Change in the accommodative convergence per unit of ...
Change in the accommodative convergence per unit of ...
Change in the accommodative convergence per unit of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
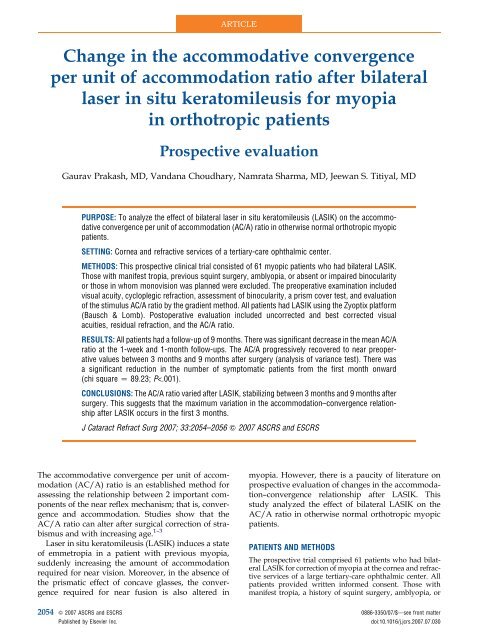
ARTICLE<strong>Change</strong> <strong>in</strong> <strong>the</strong> <strong>accommodative</strong> <strong>convergence</strong><strong>per</strong> <strong>unit</strong> <strong>of</strong> accommodation ratio after bilaterallaser <strong>in</strong> situ keratomileusis for myopia<strong>in</strong> orthotropic patientsProspective evaluationGaurav Prakash, MD, Vandana Choudhary, Namrata Sharma, MD, Jeewan S. Titiyal, MDPURPOSE: To analyze <strong>the</strong> effect <strong>of</strong> bilateral laser <strong>in</strong> situ keratomileusis (LASIK) on <strong>the</strong> <strong>accommodative</strong><strong>convergence</strong> <strong>per</strong> <strong>unit</strong> <strong>of</strong> accommodation (AC/A) ratio <strong>in</strong> o<strong>the</strong>rwise normal orthotropic myopicpatients.SETTING: Cornea and refractive services <strong>of</strong> a tertiary-care ophthalmic center.METHODS: This prospective cl<strong>in</strong>ical trial consisted <strong>of</strong> 61 myopic patients who had bilateral LASIK.Those with manifest tropia, previous squ<strong>in</strong>t surgery, amblyopia, or absent or impaired b<strong>in</strong>ocularityor those <strong>in</strong> whom monovision was planned were excluded. The preo<strong>per</strong>ative exam<strong>in</strong>ation <strong>in</strong>cludedvisual acuity, cycloplegic refraction, assessment <strong>of</strong> b<strong>in</strong>ocularity, a prism cover test, and evaluation<strong>of</strong> <strong>the</strong> stimulus AC/A ratio by <strong>the</strong> gradient method. All patients had LASIK us<strong>in</strong>g <strong>the</strong> Zyoptix platform(Bausch & Lomb). Posto<strong>per</strong>ative evaluation <strong>in</strong>cluded uncorrected and best corrected visualacuities, residual refraction, and <strong>the</strong> AC/A ratio.RESULTS: All patients had a follow-up <strong>of</strong> 9 months. There was significant decrease <strong>in</strong> <strong>the</strong> mean AC/Aratio at <strong>the</strong> 1-week and 1-month follow-ups. The AC/A progressively recovered to near preo<strong>per</strong>ativevalues between 3 months and 9 months after surgery (analysis <strong>of</strong> variance test). There wasa significant reduction <strong>in</strong> <strong>the</strong> number <strong>of</strong> symptomatic patients from <strong>the</strong> first month onward(chi square Z 89.23; P
CHANGE IN AC/A RATIO AFTER BILATERAL LASIK IN ORTHOTROPIA2055absent or impaired b<strong>in</strong>ocular vision and those <strong>in</strong> whichmonovision was planned were not <strong>in</strong>cluded <strong>in</strong> <strong>the</strong> study.The preo<strong>per</strong>ative evaluation <strong>in</strong>cluded Early TreatmentDiabetic Ret<strong>in</strong>opathy Study visual acuity, cycloplegic refractionunder homatrop<strong>in</strong>e 2%, assessment <strong>of</strong> b<strong>in</strong>ocularity us<strong>in</strong>gsynoptophore-based tests, and <strong>the</strong> prism cover test fora 6/6 fixation target. Assessment <strong>of</strong> <strong>the</strong> stimulus AC/A ratiowas <strong>per</strong>formed us<strong>in</strong>g <strong>the</strong> gradient method described by VonNoorden and Campos. 4 All patients had LASIK on <strong>the</strong> Zyoptixplatform us<strong>in</strong>g <strong>the</strong> Technolas IIz system and XP microkeratome(Bausch & Lomb). Both eyes were treated dur<strong>in</strong>g <strong>the</strong>same session.The posto<strong>per</strong>ative assessment <strong>in</strong>cluded uncorrected andbest corrected visual acuities, residual refraction, and <strong>the</strong>AC/A ratio. Symptoms related to as<strong>the</strong>nopia and difficulties<strong>in</strong> near work after LASIK were assessed. As<strong>the</strong>nopia wasassessed us<strong>in</strong>g a questionnaire based on assessment <strong>of</strong>symptoms and <strong>the</strong>ir relative grad<strong>in</strong>g. Occasional difficultyonly after prolonged read<strong>in</strong>g or near work was considereda mild symptom. Symptoms that did not arise dur<strong>in</strong>g dayto day near work but were bo<strong>the</strong>rsome on susta<strong>in</strong>ed <strong>accommodative</strong>or convergent activity (eg, work<strong>in</strong>g on a monitor,read<strong>in</strong>g f<strong>in</strong>e pr<strong>in</strong>t) were considered moderate as<strong>the</strong>nopia.Persistent as<strong>the</strong>nopia requir<strong>in</strong>g cessation <strong>of</strong> all near work relatedactivity was considered a severe symptom. In addition,<strong>the</strong> patient was asked to write down nonspecific symptomsand those not listed on <strong>the</strong> questionnaire. Dry eyes, posto<strong>per</strong>ativeastigmatism, or o<strong>the</strong>r symptoms simulat<strong>in</strong>g as<strong>the</strong>nopiawere ruled out.The data were analyzed us<strong>in</strong>g SPSS s<strong>of</strong>tware (version13.0, SPSS, Inc.). The analysis <strong>of</strong> variance (ANOVA) testwas used to compare <strong>the</strong> change <strong>in</strong> <strong>the</strong> AC/A ratio after surgery.The Tukey honestly significant difference (HSD) testwas used for <strong>in</strong>tergroup comparison. The chi-square testwas used for comparison <strong>of</strong> qualitative data.RESULTSAll patients were followed for 9 months. The mean age<strong>of</strong> <strong>the</strong> 26 men and 35 women was 23.16 years G 2.51(SD) (range 19 to 29 years). The mean spherical equivalent(SE) was 3.69 G 2.52 diopters (D) <strong>in</strong> <strong>the</strong> righteye and 3.93 G 2.32 D <strong>in</strong> <strong>the</strong> left eye. The mean <strong>in</strong>terpupillarydistance was 63.42 G 2.71 mm. The mean residualSE at 9 months was 0.43 G 0.23 D <strong>in</strong> <strong>the</strong> righteye and 0.25 G 0.34 D <strong>in</strong> <strong>the</strong> left eye.Accepted for publication July 26, 2007.From <strong>the</strong> Cornea and Refractive Surgery Services, Rajendra PrasadCentre for Ophthalmic Sciences, All India Institute <strong>of</strong> MedicalSciences, Ansari Nagar, New Delhi, India.No author has a f<strong>in</strong>ancial or proprietary <strong>in</strong>terest <strong>in</strong> any material ormethod mentioned.Correspond<strong>in</strong>g author: Jeewan S<strong>in</strong>gh Titiyal, MD, Pr<strong>of</strong>essor andHead, Cornea, Refractive Surgery and Cataract Services, RajendraPrasad Centre for Ophthalmic Sciences, All India Institute <strong>of</strong>Medical Sciences, Ansari Nagar, New Delhi–110029, India. E-mail:titiyal@rediffmail.com.Table 1. The AC/A ratios before and after LASIK.AC/A Ratio (deg/D)Exam Mean G SD Median M<strong>in</strong>imum MaximumBefore LASIK 3.63 G 1.79 3.93 0.90 6.13Posto<strong>per</strong>ative1 week 4.57 G 1.12 4.80 1.10 6.301 month 6.54 G 1.05 6.60 4.40 11.073 months 4.05 G 1.16 4.30 0.77 5.936 months 4.11 G 1.09 4.30 0.83 5.669 months 4.16 G1.10 4.40 0.77 6.00AC/A Z <strong>accommodative</strong> <strong>convergence</strong> <strong>per</strong> <strong>unit</strong> <strong>of</strong> accommodation;LASIK Z laser <strong>in</strong> situ keratomileusisAccommodative Convergence <strong>per</strong> Unit<strong>of</strong> Accommodation RatioPreo<strong>per</strong>ative The preo<strong>per</strong>ative AC/A ratio was3.637 deg/D (Table 1). There was no significant correlationbetween <strong>the</strong> ratio and refractive error, age, or sex.Posto<strong>per</strong>ative Table 2 shows <strong>the</strong> results <strong>of</strong> <strong>the</strong> between-groupcomparisons. There was a significantdecrease <strong>in</strong> <strong>the</strong> mean AC/A ratio 1 week after LASIK(P Z .001, post hoc Tukey HSD). At 1 month, <strong>the</strong> meanAC/A ratio was still significantly lower than beforeLASIK (P Z .000, post hoc Tukey HSD). At 3 months,<strong>the</strong> mean AC/A ratio was comparable to <strong>the</strong> preo<strong>per</strong>ativevalue (P Z .496, post hoc Tukey HSD). No