strong>of</strong> OAIO could be explained by <strong>the</strong> difference in <strong>the</strong>From <strong>the</strong> University <strong>of</strong> Texas He<strong>al</strong>th Science Center (UTHSC-SA), a,b and <strong>the</strong> Santa RosaChildren’s Hospit<strong>al</strong>, Baptist Medic<strong>al</strong> Center, a San Antonio, Texas.Presented at <strong>the</strong> 24th Annu<strong>al</strong> Me<strong>et</strong>ing <strong>of</strong> <strong>the</strong> American Association for PediatricOphth<strong>al</strong>mology and Strabismus, April 4-8, 1998.Submitted March 30, 1998.Revision accepted June 7, 1999.Reprint requests: James L. <strong>Mims</strong> III, MD, Suite 511, 311 Camden, San Antonio, TX78215.Copyright © 1999 by <strong>the</strong> American Association for Pediatric Ophth<strong>al</strong>mology andStrabismus.1091-8531/99 $8.00 + 0 75/1/101390surgery that had been performed in <strong>the</strong> o<strong>the</strong>r eye in eachseries. They proposed that <strong>the</strong> difference was related to<strong>the</strong> limitation <strong>of</strong> <strong>elevation</strong> in abduction <strong>of</strong> <strong>the</strong> contr<strong>al</strong>ater<strong>al</strong>eye caused by <strong>the</strong> <strong>anterior</strong> <strong>transposition</strong> procedure.After ATIO, <strong>the</strong> norm<strong>al</strong>, increased innervation <strong>of</strong> <strong>the</strong>IO muscle on supraduction produces a powerful force vectordirected inferiorly, an effect Kushner termed “antielevating.”This antielevating force can produce overaction <strong>of</strong><strong>the</strong> contr<strong>al</strong>ater<strong>al</strong> elevators in adduction that mimics recurrentor new overaction <strong>of</strong> <strong>the</strong> IO muscle <strong>of</strong> <strong>the</strong> o<strong>the</strong>r eye.This phenomenon may be termed <strong>the</strong> anti<strong>elevation</strong> <strong>syndrome</strong>(AES). The purpose <strong>of</strong> this study is to correlate <strong>the</strong>frequency <strong>of</strong> this <strong>syndrome</strong> in a large series <strong>of</strong> patientswith <strong>the</strong> mm <strong>of</strong> later<strong>al</strong> displacement (spreading) <strong>of</strong> <strong>the</strong> IOmuscle reattachment site and to suggest how to prevent<strong>the</strong> development <strong>of</strong> AES.SUBJECTS AND METHODSA r<strong>et</strong>rospective chart review was conducted on <strong>al</strong>l <strong>of</strong> <strong>the</strong>author’s patients on whom an ATIO was performed froml982 to l994. The location <strong>of</strong> <strong>the</strong> posterior fibers was tabulatedaccording to <strong>the</strong> inspection <strong>of</strong> <strong>the</strong> typed operativenotes from <strong>the</strong> hospit<strong>al</strong> records. Although <strong>the</strong> later<strong>al</strong> end <strong>of</strong><strong>the</strong> inferior rectus (IR) muscle insertion curves posteriorly,when <strong>the</strong> muscle is placed on a straight muscle hook, aJourn<strong>al</strong> <strong>of</strong> AAPOS December 1999 333
Journ<strong>al</strong> <strong>of</strong> AAPOSVolume 3 Number 6 December 1999<strong>Mims</strong> and Wood 335TABLE 1. AES cases corresponding to each degree <strong>of</strong> <strong>anterior</strong> <strong>transposition</strong> and later<strong>al</strong> displacement <strong>of</strong> <strong>the</strong> IO musclemm tempor<strong>al</strong> to later<strong>al</strong> end <strong>of</strong> IR muscle(X, later<strong>al</strong> displacement) 1 mm 2 mm 3 mm 4 mm 5 mmmm <strong>anterior</strong> to later<strong>al</strong> end <strong>of</strong> IR muscle 4 mm 0/1 0/0 0/6 1/4 1/4(Y, <strong>anterior</strong> <strong>transposition</strong>) 3 mm 0/0 0/1 0/4 1/5 0/32 mm 0/15* 0/1 5/46 3/30 5†/171 mm 0/31* 0/0 0/1 0/1 0/10 mm 0/29*The numerator <strong>of</strong> each fraction is <strong>the</strong> number <strong>of</strong> cases <strong>of</strong> AES; <strong>the</strong> denominator is <strong>the</strong> tot<strong>al</strong> cases with a specific level <strong>of</strong> <strong>anterior</strong> <strong>transposition</strong> (mm <strong>anterior</strong> to a line drawn later<strong>al</strong>lyfrom <strong>the</strong> IR muscle insertion) and later<strong>al</strong> spreading (mm later<strong>al</strong> to <strong>the</strong> later<strong>al</strong> end <strong>of</strong> <strong>the</strong> IR muscle insertion).