Intraoperative Cardiopulmonary Bypass Heparin ... - Casecag.com
Intraoperative Cardiopulmonary Bypass Heparin ... - Casecag.com
Intraoperative Cardiopulmonary Bypass Heparin ... - Casecag.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
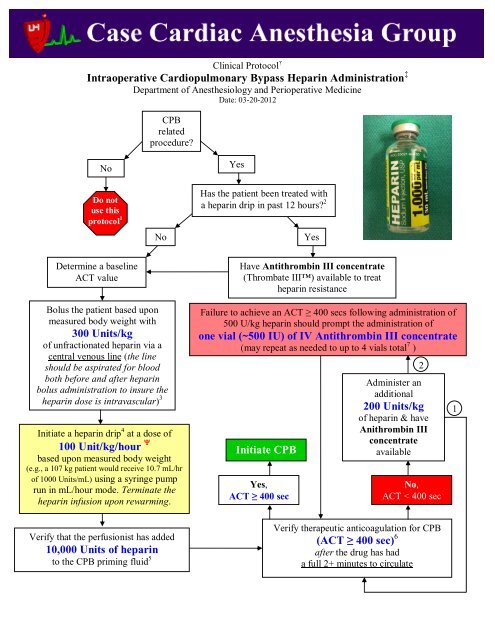
Clinical Protocol †<strong>Intraoperative</strong> <strong>Cardiopulmonary</strong> <strong>Bypass</strong> <strong>Heparin</strong> Administration ‡Department of Anesthesiology and Perioperative MedicineDate: 03-20-2012CPBrelatedprocedure?NoDo notuse thisprotocol 1NoYesHas the patient been treated witha heparin drip in past 12 hours? 2YesDetermine a baselineACT valueHave Antithrombin III concentrate(Thrombate III) available to treatheparin resistanceBolus the patient based uponmeasured body weight with300 Units/kgof unfractionated heparin via acentral venous line (the lineshould be aspirated for bloodboth before and after heparinbolus administration to insure theheparin dose is intravascular) 3Initiate a heparin drip 4 at a dose of100 Unit/kg/hour based upon measured body weight(e.g., a 107 kg patient would receive 10.7 mL/hrof 1000 Units/mL) using a syringe pumprun in mL/hour mode. Terminate theheparin infusion upon rewarming.Verify that the perfusionist has added10,000 Units of heparinto the CPB priming fluid 5Failure to achieve an ACT ≥ 400 secs following administration of500 U/kg heparin should prompt the administration ofone vial (~500 IU) of IV Antithrombin III concentrate(may repeat as needed to up to 4 vials total 7 )Initiate CPBYes,ACT ≥ 400 secNo,ACT < 400 secVerify therapeutic anticoagulation for CPB(ACT ≥ 400 sec) 6after the drug has hada full 2+ minutes to circulate2Administer anadditional200 Units/kgof heparin & haveAnithrombin IIIconcentrateavailable1
†Clinical protocols are based on the best and most recent available data and are expected to be followed by allCASECAG staff unless there is a <strong>com</strong>pelling clinical reason not to, or new data be<strong>com</strong>es available that suggestsan alternate treatment protocol. Standardizing our approach to some of our practices is expected to reduce drugerrors in the clinical environment and improve ease of work flow for the trainees.‡<strong>Heparin</strong> administration protocols vary by institution. This protocol is based upon established practice patternsat UHCMC as well as a review of the peer reviewed literature related to this topic.1: This protocol is intended for use in patients undergoing procedures requiring the use of cardiopulmonarybypass (CPB). Employing this protocol in other patient populations may result in life threatening hemorrhagic<strong>com</strong>plications.2: There are several clinical scenarios where heparin resistance (or insensitivity) has been observed to be more<strong>com</strong>mon. (Avery EG, et al.). The following list of clinical scenarios should prompt one to be ready to treatheparin resistance:Treatment with heparin infusion in the preceding 12 hoursTreatment with an intra-aortic balloon pump (IABP) ± heparin infusionTreatment with a nitroglycerin infusionKnown antithrombin III deficiencyDisseminated intravascular coagulation (DIC)Active endocarditis or sepsis3: Failure to aspirate the central line both prior to and following IV heparin administration could result in afailure to adequately heparinize the patient as central line migration cannot be ruled out. Any question about thefunctional status of the central line and administration of the heparin can be verified with the activated clottingtime (ACT). If the central line has migrated then the heparin should be administered directly into the rightatrium by the surgeon followed by ACT verification. (Mashour G, Avery EG)4: Use of