SREE CHITHRA TIRUNAL INSTITUTE FOR MEDICAL SCIENCES TECHNOLOGY
sree chithra tirunal institute for medical sciences & technology
sree chithra tirunal institute for medical sciences & technology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>SREE</strong> <strong>CHITHRA</strong> <strong>TIRUNAL</strong> <strong>INSTITUTE</strong> <strong>FOR</strong><strong>MEDICAL</strong> <strong>SCIENCES</strong> & <strong>TECHNOLOGY</strong>Thiruvananthapuram - 695 011PROJECT REPORTNameProgrammeMonth & Yearof submissionRAKESH.P.GOPALD. M. CardiologyNovember 2001
CERTIFICATEI, Dr. Rakesh P Gopal, hereby declare that the projects1nentioned here .were undertaken by me under the supervision ofthe faculty.~~&~ SignatureDr. RAKESH P. GOPALTrivandrum12-l I -2001.Forwarded. He has carried out the minimum required procedures.~Dr. JAGANMOHAN A. THARAKAN.HEAD OF THE DEPARTMENT
PROJECTSUTILITY OF WEEKLY ORAL AZYTHROMYCIN IN PREVENTIONOF GROUP A BETA HEMOLYTIC STREPTOCOCCAL THROATCOLONIZATION, INFECTION AND RHEUMATIC FEVER.FAMILY STUDY OF FOUR PROBANDS WITH HYPERTROPHICCARDIOMYOPATHY DUE TO DELETION MUT A TlONS IN MYH 7AND MYBPC 3 GENES.
UTILITY OF WEEKLY ORALAZITHROMYCIN IN PREVENTION OFGROUP A BETA HEMOLYTICSTREPTOCOCCAL THROATCOLONIZATION, INFECTION ANDRHEUMATIC FEVER.
INTRODUCTIONSecondary prophylaxis with antibiotic against streptococcal infection is a landmark public health intervention evolved in the last century(l ). Injectable long actingpenicillin once in three weeks is the gold standard, 1 but not widely practiced in keralabecause of the fear of anaphylaxis(2). Oral penicillin and erythromycin in a twice-dailydose is at present used as an alternative.Azithromycin is an orally effective antibiotic with a long half life and there arereports highlighting its utility in prevention of streptococcal infection( 17). lienee itsutility in preventing rheumatic recurrence was evaluated against oral penicillin.REVIEW OF LITERATURERheumatic heart disease remains a major cause of cardiovascular morbidity andmortality in our country despite the fact that it has declined in the west except lorresurgence in the 1980's. Rheumatic fever and rheumatic heart disease constitute 35-40'%of admissions to hospitals in India(3). The enigma of how group A Beta hemolyticstreptococci (GAS) cause rheumatic fever is evading us. But, what is obvious is that it iseasily preventable by simple means at a negligible cost. It is more economical to preventrheumatic fever than treat rheumatic heart disease. After a GAS throat infection, 0.3
J% of patients develop rheumatic fever. ICMR has projected that 2 II per thousandschool children and 1.22 per thousand of adult population in India have rheumaticfever or rheumatic heart disease(6). Considering the fact that 49 1 % of Indian populationarc school age children, we have a load of 1.2 -2 millions patients with this problem.This is alarming when we take into account that there are only 30 hospitals in Indiacapable of performing surgery for RHO, majority of them performing less that 200 suchsurgeries per year. Our health budget is a meager 2% of our GOP.6. Most of the patientsdie of RHO in the prime of their life for lack of money and availability of treatment. It isimpossible for a country like ours to handle such a heavy burden.Only rheumatogenic strains of GAS, infecting throat, virulent enough to causeimmunologic response in the host cause rheumatic fever(7,8,9, I 0). Streptococcal throatcolonization has not been known to have any effect in pathogenesis(29). The number ofstreptococcal infections has neither increased nor decreased in the last I 00years.( 1,1 I, 12,13 ). GAS is found in appreciable number of carrier throats. 15 to 25'Yt, ofchildren arc carriers, making eradication of carrier state nearly impossible. A highlycJTicicnt vaccine supplied through an extremely efficient public health system may be ananswer for this menace. But this may not be financially viable. Since rheumatic episodeshave a tendency to recur with no prophylaxis - it could recur as many as 5 times in anaverage patientand has higher chance of recurrence in those who had it once and thedamage gets worse with every recurrence, secondary prophylaxis prmmscs the bestpossible intervention in our population( 14 ).