*All <strong>of</strong> <strong>the</strong>se cases are from Kushner. 2†Two <strong>of</strong> <strong>the</strong>se 5 cases are from Kushner. 2TABLE 2. Various group characteristics among <strong>Mims</strong>’ patients (N = 123)Comparisons <strong>of</strong> those who did and did not have AESMo <strong>of</strong> follow-up* Patient age at MROU (mo) Patient age at ATIO (mo) OAIOAll who did not have AES (N = 109)87.2 ± 4.2 22.4 ± 2.0 35.5 ± 2.3 1.9 ± 0.07All who did have AES (N = 14)45.5 ± 4.3 18.2 ± 3.8 29.4 ± 4.4 2.0 ± 0.14Comparisons among those whose IO muscleswere placed 2 mm or more <strong>anterior</strong> to <strong>al</strong>ine drawn later<strong>al</strong>ly from <strong>the</strong> insertion <strong>of</strong> <strong>the</strong>IR muscle with 3, 4, or 5 mm <strong>of</strong> later<strong>al</strong> displacementMo <strong>of</strong> follow-up* Patient age at MROU (mo) Patient age at ATIO (mo) OAIO3 mm: posterior IO muscle insertion placed at X,Y <strong>of</strong> 3,4 or 3,3 or 3,2. (N = 56)81.8 ± 5.4 24.7 ± 3.1 44.8 ± 5.0 1.8 ± 0.14 mm: posterior IO muscle insertion placed at X,Y <strong>of</strong> 4,4 or 4,3 or 4,2. (N = 39)69.8 ± 6.3 21.7 ± 2.9 31.6 ± 3.7 1.8 ± 0.095 mm: posterior IO muscle insertion placed at X,Y <strong>of</strong> 5,4 or 5,4 or 5,2. (N = 22)97.9 ± 10.8 15.1 ± 3.4 43.2 ± 5.4 2.2 ± 0.16The ± designates ± 1 SE <strong>of</strong> <strong>the</strong> mean.*Months <strong>of</strong> follow-up is <strong>after</strong> <strong>the</strong> ATIO and extends to ei<strong>the</strong>r <strong>the</strong> surgic<strong>al</strong> date for AES or to <strong>the</strong> last visit in <strong>the</strong> <strong>of</strong>fice.MROU, Bilater<strong>al</strong> medi<strong>al</strong> rectus muscle recession.Kushner 2 extended this idea to explain an abnorm<strong>al</strong>motility pattern he observed in some patients <strong>after</strong> bilater<strong>al</strong>ATIO. This pattern resembles marked recurrent OAIOassociated with a Y or V pattern and exotropia in upgaze.Sm<strong>al</strong>l <strong>al</strong>ternating hypertropias (right hypertropia in leftgaze and left hypertropia in right gaze) may be present infar side gazes, but <strong>the</strong>se hypertropias are much sm<strong>al</strong>lerthan those seen in cases <strong>of</strong> primary OAIO with a similarappearance on version testing. A limitation <strong>of</strong> <strong>elevation</strong> <strong>of</strong><strong>the</strong> abducting eye is frequently demonstrable. Kushner 2has hypo<strong>the</strong>sized that this complication <strong>of</strong> ATIO is producedprimarily by <strong>the</strong> posterior fibers <strong>of</strong> <strong>the</strong> IO muscle.In this study, <strong>al</strong>l 16 patients with AES had receivedbilater<strong>al</strong> <strong>anterior</strong> <strong>transposition</strong> <strong>of</strong> <strong>the</strong> posterior fibers <strong>of</strong><strong>the</strong> IO muscle to at least 2 mm <strong>anterior</strong> to <strong>the</strong> later<strong>al</strong> end<strong>of</strong> <strong>the</strong> IR muscle, with displacement 3 to 5 mm later<strong>al</strong> to<strong>the</strong> later<strong>al</strong> end <strong>of</strong> <strong>the</strong> IR muscle insertion. Is <strong>the</strong> incidence<strong>of</strong> AES increased with more later<strong>al</strong> displacement <strong>of</strong> <strong>the</strong>TABLE 3. AES: dependence on amount <strong>of</strong> <strong>anterior</strong> <strong>transposition</strong> and