Monitoring Regional Oxygen Saturation - Casecag.com
Monitoring Regional Oxygen Saturation - Casecag.com
Monitoring Regional Oxygen Saturation - Casecag.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Faculty DisclosureUnless cited, the contents and conclusions of the followingpresentation are solely those of the presenter:• Edwin G. Avery, IV, MD, CPI• Chief, Division of Cardiac Anesthesia• University Hospitals Case Medical Center
Disclosures:Covidien: consultant, speaker’s bureauAlere: funded researchThe Medicines Company: funded research
Disclosure StatementThe speaker received funding from Nellcor Puritan Bennett LLCdba “Covidien” for this speaking engagement. To the extent thispresentation material contains images of patients or any materialwhere a copyright is held by a third party, all necessary writtenpermissions from the patient or copyright holder, as applicable,with respect to use, distribution or copying of such images orcopyrighted materials has been obtained.
ClickHerewww.casecag.<strong>com</strong>
OverviewPostoperative morbidity andmortalityGeneral concepts: Near-InfraRedSpectroscopy (NIRS) and regionalcerebral oxygenation (rSO 2 )Validation workClinical studies and illustrative casesExpanded clinical use of rSO 2A-Star Research
Surgery Related Morbidity and Mortalitymedschool.lsuhsc.edu
Projected US Population Growth by Age:2010-2050US Census Bureau, Statistical Abstract of the US 2012 (www.census.gov)Population in Millions20015065> 75> 85>140 million10065 million5002010 2015 2020 2025 2030 2035 2040 2045 2050Age is a well known risk factor for postoperative mortality and cognitivedysfunction and is associated with 1 year survival rates.
Determinants of Long-Term Survival After MajorSurgery and the Adverse Effect ofPostoperative Complications• 105,951 patients• 69% decrease inmedian survival ratefor 30 day<strong>com</strong>plication“The occurrence of a 30day postoperative<strong>com</strong>plication is moreimportant thanpreoperative patient riskand intraoperative factorsin determining survivalafter major surgery”Survival ProbabilityAll PatientsPatients surviving beyond30 days postopDays= Patients with no <strong>com</strong>plications= Patients with 1 or more <strong>com</strong>plicationsKhuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effects ofpostoperative <strong>com</strong>plications. Annals of Surgery. 2005; 242(3): 326-343.
Postoperative Delirium• Delirium is a <strong>com</strong>mon <strong>com</strong>plication afflicting postsurgicalgeriatric patients.– Hyperactive, hypoactive and mixed• Mortality is higher in those who experience post-op delirium• In 2004 alone, treatment of delirium cost Medicare $6.9 billion.• The type of surgery affects the delirium rates– After orthopedic procedures, a range of 16%-62% after femoral neckfracture repairs– After cardiac surgery, a range of 8.4% - 41.7%– After vascular surgery, a range of 29.1% - 42.3%– After general surgery, ~7% but estimates increase to 26% after majorabdominal surgery
General Concepts: Near-Infrared Spectroscopybased Cerebral Oximetry
NIRS Measures Hemoglobin in Microcirculation (vessels < 100 μm)<strong>Regional</strong> O 2 saturation (rSO 2 ):1. Provides a unique venousweighted measure of O 2 balanceat the gas exchange site2. Reflects real-time changes inregional tissueperfusion adequacy3. May precede changes insystemic parametersMicrocirculation ( vessels < 100μm) contains half of the body’sblood volume.rSO 225% arterial75% venousTobias JD. Cerebral Oximetry <strong>Monitoring</strong> with Near Infrared Spectroscopy DetectsAlterations in <strong>Oxygen</strong>ation Before Pulse Oximetry. J Intensive Care Med. 2008; 23:384-388
Cerebral rSO 2Despite the relatively small volume of tissue being interrogated byNIRS cerebral oximetry (i.e. ~15 mm 3 ) it may serve as an indexorgan reflecting the adequacy of tissue oxygenation throughout theentire body.< 100 microns (0.1 mm) indiameter2010 Avery EG, White paper
NIRS Readings“Banana arc”Arc sensor(distaldetector)Arc sensor(proximaldetector)Light emitting diode (LED)AdhesivepadHongo K, Kobayashi S, Okudera H, Hokama M, Nakagawa F. Noninvasive Cerebral Optical Spectroscopy: Depth-resolvedMeasurements of Cerebral Haemodynamics Using Indocyanine Green. Neurol Res 1995;17: 89-93
General Concepts – rSO 2Sensor PADReceptorsPredictable pathBanana arcSpatiallyresolvedLED
Available devicesThere are currently five FDA cleared devices ‡ that are marketedto assess cerebral oxygenation which include:2λSomanetics INVOSCASMED – Fore-sight4λ(~20 years of clinical use)Ornim – Cerox 3,4λNonin – Equanox4λ(2 models)‡Devices listed in order of FDA clearance2010 Avery EG, White paper.Gagnon RE, Macnab AJ, Gagnon FA, et al. Comparison of Two Spatially Resolved NIRS <strong>Oxygen</strong>ation Indices. J Clin Monit2002;17:385-91
INVOS Indications for UseThe noninvasive INVOS 5100C is intended for use as an adjunctmonitor of regional hemoglobin oxygen saturation of blood in thebrain or in other tissue beneath the sensor. It is intended for use inindividuals greater than 2.5 kg at risk for reduced-flow or non-flowischemic states. It is also intended for use as an adjunct trendmonitor of regional hemoglobin saturation in the brain or in othertissues beneath the sensor in any individual.
