A study of the pathology and pathogenesis of bronchiectasis.
A study of the pathology and pathogenesis of bronchiectasis.
A study of the pathology and pathogenesis of bronchiectasis.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
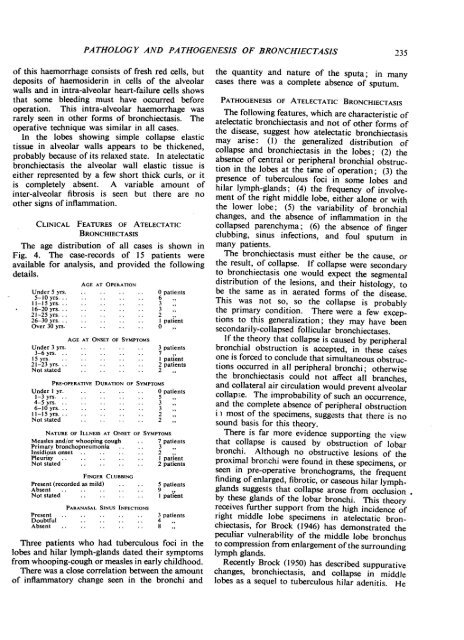
PATHOLOGY AND PA THOGENESIS OF BRONCHIECTASIS<strong>of</strong> this haemorrhage consists <strong>of</strong> fresh red cells, but(leposits <strong>of</strong> haemosiderin in cells <strong>of</strong> <strong>the</strong> alveolarwalls <strong>and</strong> in intra-alveolar heart-failure cells showsthat some bleeding must have occurred beforeoperation. This intra-alveolar haemorrhage wasrarely seen in o<strong>the</strong>r forms <strong>of</strong> <strong>bronchiectasis</strong>. Theoperative technique was similar in all cases.In <strong>the</strong> lobes showing simple collapse elastictissue in alveolar walls appears to be thickened,probably because <strong>of</strong> its relaxed state. In atelectatic<strong>bronchiectasis</strong> <strong>the</strong> alveolar wall elastic tissue isei<strong>the</strong>r represented by a few short thick curls, or itis completely absent. A variable amount <strong>of</strong>inter-alveolar fibrosis is seen but <strong>the</strong>re are noo<strong>the</strong>r signs <strong>of</strong> inflammation.CLINICAL FEATURES OF ATELECTATICBRONCHIECTASISThe age distribution <strong>of</strong> all cases is shown inFig. 4. The case-records <strong>of</strong> 15 patients wereavailable for analysis, <strong>and</strong> provided <strong>the</strong> followingdetails.AGE AT OPERATIONUnder 5 yrs.5-10 yrs.11-1 5 yrs.16-20yrs.21-25yrs.26-30yrs.Over 30 yrs.AGE AT ONSET OF SYMPTOMSUnder 3 yrs.3-6yrs.15yrs.21-23yrs.Not stated0 patients6 332 -I patient0 ,3 patients7I patientpatients2PRE-OPERATIVE DURATION OF SYMPTOMSUnder I yr. 0 patients1-3 yrs. 54-5 yrs. 36-10 yrs. 3II-I 5 yrs. 2Not stated 2NATURE OF ILLNESS AT ONSET OF SYMPTOMSMeasles <strong>and</strong>/or whooping cough7 patientsPrimary bronchopneumonia 3Insidious onset .. 2Pleurisy .. I patientNotstated.2 patientsFINGER CLUBBINGPresent (recorded as mild)Absent . .Not statedPresentDoubtfulAbsentPARANASAL SINUS INFECTIONS5 patients9 .,I patient3 patients48Three patients who had tuberculous foci in <strong>the</strong>lobes <strong>and</strong> hilar lymph-gl<strong>and</strong>s dated <strong>the</strong>ir symptomsfrom whooping-cough or measles in early childhood.There was a close correlation between <strong>the</strong> amount<strong>of</strong> inflammatory change seen in <strong>the</strong> bronchi <strong>and</strong>235<strong>the</strong> quantity <strong>and</strong> nature <strong>of</strong> <strong>the</strong> sputa; in manycases <strong>the</strong>re was a complete absence <strong>of</strong> sputum.PATHOGENESIS OF ATELECTATIC BRONCHIECTASISThe following features, which are characteristic <strong>of</strong>atelectatic <strong>bronchiectasis</strong> <strong>and</strong> not <strong>of</strong> o<strong>the</strong>r forms <strong>of</strong><strong>the</strong> disease, suggest how atelectatic <strong>bronchiectasis</strong>may arise: (1) <strong>the</strong> generalized distribution <strong>of</strong>collapse <strong>and</strong> <strong>bronchiectasis</strong> in <strong>the</strong> lobes; (2) <strong>the</strong>absence <strong>of</strong> central or peripheral bronchial obstructionin <strong>the</strong> lobes at <strong>the</strong> time <strong>of</strong> operation; (3) <strong>the</strong>presence <strong>of</strong> tuberculous foci in some lobes <strong>and</strong>hilar lymph-gl<strong>and</strong>s; (4) <strong>the</strong> frequency <strong>of</strong> involvement<strong>of</strong> <strong>the</strong> right middle lobe, ei<strong>the</strong>r alone or with<strong>the</strong> lower lobe; (5) <strong>the</strong> variability <strong>of</strong> bronchialchanges, <strong>and</strong> <strong>the</strong> absence <strong>of</strong> inflammation in <strong>the</strong>collapsed parenchyma; (6) <strong>the</strong> absence <strong>of</strong> fingerclubbing, sinus infections, <strong>and</strong> foul sputum inmany patients.The <strong>bronchiectasis</strong> must ei<strong>the</strong>r be <strong>the</strong> cause, or<strong>the</strong> result, <strong>of</strong> collapse. If collapse were secondaryto <strong>bronchiectasis</strong> one would expect <strong>the</strong> segmentaldistribution <strong>of</strong> <strong>the</strong> lesions, <strong>and</strong> <strong>the</strong>ir histology, tobe <strong>the</strong> same as in aerated forms <strong>of</strong> <strong>the</strong> disease.This was not so, so <strong>the</strong> collapse is probably<strong>the</strong> primary condition. There were a few exceptionsto this generalization; <strong>the</strong>y may have beensecondarily-collapsed follicular bronchiectases.If <strong>the</strong> <strong>the</strong>ory that collapse is caused by peripheralbronchial obstruction is accepted, in <strong>the</strong>se casesone is forced to conclude that simultaneous obstructionsoccurred in all peripheral bronchi; o<strong>the</strong>rwise<strong>the</strong> <strong>bronchiectasis</strong> could not affect all branches,<strong>and</strong> collateral air circulation would prevent alveolarcollapse. The improbability <strong>of</strong> such an occurrence,<strong>and</strong> <strong>the</strong> complete absence <strong>of</strong> peripheral obstructioni most <strong>of</strong> <strong>the</strong> specimens, suggests that <strong>the</strong>re is nosound basis for this <strong>the</strong>ory.There is far more evidence supporting <strong>the</strong> viewthat collapse is caused by obstruction <strong>of</strong> lobarbronchi. Although no obstructive lesions <strong>of</strong> <strong>the</strong>proximal bronchi were found in <strong>the</strong>se specimens, orseen in pre-operative bronchograms, <strong>the</strong> frequentfinding <strong>of</strong> enlarged, fibrotic, or caseous hilar lymphgl<strong>and</strong>ssuggests that collapse arose from occlusionby <strong>the</strong>se gl<strong>and</strong>s <strong>of</strong> <strong>the</strong> lobar bronchi. This <strong>the</strong>oryreceives fur<strong>the</strong>r support from <strong>the</strong> high incidence <strong>of</strong>right middle lobe specimens in atelectatic <strong>bronchiectasis</strong>,for Brock (1946) has demonstrated <strong>the</strong>peculiar vulnerability <strong>of</strong> <strong>the</strong> middle lobe bronchusto compression from enlargement <strong>of</strong> <strong>the</strong> surroundinglymph gl<strong>and</strong>s.Recently Brock (1950) has described suppurativechanges, <strong>bronchiectasis</strong>, <strong>and</strong> collapse in middlelobes as a sequel to tuberculous hilar adenitis. He