later<strong>al</strong><strong>transposition</strong> (percentages <strong>of</strong> patients with AES <strong>after</strong> ATIO)X (later<strong>al</strong> displacement)Y (<strong>anterior</strong> <strong>transposition</strong>) 0-2 mm 3 mm 4 mm 5 mm0-1 mm 0% 0% 0% 0%2-4 mm 0% 8.9% 12.8% 25%These percentages were derived from <strong>the</strong> data in Table 1.This progression in incidence <strong>of</strong> AES with more spreading out <strong>of</strong> <strong>the</strong> new IO muscleinsertion later<strong>al</strong>ly was significant (P = .011).posterior fibers <strong>of</strong> <strong>the</strong> IO muscle? When we combined ourpatients with those previously reported on by Kushner, 2we found that for those patients with posterior fibers <strong>of</strong> <strong>the</strong>IO muscle placed at least 2 mm directly <strong>anterior</strong> to <strong>the</strong> later<strong>al</strong>end <strong>of</strong> <strong>the</strong> IR muscle, <strong>the</strong> amount <strong>of</strong> later<strong>al</strong> displacement<strong>of</strong> <strong>the</strong> new IO muscle insertion significantly
336 <strong>Mims</strong> and Woodincreased <strong>the</strong> incidence <strong>of</strong> AES (P = .011). A similar an<strong>al</strong>ysisusing only our patients indicated only a trend in thisdirection, not statistic<strong>al</strong> significance (P = .19). There werenot enough patients who were <strong>anterior</strong>ly transposed 0 to 1mm with concurrent displacement 3 to 5 mm later<strong>al</strong>ly tod<strong>et</strong>ermine wh<strong>et</strong>her later<strong>al</strong> displacement was <strong>al</strong>so a hazardwith less <strong>anterior</strong> displacement.For now, it appears that if <strong>the</strong> new insertion <strong>of</strong> <strong>the</strong> IOmuscle is <strong>anterior</strong>ized more than 1 mm (Y >1 mm), <strong>the</strong> newinsertion <strong>of</strong> <strong>the</strong> IO muscle should not be spread out mor<strong>et</strong>han 2 mm, unless <strong>the</strong> severity <strong>of</strong> <strong>the</strong> DVD warrants risk <strong>of</strong>later development <strong>of</strong> AES. The mm <strong>of</strong> <strong>anterior</strong>ization <strong>of</strong><strong>the</strong> IO muscle’s posterior fibers beyond <strong>the</strong> later<strong>al</strong> edge <strong>of</strong><strong>the</strong> IR muscle insertion required to effectively treat variousdegrees <strong>of</strong> DVD severity is not y<strong>et</strong> well characterized. 12-14Also, wh<strong>et</strong>her spreading out <strong>the</strong> muscle less will decreas<strong>et</strong>he effectiveness <strong>of</strong> ATIO in <strong>the</strong> treatment or prevention <strong>of</strong>DVD has not y<strong>et</strong> been studied adequately.Once AES has developed, properly performed bilater<strong>al</strong>nas<strong>al</strong> myectomy is preferable to denervation-extirpationbecause denervation-extirpation can unleash significantDVD. Prevention should be possible because <strong>the</strong> AESappears to be <strong>the</strong> result <strong>of</strong> an excessive downward forcevector <strong>after</strong> ATIO. AES may be prevented by attaching <strong>the</strong>posterior fibers <strong>of</strong> <strong>the</strong> <strong>anterior</strong>ized IO muscle no mor<strong>et</strong>han 2 mm later<strong>al</strong> to <strong>the</strong> IR muscle insertion.Bunching <strong>the</strong> IO muscle insertion at <strong>the</strong> later<strong>al</strong> edge <strong>of</strong><strong>the</strong> IR muscle insertion as described by Kushner 2 shouldbe associated with a very low incidence <strong>of</strong> AES; <strong>the</strong> incidenceand cure <strong>of</strong> DVD were not reported. 