NIRS rSO 2 Validation Studies
Validation – No Gold StandardThe validation of rSO 2 monitoring is challenged by the fact thatthere is no gold standard, or index test, invasive or non-invasiveof cerebral oxygenation.2010 Avery EG, White paper
Validation: rSO 2 Assesses Cortical TissueICG ICA injectionICG ECA injection†Hongo K, Kobayashi S, Okudera H, Hokama M, Nakagawa F. Noninvasive Cerebral Optical Spectroscopy: Depth-resolvedMeasurements of Cerebral Haemodynamics Using Indocyanine Green. Neurol Res 1995;17: 89-93
Validation: Intra-Cranial Sensitivity†• Balloon test occlusion w/ SPECT +cerebral oximeter + stump pressure• Desaturation >8% = low flow +ischemic symptomsKaminogo M, Ochi M, Onizuka M, Takahata H, Shibata S. An Additional <strong>Monitoring</strong> of Regaionl Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> toHMPAO SPECT Study During Balloon Test Occlusion. Stroke. 1999; 30:407-413†rSO 2 data on file at Covidien, Boulder, CO.
Relevant Comparative Variables:SaO 2 , SpO 2 , TiPO 2 , SvO 2 , SjvO 2 vs. rSO 2SaO 2 - Systemic arterial oxygen availabilitySpO 2 - Depends on pulsatile blood flow and measures only theoxy-Hb in arterial blood as it leaves the heartTiPO 2 - Partial pressure of O 2 in cerebral tissueSvO 2 - Mixed venous saturationSjvO 2 – Jugular venous saturationrSO 2 – A venous weighted value (75% venous:25% arterial)that measures the regional relative concentrations of oxy-Hband deoxy-Hb; it represents the venous reserve capacityfollowing tissue oxygen extraction2010 Avery EG, White paper; Marin and Moore. Understanding Near-Infrared Spectroscopy. Advances in Neonatal Care. Vol 11,No 6, pp 382-388
Relevant Comparative Variables:rSO 2 vs. SaO 2 , TiPO 2 , SvO 2 , SjvO 2 , f SO 2Reference Title Methods Results ConclusionsJ Clin Monit2000;16:191-9Estimation of Jugular VenousO 2 <strong>Saturation</strong> from CerebralOximetry or Arterial O 2<strong>Saturation</strong> During IsocapnicHypoxiaProspective,observationalN=42 healthy adultsVaried FiO 2 with isoandhypercapniarSO 2 & SjvO 2 ,r=0.9SaO 2 & SjvO 2 ,r=0.77Compared withSjvO 2 , the rSO 2values correlatedmore closely thanSaO 2 ; SjvO 2changed > rSO 2 withhypercapniaNeurol Res1997; 19:246-8Dynamic Changes of Cerebral<strong>Oxygen</strong>ation Measured byBrain Tissue <strong>Oxygen</strong> Pressureand Near Infra-redSpectroscopyProspective, rSO 2 & t i PO 2 ,observationalr=0.73N=10 Neuro ICUt i PO 2 and rSO 2Compared witht i PO 2 , the rSO 2values correlatedwell in head injuredsubjectsInteractiveCardiovascThorac Surg2011; 0 (Dec):1-5Non-invasive Cerebral<strong>Oxygen</strong>ation Reflects MixedVenous <strong>Oxygen</strong> <strong>Saturation</strong>During the VaryingHaemodynamic Conditions inPatients UndergoingTransapical TranscatheterAortic Valve ImplantationProspective,observationalN=20 TA-TAVISvO 2 and rSO 2 at 6time pointsrSO 2 & SvO 2 ,r=0.76Compared withSvO 2 , the rSO 2values correlatedwell in TA-TAVIsubjects indicatingthat rSO 2 reflectssystemic O 2 balance
Validation: rSO 2 Correlates with SjvO 2r = 0.77r = 0.90• 42 healthy volunteers, five levels of SaO 2 atnormocapnia and repeated at hypercapnia• SaO 2 <strong>com</strong>pared against jugular venous blood(SjvO 2 ) demonstrating only fair correlation• Changes in oximetry (rSO 2 ) <strong>com</strong>pared againstchanges in jugular venous blood (SjvO 2 )demonstrating excellent correlationKim M, Ward D, Cartwright C, Kolano J, Chlebowski S, Henson L. Estimation of jugular venous O 2 saturation from cerebraloximetry or arterial O 2 saturation during isocapnic hypoxia. J Clin Monit Comput. 2000;16(3):191-99.