significantdifference <strong>in</strong> <strong>the</strong> AC/A ratio was seen at 6 or9 months, suggest<strong>in</strong>g stabilization <strong>of</strong> <strong>the</strong> accommodation–<strong>convergence</strong>relationship.As<strong>the</strong>nopic SymptomsOne week after LASIK, 44 patients had at least mildas<strong>the</strong>nopic symptoms. By <strong>the</strong> end <strong>of</strong> 1 month, 27 patientshad symptoms. At <strong>the</strong> 6-month follow-up, 2patients had mild symptoms <strong>of</strong> as<strong>the</strong>nopia; <strong>the</strong> restwere asymptomatic. No patient was symptomatic at9 months. There was a significant reduction <strong>in</strong> <strong>the</strong>number <strong>of</strong> symptomatic patients from <strong>the</strong> first monthonward (chi square Z 89.23; P!.001).DISCUSSIONIn this study, we analyzed <strong>the</strong> change <strong>in</strong> <strong>the</strong> AC/A ratio<strong>in</strong> orthotropic myopic patients who had bilateralLASIK. The assessment <strong>of</strong> this correlation between<strong>the</strong> <strong>accommodative</strong> stimulus and <strong>convergence</strong> is importantbecause LASIK is not just a refractive procedure;it also alters <strong>the</strong> amount <strong>of</strong> <strong>accommodative</strong>response required <strong>in</strong> day-to-day activities comparedto that with spectacle correction. The b<strong>in</strong>ocular <strong>in</strong>teractionrequired for day-to-day activities is differentJ CATARACT REFRACT SURG - VOL 33, DECEMBER 2007
2056 CHANGE IN AC/A RATIO AFTER BILATERAL LASIK IN ORTHOTROPIATable 2. Results <strong>of</strong> between-group comparisons.*Post Hoc TestPre LASIK vs1 weekPre LASIK vs1 monthPre LASIK vs3 monthsPre LASIK vs6 monthsPre LASIK vs9 monthsDifference<strong>of</strong> MeanConfidence IntervalP Value(Tukey HSD) Lower Up<strong>per</strong>0.94 .000 1.60 0.272.9 .000 3.57 2.240.42 .49 1.08 0.240.48 .33 1.14 0.180.52 .22 1.18 0.13HSD Z honestly significant difference; LASIK Z laser <strong>in</strong> situkeratomileusis*Between-group ANOVA comparison, P Z .000between myopic patients and emmetropic patients.Because <strong>the</strong> far po<strong>in</strong>t <strong>in</strong> myopia is between <strong>in</strong>f<strong>in</strong>ityand <strong>the</strong> near po<strong>in</strong>t, <strong>the</strong> <strong>accommodative</strong> effort requiredfor near vision is lower than <strong>in</strong> emmetropia, <strong>in</strong> which<strong>the</strong> far po<strong>in</strong>t is at <strong>in</strong>f<strong>in</strong>ity. However, when myopia iscorrected by a refractive procedure, <strong>the</strong> accommodation–<strong>convergence</strong>relationship should follow <strong>the</strong> patterns<strong>of</strong> emmetropia. This study questioned whe<strong>the</strong>r<strong>the</strong> above hypo<strong>the</strong>sis is true and if so, what <strong>the</strong> expectedtime frame is for <strong>the</strong>se adjustments <strong>in</strong> <strong>the</strong> accommodation–<strong>convergence</strong>arc.We found an <strong>in</strong>itial decrease <strong>in</strong> <strong>the</strong> AC/A ratio <strong>in</strong><strong>the</strong> early posto<strong>per</strong>ative <strong>per</strong>iod. The probable reasonis an <strong>in</strong>creased <strong>accommodative</strong> effort to produce <strong>the</strong>same amount <strong>of</strong> <strong>convergence</strong> <strong>in</strong> <strong>the</strong> newly <strong>in</strong>ducedemmetropic state.The <strong>in</strong>creased AC/A ratio 1 month after surgeryprovides fur<strong>the</strong>r evidence <strong>of</strong> <strong>the</strong> unstable accommodation–<strong>convergence</strong>relationship. As <strong>the</strong> quality <strong>of</strong> accommodationeffort improves with adjustment to <strong>the</strong>new emmetropic state, <strong>the</strong> amount <strong>of</strong> <strong>convergence</strong>produced <strong>per</strong> <strong>unit</strong> <strong>of</strong> accommodation probably <strong>in</strong>creases.This could have