heparin infusions have been demonstrated in prospective studies to be associated with achievement ofmore consistent blood heparin levels as well as less postoperative hemorrhage. (Despotis GJ, et al.) Further, useof heparin infusions in the setting of cardiac surgery has been associated with biochemical evidence of bettercoagulation cascade suppression. (Despotis GJ, et al.): The use of an infusion is optional but is well supported by the literature. In the absence of an infusion theperfusionists will administer additional heparin based upon the measured ACT on bypass which was formerlydemonstrated to have a poor correlation with measured heparin concentrations (likely due to the hypothermiaand hemodilution that frequently ac<strong>com</strong>panies extracorporeal circulation). A more sound strategy would be toadminister 100 U/kg of heparin as an IV bolus every hour of bypass following the initial loading dose of 300U/kg until bypass is terminated.5: The perfusionists are all careful not to add the heparin (and amicar when applicable) to the CPB pump primeuntil after they have <strong>com</strong>pleted the retrograde autologous priming procedure so that the drugs are not lost in thediscarded prime fluids.6: The established threshold of an ACT ≥ 400 sec with the Hemochron Jr. Elite is equivalent to an ACT of 480sec obtained with the Hemochron 801 per an internal validation/<strong>com</strong>parison study. The ACT value of ≥ 400 secwill continue to be acceptable at our institution until prospective study of this value in our unique clinicalsetting demonstrates either biochemical or transfusion out<strong>com</strong>e evidence of a detrimental out<strong>com</strong>e associatedwith employing this threshold. Peak heparin effect has been shown to occur at 2 minutes after IV bolus injectionin cardiac surgical patients. Waiting longer to check an ACT in patient with low cardiac output syndrome isonly a theoretical concern that has never been validated.
7: Doses as high as 50 IU/kg (e.g., approximately 7 vials in a 70 kg patient)of antithrombin III concentrate have been tested in cardiac surgical patientsand found to be safe and effective. It has not been shown that there is anyclear benefit in using such high doses so it appears to be both medically safeand pharmacoeconomically prudent not to use any more than is necessary toachieve our desired ACT threshold of ≥ 400 sec. (Koster A, et al.)References:Avery EG, Willsey D, Chang Y, Grecu L, D’Ambra M. Predictors of <strong>Heparin</strong> Resistance: The Importance ofRefining <strong>Heparin</strong> Dosing Guidelines in Cardiac Surgical Patients. Anesthesia and Analgesia 2001: 92(4S):SCA105.Mashour G, Avery EG. Anesthesia for Cardiac Surgery. Hurford WE, Bailin MT, Davison JK, Haspel KL,Rosow CE, Vassalo SE. Clinical Anesthesia Procedures of the Massachusetts General Hospital 6 th ed.Lippincott, Williams and Wilkins. Philadelphia, PA. 2007;p. 401-40.Despotis GJ, Levine J, Joiner-Maier D, et al. A Comparison Between Continuous Infusion and Standard BolusAdministration of <strong>Heparin</strong> Based On Monitoring in Cardiac Surgery. Blood Coagul Fibrinolysis 1997;8(7):419-30.Despotis GJ, Joist JH, Hogue CW, et al. The Impact of <strong>Heparin</strong> Concentration and Activated Clotting TimeMonitoring on Blood Conservation: A Prospective, Randomized Evaluation in Patients Undergoing CardiacOperation. J Thorac Cardiovasc Surg 1995;110:46-54.Koster A, Fischer T, Greundel M, et al. Management of <strong>Heparin</strong> Resistance During <strong>Cardiopulmonary</strong> <strong>Bypass</strong>:The Effects of Five Different Anticoagulation Strategies on Hemostatic Activation. J Cardiothorac VascAnesth 2003;17(2):171-75.