Guideline on Treatment of Patients with Severe and Multiple ... - AWMF
Guideline on Treatment of Patients with Severe and Multiple ... - AWMF
Guideline on Treatment of Patients with Severe and Multiple ... - AWMF
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
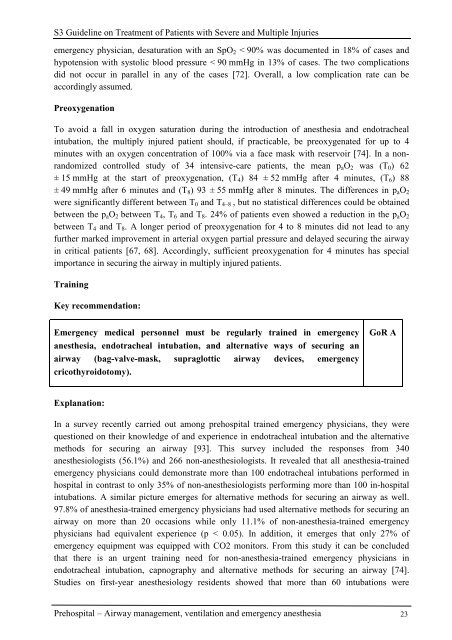
S3 <str<strong>on</strong>g>Guideline</str<strong>on</strong>g> <strong>on</strong> <strong>Treatment</strong> <strong>of</strong> <strong>Patients</strong> <strong>with</strong> <strong>Severe</strong> <strong>and</strong> <strong>Multiple</strong> Injuries<br />
emergency physician, desaturati<strong>on</strong> <strong>with</strong> an SpO2 < 90% was documented in 18% <strong>of</strong> cases <strong>and</strong><br />
hypotensi<strong>on</strong> <strong>with</strong> systolic blood pressure < 90 mmHg in 13% <strong>of</strong> cases. The two complicati<strong>on</strong>s<br />
did not occur in parallel in any <strong>of</strong> the cases [72]. Overall, a low complicati<strong>on</strong> rate can be<br />
accordingly assumed.<br />
Preoxygenati<strong>on</strong><br />
To avoid a fall in oxygen saturati<strong>on</strong> during the introducti<strong>on</strong> <strong>of</strong> anesthesia <strong>and</strong> endotracheal<br />
intubati<strong>on</strong>, the multiply injured patient should, if practicable, be preoxygenated for up to 4<br />
minutes <strong>with</strong> an oxygen c<strong>on</strong>centrati<strong>on</strong> <strong>of</strong> 100% via a face mask <strong>with</strong> reservoir [74]. In a n<strong>on</strong>r<strong>and</strong>omized<br />
c<strong>on</strong>trolled study <strong>of</strong> 34 intensive-care patients, the mean paO2 was (T0) 62<br />
± 15 mmHg at the start <strong>of</strong> preoxygenati<strong>on</strong>, (T4) 84 ± 52 mmHg after 4 minutes, (T6) 88<br />
± 49 mmHg after 6 minutes <strong>and</strong> (T8) 93 ± 55 mmHg after 8 minutes. The differences in paO2<br />
were significantly different between T0 <strong>and</strong> T4–8 , but no statistical differences could be obtained<br />
between the paO2 between T4, T6 <strong>and</strong> T8. 24% <strong>of</strong> patients even showed a reducti<strong>on</strong> in the paO2<br />
between T4 <strong>and</strong> T8. A l<strong>on</strong>ger period <strong>of</strong> preoxygenati<strong>on</strong> for 4 to 8 minutes did not lead to any<br />
further marked improvement in arterial oxygen partial pressure <strong>and</strong> delayed securing the airway<br />
in critical patients [67, 68]. Accordingly, sufficient preoxygenati<strong>on</strong> for 4 minutes has special<br />
importance in securing the airway in multiply injured patients.<br />
Training<br />
Key recommendati<strong>on</strong>:<br />
Emergency medical pers<strong>on</strong>nel must be regularly trained in emergency<br />
anesthesia, endotracheal intubati<strong>on</strong>, <strong>and</strong> alternative ways <strong>of</strong> securing an<br />
airway (bag-valve-mask, supraglottic airway devices, emergency<br />
cricothyroidotomy).<br />
Explanati<strong>on</strong>:<br />
GoR A<br />
In a survey recently carried out am<strong>on</strong>g prehospital trained emergency physicians, they were<br />
questi<strong>on</strong>ed <strong>on</strong> their knowledge <strong>of</strong> <strong>and</strong> experience in endotracheal intubati<strong>on</strong> <strong>and</strong> the alternative<br />
methods for securing an airway [93]. This survey included the resp<strong>on</strong>ses from 340<br />
anesthesiologists (56.1%) <strong>and</strong> 266 n<strong>on</strong>-anesthesiologists. It revealed that all anesthesia-trained<br />
emergency physicians could dem<strong>on</strong>strate more than 100 endotracheal intubati<strong>on</strong>s performed in<br />
hospital in c<strong>on</strong>trast to <strong>on</strong>ly 35% <strong>of</strong> n<strong>on</strong>-anesthesiologists performing more than 100 in-hospital<br />
intubati<strong>on</strong>s. A similar picture emerges for alternative methods for securing an airway as well.<br />
97.8% <strong>of</strong> anesthesia-trained emergency physicians had used alternative methods for securing an<br />
airway <strong>on</strong> more than 20 occasi<strong>on</strong>s while <strong>on</strong>ly 11.1% <strong>of</strong> n<strong>on</strong>-anesthesia-trained emergency<br />
physicians had equivalent experience (p < 0.05). In additi<strong>on</strong>, it emerges that <strong>on</strong>ly 27% <strong>of</strong><br />
emergency equipment was equipped <strong>with</strong> CO2 m<strong>on</strong>itors. From this study it can be c<strong>on</strong>cluded<br />
that there is an urgent training need for n<strong>on</strong>-anesthesia-trained emergency physicians in<br />
endotracheal intubati<strong>on</strong>, capnography <strong>and</strong> alternative methods for securing an airway [74].<br />
Studies <strong>on</strong> first-year anesthesiology residents showed that more than 60 intubati<strong>on</strong>s were<br />
Prehospital – Airway management, ventilati<strong>on</strong> <strong>and</strong> emergency anesthesia 23