Trauma Guideline Manual - SUNY Upstate Medical University
Trauma Guideline Manual - SUNY Upstate Medical University
Trauma Guideline Manual - SUNY Upstate Medical University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
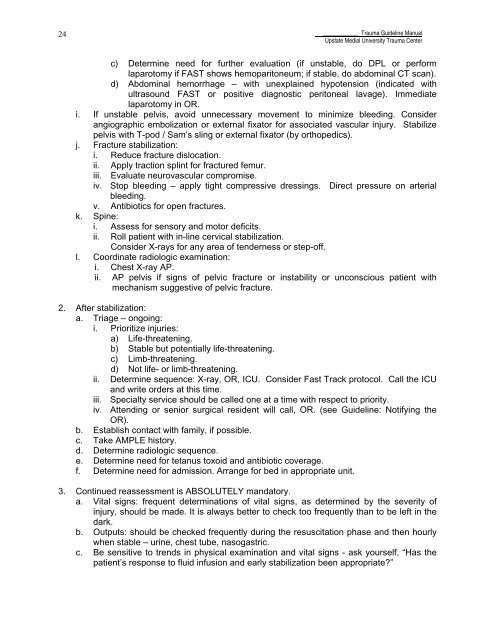
24____________ <strong>Trauma</strong> <strong>Guideline</strong> <strong>Manual</strong><strong>Upstate</strong> Medial <strong>University</strong> <strong>Trauma</strong> Centerc) Determine need for further evaluation (if unstable, do DPL or performlaparotomy if FAST shows hemoparitoneum; if stable, do abdominal CT scan).d) Abdominal hemorrhage – with unexplained hypotension (indicated withultrasound FAST or positive diagnostic peritoneal lavage). Immediatelaparotomy in OR.i. If unstable pelvis, avoid unnecessary movement to minimize bleeding. Considerangiographic embolization or external fixator for associated vascular injury. Stabilizepelvis with T-pod / Sam’s sling or external fixator (by orthopedics).j. Fracture stabilization:i. Reduce fracture dislocation.ii. Apply traction splint for fractured femur.iii. Evaluate neurovascular compromise.iv. Stop bleeding – apply tight compressive dressings. Direct pressure on arterialbleeding.v. Antibiotics for open fractures.k. Spine:i. Assess for sensory and motor deficits.ii. Roll patient with in-line cervical stabilization.Consider X-rays for any area of tenderness or step-off.l. Coordinate radiologic examination:i. Chest X-ray AP.ii.AP pelvis if signs of pelvic fracture or instability or unconscious patient withmechanism suggestive of pelvic fracture.2. After stabilization:a. Triage – ongoing:i. Prioritize injuries:a) Life-threatening.b) Stable but potentially life-threatening.c) Limb-threatening.d) Not life- or limb-threatening.ii.Determine sequence: X-ray, OR, ICU. Consider Fast Track protocol. Call the ICUand write orders at this time.iii. Specialty service should be called one at a time with respect to priority.iv. Attending or senior surgical resident will call, OR. (see <strong>Guideline</strong>: Notifying theOR).b. Establish contact with family, if possible.c. Take AMPLE history.d. Determine radiologic sequence.e. Determine need for tetanus toxoid and antibiotic coverage.f. Determine need for admission. Arrange for bed in appropriate unit.3. Continued reassessment is ABSOLUTELY mandatory.a. Vital signs: frequent determinations of vital signs, as determined by the severity ofinjury, should be made. It is always better to check too frequently than to be left in thedark.b. Outputs: should be checked frequently during the resuscitation phase and then hourlywhen stable – urine, chest tube, nasogastric.c. Be sensitive to trends in physical examination and vital signs - ask yourself, “Has thepatient’s response to fluid infusion and early stabilization been appropriate?”