Healthy VolunteersWide Static Normative Cerebral rSO 2 RangeWide Static Normative Distribution of SjvO 2Kim M, Ward D, Cartwright C, Kolano J, Chlebowski S, Henson L. Estimation of jugular venous O2 saturation from cerebraloximetry or arterial O2 saturation during isocapnic hypoxia. J Clin Monit Comput. 2000;16(3):191-99.
ValidationStroke 2010;41:1951-6Anes & Analg 2012;116:834-40
Validation - SummarySeveral validation studies of NIRS rSO 2 have been published using an array of<strong>com</strong>parative physiologic variables and all similarly conclude that although there is noindex test to <strong>com</strong>pare rSO 2 values with, the observed data appears to reflect dynamics ofregional cerebral oxygen balance.Of note, caution should be taken in extrapolating the results of validation studiesperformed with the INVOS monitor to the other devices which claim to measure the sameparameter because the internal processing algorithms and physical characteristics of thefive FDA approved devices are all unique and key to the clinical data that they generate.
Cerebral Oximetry Clinical Studies
Continuous monitoring of cerebral oxygen saturation in elderlypatients undergoing major abdominal surgery minimizes brainexposure to potential hypoxia.Casati A, Fanelli G, Pietropaoli P, et al.Study Design:• Multicenter, prospective, blinded,randomized and controlled trial of 122elderly, high risk general surgery (majorabdominal) patients– Subjects were expected >2 hour operationand were >65 YOAHypothesis:• rSO 2 monitoring with active interventionduring cerebral desaturations in elderlypatients undergoing major abdominalsurgery will reduce the potential exposureof the brain to inadequate oxygen supplyConclusion:• Cerebral desaturations were <strong>com</strong>mon(~20% of patients) during major abdominalsurgery in the elderly and reacting to theseevents prevented exposure of the brain topotential hypoxia. Effective treatment ofthese cerebral desaturations resulted indecreased PACU and Hospital LOS, lesscognitive decline (as assessed by MMSEscores)Anesth Analg. 2005;101(3):740-747
Incidence of Cerebral DesaturationCasati A, et al.Goal for intervention group was to maintain INVOS rSO 2 valuesabove 75% of subject’s established room air baseline. The numberof subjects experiencing cerebral desaturation was similar betweenthe control and intervention groups.Control Groupn = 15 (23%) subjectsWith rSO 2 DesaturationStudy Groupn = 11 (20%) subjectsWith rSO 2 Desaturationp = 0.82Casati A, Fanelli G, Piertropaoli P, et al. Continuous <strong>Monitoring</strong> of Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> in Elderly Patients UndergoingMajor Abdominal Surgery Minimizes Brain Exposure to Potential Hypoxia. Anesth Analg.. 2005; Sep;101(3):740-7
Desaturation Relation to PACU Discharge,LOS and MMSECasati A, et al.9080706050403020100Control InterventionP = 0.017P = 0.002P = 0.01P = 0.02P = 0.007mean rSO2% AUC
Correlation of rSO 2 Desaturation with HospitalLOSAmong the subjectsexperiencing an rSO 2desaturation thehospital length of stay(LOS) significantlycorrelated with themagnitude of thecerebral desaturationsr 2 = 0.40, P = 0.001Casati A, Fanelli G, Piertropaoli P, et al. Continuous <strong>Monitoring</strong> of Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> in Elderly Patients UndergoingMajor Abdominal Surgery Minimizes Brain Exposure to Potential Hypoxia. Anesth Analg.. 2005; Sep;101(3):740-7
Clinical StudiesCardiac SurgeryStudydiscussions.<strong>com</strong>
<strong>Monitoring</strong> brain oxygen saturation during coronary bypasssurgery: a randomized, prospective studyMurkin JM, Adams SJ, Novick RJ, et al.Study Design:Prospective, randomized, blinded,controlled CAB Study, 200 patientsHypothesis:By using the brain as an index organ,interventions to optimize cerebralperfusion will have a similarly beneficialeffect on systemic tissue perfusion andclinical out<strong>com</strong>esConclusion:“<strong>Monitoring</strong> cerebral rSO 2 in coronaryartery bypass patients avoids profoundcerebral desaturation and is associatedwith significantly fewer incidences ofmajor organ dysfunction”Anesth Analg. 2007;104(1):51-58.N=100 control(electronic blinding)N= 100 intervention
Cardiac Surgery - MurkinThe percentage of serious desaturations was significantly greater in thecontrol groupControl GroupStudy Group• rSO 2 AUC < 70% Baseline• rSO 2 AUC < 70% Baseline• > 150 min · %• > 150 min · %• 6 patients• none††p < 0.0142010 Avery ASAMurkin JM, Adams SJ, Movick RJ, et al. <strong>Monitoring</strong> Brain <strong>Oxygen</strong><strong>Saturation</strong> During Coronary Bypass Surgery: A Randomized, ProspectiveStudy. Anesth Analg. 2007 Jan;104(1):51-58.