2 This studydid not include enough patients with later<strong>al</strong> displacementat <strong>the</strong> exact level <strong>of</strong> <strong>the</strong> IR muscle insertion as described byKratz <strong>et</strong> <strong>al</strong> 12 to predict <strong>the</strong> incidence <strong>of</strong> AES in this technique.Placing <strong>the</strong> new IO muscle insertion 4 to 5 mm justlater<strong>al</strong> to and par<strong>al</strong>lel with <strong>the</strong> <strong>anterior</strong> end <strong>of</strong> <strong>the</strong> IR muscle,as recently described by Guemes and Wright, 15 shouldJourn<strong>al</strong> <strong>of</strong> AAPOSVolume 3 Number 6 December 1999reduce <strong>the</strong> incidence <strong>of</strong> AES, but may reduce <strong>the</strong> control<strong>of</strong> DVD. The technique <strong>of</strong> ATIO as described by <strong>Mims</strong> 3should probably be limited to severe cases <strong>of</strong> DVD.References1.Stein LA, Ellis FJ.Apparent contr<strong>al</strong>ater<strong>al</strong> inferior oblique muscleoveraction <strong>after</strong> unilater<strong>al</strong> inferior oblique weakening procedures. JAAPOS l997;1:2-7.2.Kushner BJ.Restriction <strong>of</strong> <strong>elevation</strong> in abduction <strong>after</strong> inferioroblique <strong>anterior</strong>ization. J AAPOS 1997;1:55-62.3.<strong>Mims</strong> JL, Wood RC.Bilater<strong>al</strong> <strong>anterior</strong> <strong>transposition</strong> <strong>of</strong> <strong>the</strong> inferiorobliques. Arch Ophth<strong>al</strong>mol 1989;107:41-4.4.Scott AB.Planning inferior oblique surgery.In: Reinecke RD, editor.Strabismus. New York: Grune and Stratton; 1978. p. 347-54.5.Elliott RL, Nankin SJ.Anterior <strong>transposition</strong> <strong>of</strong> <strong>the</strong> inferior oblique.J Pediatr Ophth<strong>al</strong>mol Strabismus 1981;18:35-8.6.Elliott RL, Parks MM.A comparison <strong>of</strong> inferior oblique muscleweakening by <strong>anterior</strong> <strong>transposition</strong> or denervation-extirpation.Binocular Vision Eye Muscle Surg Q 1992;7:205-10.7.Weakley DR, Stager DR.Inferior oblique weakening procedures.Ophth<strong>al</strong>mology Clin N Am 1992;5:57-65.8.<strong>Mims</strong> JL.Benefits <strong>of</strong> bilater<strong>al</strong> <strong>anterior</strong> <strong>transposition</strong> <strong>of</strong> <strong>the</strong> inferiorobliques. Arch Ophth<strong>al</strong>mol l986;104:800-1.9.Stager DR, Weakley DR Jr, Stager D.Anterior <strong>transposition</strong> <strong>of</strong> <strong>the</strong>inferior oblique: anatomic assessment <strong>of</strong> <strong>the</strong> neurovascular bundle.Arch Ophth<strong>al</strong>mol 1992;110:360-2.10.Stager DR.The neurovascular bundle <strong>of</strong> <strong>the</strong> inferior oblique muscleas its ancillary origin. Trans Am Ophth<strong>al</strong>mol Soc 1996;94:1073-94.11.Stager DR.The neurovascular bundle <strong>of</strong> <strong>the</strong> inferior oblique muscleas <strong>the</strong> ancillary origin <strong>of</strong> that muscle. J AAPOS l997;1:216-25.12.Kratz RE, Rogers GL, Bremer DL, Lequire LE.Anterior tendondisplacement <strong>of</strong> <strong>the</strong> inferior oblique for DVD. J Pediatr Ophth<strong>al</strong>molStrabismus l989;26:212-7.13.Bac<strong>al</strong> DA, Nelson LB.Anterior <strong>transposition</strong> <strong>of</strong> <strong>the</strong> inferior obliquemuscle for both dissociated vertic<strong>al</strong> deviation and/or inferior obliqueoveraction: results <strong>of</strong> 94 procedures in 55 patients. Binocular VisionEye Muscle Surg Q 1992;17:219-25.14.Ziffer AJ, Isenberg SJ, Elliott RJ, Apt L.The effect <strong>of</strong> <strong>anterior</strong> <strong>transposition</strong><strong>of</strong> <strong>the</strong> inferior oblique muscle. Am J Ophth<strong>al</strong>mol 1993;116:224-7.15.Guemes A, Wright KW.Effect <strong>of</strong> graded <strong>anterior</strong> <strong>transposition</strong> <strong>of</strong><strong>the</strong> inferior oblique muscle on versions and vertic<strong>al</strong> deviation in <strong>the</strong>primary position. J AAPOS 1998;2:201-6.