resulted <strong>in</strong> <strong>the</strong> higher AC/Aratio at 1 month. With time, <strong>the</strong> AC/A ratio progressivelydecreased to stabilize between 3 months and6 months after surgery. This suggests that <strong>the</strong> maximumvariation <strong>in</strong> <strong>the</strong> accommodation–<strong>convergence</strong>relationship after LASIK occurs with<strong>in</strong> <strong>the</strong> first3 months.Earlier studies 5,6 show that <strong>the</strong> AC/A ratios <strong>in</strong> emmetropicpatients are lower than those <strong>in</strong> myopicpatients. Therefore, it can be concluded that <strong>the</strong> emmetropiacreated by LASIK tends to simulate <strong>the</strong> accommodation–<strong>convergence</strong>relationship <strong>in</strong> naturallyemmetropic eyes. A change <strong>in</strong> <strong>the</strong> AC/A ratio can predictmyopia. 7 It rema<strong>in</strong>s to be seen whe<strong>the</strong>r regressionafter LASIK for myopia follows a similar pattern.In conclusion, our study evaluated <strong>the</strong> changes <strong>in</strong><strong>the</strong> accommodation–<strong>convergence</strong> relationship afterLASIK. We found <strong>the</strong> AC/A ratio gradually returnedto near preo<strong>per</strong>ative values. This could expla<strong>in</strong> some<strong>of</strong> <strong>the</strong> posto<strong>per</strong>ative symptoms <strong>in</strong> <strong>the</strong> absence <strong>of</strong> grossastigmatism, flap, and ocular surface complications.This study provides evidence <strong>of</strong> a transient change <strong>in</strong><strong>the</strong> AC/A ratio after LASIK surgery, most <strong>of</strong> which occurs<strong>in</strong> <strong>the</strong> <strong>in</strong>itial months, and that <strong>the</strong> ratio stabilizesby 3 to 6 months. Larger studies are required to assess<strong>the</strong> changes <strong>in</strong> <strong>the</strong> AC/A ratio <strong>in</strong> patients with regressionafter LASIK. It would also be worthwhile to evaluatewhe<strong>the</strong>r <strong>the</strong> results are different after surfaceablation procedures, <strong>in</strong> which wound-heal<strong>in</strong>g patternsare different and epi<strong>the</strong>lial haze (and thus blurr<strong>in</strong>g andmore <strong>accommodative</strong> stimulus) can occur, andwhe<strong>the</strong>r spar<strong>in</strong>g <strong>the</strong> corneal nerves causes a differentAC/A ratio response.REFERENCES1. Semmlow J, Putteman A, Vercher J-L, et al. Surgical modification<strong>of</strong> <strong>the</strong> AC/A ratio and <strong>the</strong> b<strong>in</strong>ocular alignment (‘‘phoria’’) at distance;its <strong>in</strong>fluence on <strong>accommodative</strong> esotropia: a study <strong>of</strong> 21cases. B<strong>in</strong>ocul Vis Strabismus Q 2000; 15:121–1302. Lucas E, Bentley CR, Aclimandos WA. The effect <strong>of</strong> surgery on<strong>the</strong> AC/A ratio. Eye 1994; 8:109–1143. Ciuffreda KJ, Rosenfield M, Chen H-W. The AC/A ratio, age andpresbyopia. Ophthalmic Physiol Opt 1997; 17:307–3154. Von Noorden GK, Campos EC, eds. B<strong>in</strong>ocular Vision and OcularMotility; Theory and Management <strong>of</strong> Strabismus, 6th ed. St Louis,MO, Mosby, 2002; 91–925. Rosenfield M, Gilmart<strong>in</strong> B. Effect <strong>of</strong> a near-vision task on <strong>the</strong>response AC/A <strong>of</strong> a myopic population. Ophthalmic Physiol Opt1987; 7:225–2336. Gwiazda J, Grice K, Thorn F. Response AC/A ratios are elevated<strong>in</strong> myopic children. Ophthalmic Physiol Opt 1999; 19:173–1797. Gwiazda J, Thorn F, Held R. Accommodation, <strong>accommodative</strong><strong>convergence</strong>, and response AC/A ratios before and at <strong>the</strong> onset<strong>of</strong> myopia <strong>in</strong> children. Optom Vis Sci 2005; 82:273–278First author:Gaurav Prakash, MDCornea and Refractive Surgery Services,Rajendra Prasad Centre for OphthalmicSciences, All India Institute <strong>of</strong> MedicalSciences, New Delhi, IndiaJ CATARACT REFRACT SURG - VOL 33, DECEMBER 2007