Efficacy of Desaturation InterventionsMurkin J, et al.Overall % Efficacy of Interventions 80.4%71% (40/56) required > 3 interventionsMurkin JM, Adams SJ, Movick RJ, et al. <strong>Monitoring</strong> Brain <strong>Oxygen</strong> <strong>Saturation</strong> During Coronary Bypass Surgery: A Randomized,Prospective Study. Anesth Analg. 2007 Jan;104(1):51-58.
Reduced ICU Length of StayMurkin J, et al.54MonitoredUnmonitored• ICU length of stay for theintervention group wassignificantly shorterDays321±0.81.25±2.71.87(p
Cerebral oxygen desaturation predicts cognitive decline and longerhospital stay after cardiac surgery.Slater JP, Guarino T, Stack J, et al.Study Design:• Prospective, randomized, controlled,blinded trial in a coronary artery bypassgrafting (CABG) population.– Jan 2004-Feb 2006, n=265 CABG patientsutilizing cardiopulmonary bypass. (n=115control group; n=125 intervention group)Objective:• Examine and describe a relationshipbetween intraoperative cerebral oxygendesaturation and adverse events such asneurocognitive decline and increased lengthof stay.Conclusion :• Intraoperative cerebral oxygen desaturationis significantly associated with an increasedrisk of cognitive decline (OR 2.2; 95% CI[1.11, 4.45], P = 0.024) and prolongedhospital stay (OR 2.71; 95% CI [1.31,5.6], P= 0.007). Mitigating cerebral desaturationsmay reduce these risks.Ann Thorac Surg. 2009;87(1):36-44.
Cognitive Decline and Cerebral Desaturation Predict IncreasedHospital Length of StaySlater J, et al.Odds Ratio for LOS > 6 Days2.521.51p = 0.0412.17Odds Ratio for LOS > 6 Days2.521.51p = 0.00712.220.50.50No CognitiveDeclineCognitive Decline0No CerebralDesaturationCerebralDesaturation** Cerebral desaturation defined by AUC > 3000 sec·% for rSO 2 score < 50% Based on a logistic regression model adjusted forcognitive decline, age, study group, gender, race, HADS, and deliriumAnn Thorac Surg. 2009;87(1):36-44.
ConclusionsSlater J, et al.• Severe intraoperative cerebral desaturation is significantlyassociated with, and predictive of an increased risk of cognitivedecline after CABG surgery as well as increased hospital lengthof stay• Intraoperative management of rSO 2 may result in decreasedpostoperative cognitive decline and less frequent prolongedlength of stay after CABGSlater JP, Guarino T, Stack J, et al. Cerebral <strong>Oxygen</strong> Desaturation Predicts Cognitive Decline and Longer Hospital Stay AfterCardiac Surgery. Ann Thorac Surg. 2009 Jan;(1) 87:36–45
Vascular Surgery
SO 2 and Carotid Surgery• Several studies have examined the utility of NIRS rSO 2monitoring during carotid endarterectomy (CEA) surgery.• The conclusions from these studies have been consistent in thatthey all found a very high negative predictive value associatedwith the use of rSO 2 to detect carotid cross clamping relatedcerebral ischemia when <strong>com</strong>pared to the index of EEGmonitoring.• The observed moderate levels of sensitivity and specificity variedbut do not support using rSO 2 as the sole monitor of cerebralischemia for CEA.
SO 2 and Carotid SurgeryReference Title Methods Results ConclusionsJ Clin Anes2005;17:426A clinical evaluation of near cerebraloximetry in the awake patient tomonitor cerebral perfusion duringCEAProspective,observational study.Index – EEG, awakeexam. N=50Sensitivity 44%Specificity 82%NPV 94%rSO 2 correlates with clinicalsigns and EEG detectedischemia during CEAS African JSurg 2007;45:43Cerebral monitoring during CEA-a<strong>com</strong>parison between EEG,transcranial cerebral oximetry andcarotid stump pressureProspective,observational studyIndex-EEG, stumppressureN=100Sensitivity 100%Specificity 87%NPV 100%PPV 33%rSO 2 has a high sensitivity butlow specificity for ischemiaduring CEA when indexedagainst EEG. rSO 2 changedprior to EEG change duringischemia.J Vasc Surg2008;48:601Cerebral oximetry does not correlatewith EEG and SSEP in determiningthe need for shunting during CEAProspective,observational studyIndex-EEG, SSEPN=323Sensitivity 68%Specificity 94%NPV 98%PPV 47%rSO 2 should not be used as thesole monitor for ischemiaduring CEA. rSO 2 does addinformation regarding cerebralischemia when indexed againstEEG and SSEPEur J VascEndovascSurg 2011;41; 606The role of cerebral oximetry in<strong>com</strong>bination with awake testing inpatients undergoing CEA under localanaesthesia.Prospective,observational studyIndex-awake examN=100Sensitivity 100%Specificity 96%NPV 100%PPV 81%≥19% drop in rSO 2 has a highsensitivity and specificity fordetecting cerebral ischemia<strong>com</strong>pared with awake examCEA–carotid endarterectomy; EEG-electroencephalogram; NPV-negative predictive value; PPV-positive predictive value;SSEP-somatosensory evoke potentials
SO 2 and Neurocognitive Dysfunction
SO 2 and Neurocognitive Dysfunction• Previous clinical studies have indicated that cardiac surgery can be associatedwith an 33-83% incidence of postoperative neurocognitive dysfunction. ‡• The association between physiologic variables representative of cerebraloxygenation and neurocognitive out<strong>com</strong>es was identified almost two decadesago. †• Recently, studies expanding on this work have demonstrated significantassociations between perioperative NIRS rSO 2 values and postoperativeneurocognitive dysfunction indicating a potential to mitigate these unfavorableout<strong>com</strong>es by monitoring and treating observed perioperative cerebraldesaturation.‡Tournay-Jette E, Dupuis G, Bherer L, et al. The relationship between cerebral oxygen saturation changes and postoperativecognitive dysfunction in elderly patients after coronary artery bypass graft surgery. J Cardiothor Vasc Anes 2011;25(1):95-104†Croughwell ND, Newmann MF, Blumenthal JA, et al. Jugular bulb saturation and cognitive dysfunction after cardiopulmnarybypass. Ann Thorac Surg 1994; 58: 1702-8
SO 2 and Neurocognitive DysfunctionReference Title Methods Results ConclusionJ Cardio ThoracVasc Anes 2004; 18:552-8Cerebral oxygen desaturationis associated with earlypostoperativeneuropsychologicaldysfunction in patientsundergoing cardiac surgeryProspective,observationalASEM and MMSEassessed NCDN=101rSO 2 < 40% anindependent predictorof ↑ incidence of bothASEM & MMSEimpairmentrSO 2 desaturation isassociated with earlypostoperative NCD instudied populationJ Cardiothor VascAnes 2011; 25(1):95-104The relationship betweencerebral oxygen saturationchanges and postoperativecognitive dysfunction inelderly patients after coronaryartery bypass graft surgeryProspective,observationalFullneuropsychologicaltesting doneAge > 65 years oldN=61rSO 2 < 50% duringsurgery was associatedwith early NCD. rSO 2 6 d)IntraoperativerSO 2 desaturation issignificantly associatedwith NCD and prolongedhospital stayCrit Care 2011; 15:R218Preoperative regional cerebraloxygen saturation is apredictor of postoperativedelirium in on pump cardiacsurgery patients: a prospectiveobservational trialProspective,observationalDelirium (CAM-ICU)and MMSE assessedNCDN=230Lower preoperativerSO 2 (< 59.5%) is anindependent predictorof postoperativedeliriumLow preoperativerSO 2 is associated withpostoperative deliriumafter on pump cardiacsurgeryASEM-antisaccadic eye movement test; MMSE-mini-mental stateexamination; NCD-neurocognitive dysfunction; BL-baseline; CAM-ICUconfusionassessment method for the intensive care unit
Baseline rSO 2 and Risk StratificationRecently published data suggests that theroom air baseline and oxygensupplemented rSO 2 values may serve as asimple, noninvasive risk stratification toolfor cardiac surgical patients providinguseful insight into 30 day and 1 yearmortality as well as the propensity forpatients to develop postoperativedelirium.Heringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69Schoen J, Meyerrose J, Paarmann H, et al. Preoperative regional cerebral oxygen saturation is a predictor of postoperativedelirium in on-pump cardiac sugery patients: a prospective observational trial. Critical Care 2011;15:R218
Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> andClinical Out<strong>com</strong>es in Cardiac SurgeryHeringlake M, Garbers C, Kabler JH, et al.Prospective, observational pilot studyn = 1,178 patients undergoing on-pumpcardiac surgery in 2008Preoperative determination of ScO 2 (mostlyon the ward)ScO 2 when breathing room airScO 2 during oxygen supplementation(ScO 2min-ox ) -goal: SaO 2 >98%Con<strong>com</strong>itant determination of preoperative:– NTproBNP - Hematocrit - EuroSCORE– hsTNT - GFR - LVEF classFollow up including morbidity and mortality– Morbidity• > 1 major <strong>com</strong>plications (LCOS, stroke, new RRT,reintubation)• and/or high dependency unit stay (ICU+ intermediate care)≥ 10 days– 30-day and 1-year mortalityNTproBNP: N-terminal pro-B-type natriuetic peptide: high sensitivity troponinT; LCOS: low cardiac output syndrome; RRT: renal replacement therapyHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
Correlation of ScO 2min-ox with Peri-Procedural VariablesHeringlake M, Garbers C, Kabler JH, et al.ScO 2min-ox had statistically strong correlations with the followingcovariates that are well accepted predictors of morbidity andmortality in cardiac surgical procedures.– N-terminal pro-B-type natriuretic peptide (ρ; -0.35) †– Troponin T: (ρ= -0.28) †– Hematocrit: (ρ= 0.34)– Glomerular Filtration Rate: (ρ= 0.19)– EuroSCORE: (t; 0.20) †– LV ejection fraction class: (t = 0.12)All: P < 0.0001† These variables, along with ScO 2min-ox ≤ 50%, were all found to be independent predictors of both 30-day and 1-year mortality bylogistic regression analysis.Heringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
ScO 2min-ox and MorbidityHeringlake M, Garbers C, Kabler JH, et al.• Using the predefined study definition of <strong>com</strong>bined morbidity † the ScO 2min-ox ≤60% value had the following ability to predict this endpoint:• AUC 0.68 (95% CI, 0.65-0.70); P < 0.001• Sensitivity = 56.1%• Specificity = 71.%†Morbidity> 1 major <strong>com</strong>plications (LCOS,stroke, new RRT, reintubation) and/orhigh dependency unit stay (ICU+intermediate care) ≥ 10 daysHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
ScO 2min-ox 30 Day SurvivorsHeringlake M, Garbers C, Kabler JH, et al.6560P< 0.000155P< 0.0015045ScO2 room-airScO2 min-OxSurvivors30d-Non-SurvivorsHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
ScO 2min-ox and 30 Day MortalityHeringlake M, Garbers C, Kabler JH, et al.ScO 2min-ox <strong>com</strong>petes with the EuroSCORE as a predictive index of 30-day mortality.AUC EuroSCORE 0.82 AUC EuroSCORE 0.54AUC ScO 2min-ox 0.71 AUC ScO 2min-ox 0.79p=0.015p=0.0044Total CohortEuroSCORE > 10 CohortHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
ScO 2min-ox ≤ 50% and 1 yr SurvivalHeringlake M, Garbers C, Kabler JH, et al.ScO 2min-ox ≤ 50% predicts 1 year mortality <strong>com</strong>pared to ScO 2min-ox > 50%(days)Total CohortEuroSCORE > 10 CohortHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
ScO 2min-ox and Risk Stratification SummaryCorrelations were established between baseline O 2 supplemented rSO 2(ScO 2min-ox ) values and 30-day/1 year mortality as well as a <strong>com</strong>binedmorbidity endpointSignificant relationships between known objective measures ofcardiopulmonary function which serve as risk stratifying tools in cardiacsurgical procedures and baseline rSO 2 values were establishedScO 2min-ox value was nearly as strong a predictor of 30-d mortality as theEuroSCORE in the studied population and even stronger in a sicker, selectsub-group analysisHeringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery.Anesthesiology. 2011; 114(1):58-69
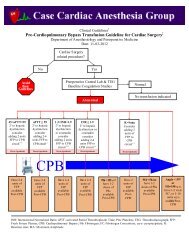
Risk Stratification:STS Database “First Alert”STS Optional Harvest seven rSO 2 data fields• STS Database was queried for the subjective, dichotomous variable (Y/N?) did rSO 2monitoring serve as a first indicator of an intraoperative event (i.e. technical problemor physiologic change) lead that could lead to an adverse out<strong>com</strong>e.• n = 36, 548 out of which 8,406 (23%) entries indicated that rSO 2 monitoring served asa “First Alert” indicator of a potential adverse out<strong>com</strong>e.2010 Avery NIRS White Paper Review
INVOS rSO 2 <strong>Monitoring</strong> EffectivenessStudies in >7,000 patients found clinical and/or economic benefit.All studies using a standardized intervention protocol have found benefit.• Edmonds HL Jr. 1997 Anesthesiology 87:A426• Edmonds HL Jr. 1997 Anesthesia Analgesia 88:SCA26• Schmahl TM. 2000 Anesthesiology 94:A399• Yao F-S-F. 2001 Anesthesia Analgesia 92:SCA86• Yao F-S-F. 2001 Anesthesiology 95;A152• Alexander JC. 2002 Annals Thoracic Surgery 373-C• Goldman S. 2004 Heart Surgery Forum 7:E376• Yao F-S-F. 2004 J Cardiothoracic Vascular Anesthesia 18:552• Casati A. 2005 Anesthesia Analgesia 101:740• Olsson CJ. 2006 J Thoracic Cardiovascular Surgery 131:371• Baker RA. 2006 J Extracorporeal Circulation 8:77• Murkin JM. 2007 Anesthesia Analgesia 104:51
NIRS <strong>Monitoring</strong>
Targets and ThresholdsEdmonds HL Jr, et al. Semin Cardiothorac Vasc Anesth. 2004;8(2):147-166. ; Alexander HC, et al. Ann Thorac Surg. 2002;73 373-C. ; Cho H, et al. J Neurosurg. 1998;89(4):533-538. ; Iglesias I, et al. Heart Surgery Forum. 2003;6:204. ; Edmonds, HL Jr, et al. J Interv Cardiol. 1998;11(3):197-204. ; Yao FSF, et al. Anesthesiology. 2001;95:A-152. ; RobertsKW, et al. Anesthesiology. 1998;89:A934. ; Higami T, et al. Ann Thorac Surg. 1999;67(4):1091-1096. ; Singer I, et al. Pacing Clin Electrophysiol. 1999;22(1 Pt2):216-222. ;Tournay-Jette E, et al. J Cardiothor Vasc Anes 2011;25:95-104.
Targets and Thresholds• Expressed in rSO 2 numerical values and % change from baseline• Patient is his/her own control• Clinical decisions based on patient’s unique physiology andclinical situation– Healthy Cerebral rSO 2 : 58-82 points– Intervention Threshold: ≤ 50 points (or ~20% from baseline)– Critical Threshold: ≤40 points (or ~25% from baseline)
Targets and ThresholdsEdmonds HL Jr, et al. Semin Cardiothorac Vasc Anesth. 2004;8(2):147-166. ; Alexander HC, et al. Ann Thorac Surg. 2002;73 373-C. ; Cho H, et al. J Neurosurg. 1998;89(4):533-538. ; Iglesias I, et al. Heart Surgery Forum. 2003;6:204. ; Edmonds, HL Jr, et al. J Interv Cardiol. 1998;11(3):197-204. ; Yao FSF, et al. Anesthesiology. 2001;95:A-152. ; RobertsKW, et al. Anesthesiology. 1998;89:A934. ; Higami T, et al. Ann Thorac Surg. 1999;67(4):1091-1096. ; Singer I, et al. Pacing Clin Electrophysiol. 1999;22(1 Pt2):216-222. ; Tournay-Jette E, et al. J Cardiothor Vasc Anes 2011;25:95-104.
Clinical Use• Room air baseline established(re<strong>com</strong>mended)• <strong>Oxygen</strong> supplemented baselineestablished (re<strong>com</strong>mended)• 2 Strategies:– Maintain bilateral rSO 2 values within75% of established room air baseline– Maintain bilateral rSO 2 values above50% for patients with a baseline valueof ≤ 50%Heringlake M, Garbers C, Kabler J-H, et al. Preoperative Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> and Clinical Out<strong>com</strong>es in Cardiac Surgery. Anesthesiology. 2011; 114(1):58-69Botes K, LeRoux DA, VanMarle J. Cerebral <strong>Monitoring</strong> During Carotid Endarterectomy- A Comparison Between Electroencephalography, Transcranial Cerebral Oximetry andCarotid Stump Pressure. S Afr J Surg. 2007; 45(2):43-46Kurihara K, Kukukawa A, Kobayashi A, Nakadate T. Frontal Cortical <strong>Oxygen</strong>ation Changes During Gravity-Induced Loss of Consiousness in Humans: A Near-Infrared SpatiallyResolved Spectroscopic Study. J Appl Physiol . 2007; 103:1326-1331Kaminogo M, Ochi M, Onizuka M, Takahata H, Shibata S. An Additional <strong>Monitoring</strong> of Regaionl Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> to HMPAO SPECT Study During Balloon TestOcclusion. Stroke. 1999; 30:407-413Moritz S, Kasprzak P, Arlt M, Taeger K, Metz C. Accuracy of Cerebral <strong>Monitoring</strong> in Detecting Cerebral Ischemia During Carotid Endarterectomy. Anesthesiol. 2007; 107(4):563-569
Desaturation IncidenceCerebral Desaturation > 25% below baseline is <strong>com</strong>mon• CABG Surgery 1 – 42%• Arthroscopic Shoulder Surgery (Beach Chair Position) 2 - 80%• Pediatric Cardiac Surgery 3 - 58%• Non-Cardiac Geriatric Surgical Patients 4 - 26%1 Edmonds HL. Protective Effect of Neuromonitoring During Cardiac Surgery. Ann NY Acad Sci . 2005; 1053:12-192 Murphy GS, Szokol JW, Marymont JH, et al. Cerebral <strong>Oxygen</strong> Desaturation Events Assessed by Near-Infrared Spectroscopy During Shoulder Arthrsocopy in the Beach Chairand Lateral Decubitus Positions. Anesth Analg 2010; 111:496-505.3 Austin EH, Edmonds HL, Auden SM, et al. Benefit of Neurophysiologic <strong>Monitoring</strong> for Pediatric Cardiac Surgery. J Thorac Cardiovasc Surg . 1997; 114:707-7174 Casati A , Fanelli G, Pietropaoli P, Proietti R, Tufano R, Montanini S. <strong>Monitoring</strong> Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> in Elderly Patients Undergoing General Abdominal Surgery: aProspective Cohort Study. Eur J Anesth. 2007; 24:59-65
Dynamic rSO 2 Alarm Criterion: baseline -20%• Conscious -15% 1-6• Anesthetized -20% 7-9“It’s too early to re<strong>com</strong>mend specifictarget rSO 2 that should bemaintained in different clinicalsettings.” 10Without baseline and dynamic threshold, a fixed alarm threshold of 50 is widely used 11,12- healthy normative mean -20%- bottom of cardiac normative range- baseline rSO 2
Clinical Interventions
Interventions to Improve rSO 2Mechanical Cause:– Head position– Cannula positionIncrease Supply (<strong>Oxygen</strong> Delivery):– Increase blood pressure– Normalize CO 2 to physiologic level– Increase FiO 2– Increase cardiac output (pump flow)– Increase hematocritDecrease Demand (cerebral metabolism):– Increase anesthetic depth– Decrease body temperature-Yao FS, Levin SK, Woo D, et al. Maintaining Cerebral <strong>Oxygen</strong> <strong>Saturation</strong> During Cardiac Surgery Shortened ICU and HospitalStays. J Cardiothorac Vasc Anesth 2004;18(5)5:552-558.-Denault A, Deschamps A, Murkin JM. A Proposed Algorithm for the Intraoperative Use of Cerebral Near-Infrared Spectroscopy.Sem Cardiothor Vasc Anesth. 2007: 11:274-281
<strong>Monitoring</strong> Algorithms HelpMitigate rSO 2 DesaturationDenault A, Deschamps A, Murkin JM. A Proposed Algorithm for the Intraoperative Use of Cerebral Near-Infrared Spectroscopy. SemCardiothor Vasc Anesth. 2007: 11:274-281
NIRS in Clinical practice
Clinical Application: NIRS Cerebral rSO 2• Cardiovascular surgery procedures (CABG,Valve, CEA, Vascular Stenting, TAVI)• Thoracic surgery (single lung ventilation)• Electrophysiology lab procedures (RFAablation of VT or AFIB)• Surgical procedures involving controlledhypotension• Elderly general surgery patients• Orthopedic surgical patients (beach chairprocedures)• ICU patients– severe pulmonary infections, ARDS– septic or cardiogenic shock– Intracranial hypertension– Intracranial hemorrhage– Cerebral vasospasm– Seizures• Neck hematoma (line related)• Compartment syndromefrca.co.uk2010 Avery NIRS White Paper Reviewtheuniversityhospital.<strong>com</strong>ortho.umn.edu
Conclusions• Clinicians will be increasingly challenged to maintain and/or improveupon the presently achieved clinical out<strong>com</strong>es in our aging population• NIRS is non-invasive and reveals regional tissue oxygen saturation(an index of tissue oxygen balance), in contrast to relying uponassumptions related to “acceptable” physiologic parameters (e.g.,MAP of 50-60 mmHg on CPB)• Peer reviewed studies found robust support of the idea that the INVOSrSO 2 value represents an index of regional cerebral oxygen balance• Evidence supports the use of INOVS monitoring in Cardiac,Orthopedic, General, and Vascular surgery to alert the clinician tohypoperfusion and/or mechanical obstruction which may result inpoor clinical out<strong>com</strong>es
ClickHerewww.casecag.<strong>com</strong>
Thank you