Secondary prevention has evolved from the beginning of last century, from theearly days of sanatoria, to the introduction of sulfadiazine in the early I 940's through thegrund entry of penicillin in the mid 1940's(14). Penicillin is the land mark discovery in(14). Injection BP leads to an early peak in serum levelsuf"lleient to eradicate GAS from throat and levels adequate to prevent colonization untilnext dose( 15, 16). But, the problem with BP is compliance. It is very painful, has to beadministered to an otherwise healthy patient on a regular basis, and it carries a risk of lifethreatening anaphylaxis . Mortality figures with penicillin anaphylaxis is not alarming,but what is alarming is the fear among the patients, relatives and health careprofessionals.2. Also, it's usc is cumbersome in patients on oral anticoagulants,especially in those withprosthetic valves. Not withstanding are problems related toinjections per se and traumatic determinism.BP is even banned in certain states bylaw( 17). There is also a possibility that penicillin may promote the emergence or otherresistant organisms that colonize the throat. Respiratory infection per sc is an importantcause of morbidity and mortality in the young. Penicillin causes a significant qualitative
and quantitative decrease in both the composition of inhibitory flora and its interferenceactivity in preventing infection by pathogenic bacteria. These effects persist for weeks.Elimination of alpha streptococci from throat eliminates their ability to producehactcriocin which arc part of the natural host defense mechanisms(30,31 ). Artificiallycolonizing patients with alpha streptococcus using throat samples of live bacteriagenerally prepared from patients own throat has been suggested as a possible therapeuticstrategy- Bacteriotherapy(32).Variability in colonization characteristics, drug resistance and GAS virulence areother problems of chemoprophylaxis as a population based strategy. However, theefficacy of BP was proved beyond doubt in the 1960's Irvin&rton House studies, when itwas proved superior to oral penicillin and sulfadiazine. Sulfa has shown a recurrence rateof 2.6/100 patient years in U.K- US trials and also, sulfa is a drug frequently associatedwith troublesome if not life threatening side efTects(l4).Another alternative isErythromycin. Both these drugs arc to be administered twice daily. Cost and complianceproblem arises here also.In Irvington House study itself: despite the help of trainedsocial workers, the compliance to oral penicillin was only 50%,. In Baltimore, it was onlyJ2%. Japanese statistics show 36%, Taiwanese 49% non-compliance. Soncto reports acompliance of only 17'% which could be increased to 38 1 % through a community heulthcare programme. Those with minimal disease or no RHD arc more likely to defaultThis is actually the higher risk population likely to contract and spread disease and add tothe burden of RHD( 14). This paves the way for newer drug trials. Recently, once a weekural Azithromycin proved effective, as prophylaxis for agents causing acute respiratorytract infections including streptococcus(l5). It could be a safe und effective alternative
for those who arc not tolerating Penicillin and Erythromycin and in those whom theorganisms are sensitive. Once a week prophylaxis has the added advantage of complianceand problem of multiple doses can be avoided. Many a times, the twice duily dose iscircumvented or not practically adhered to, by the patients.Azithromycin is a novel 15 membered Azalide antibiotic( 18). Its nuclearstructure differ from that of Erythromycin in that the lactone ring contains a nitrogenatom. This molecular arrangement gives Azithromycin (Azt) unique pharmacologicalproperties. It is extremely acid stable (Azt is 300 times more stable than Erythromycin)and well absorbed with oral intake.Most important characteristic of Azt is that itpenetrates very well into tissues and is concentrated in macrophages, PMN, monocytesand fibroblasts which mayserve as a delivery vehicle for this agent to the site ofinfection. Azt is probably transported into cells because of its dibasic, amphiphilicdmracter, thus behaving as a classic lysosomotropic agent(18,20). Because it is rapidlydistributed in tissues serum levels arc very low after standard dosing. Since the drug ishighly concentrated in tissues and then slowly released, it has a very long biologic halflite. The drug does not have any deleterious effect on cellular function despite high intracellular concentration. Spontaneous release of Azt from fibroblasts and phagocyles is aHlow process. However, release from phagocytcs is enhanced by exposure ol' the celllllcmbranc to bacteria.It can ofT load as much as 82% of the drug upon bacterialchallenge. Release of the drug li·mn fibroblasts is not enhanced by bacteria , thus servingthe purpose of a reservoir. Azithrornycin is bactericidal for most gram positiveorganisms. Drug inhibits streptococcus pyogenes, group A,B,C,F,G streptococcal
species, hemophilus, streptococcus bovisand viridans. 1t acts by inhibiting 50S ribosomesub units and interferes with translocation( 19-23).Following a single oral dose of 500mg, Azt is eliminated from serum in apolyphasic manner.Initial rapid decline in the plasma level is due to the tissuedistribution and late by distribution and elimination.Terminal elimination phase ischaracterized by movement of Azt from the tissue compar1ments into the vascularcompartment, elimination by I iver and trans intestinal passage. Terminal serum hal f-1 i fewith a 500mg single oral dose is more than 40 hours.20.Baldwin et al in u trialconducted in UK measured pulmonary tissue concentration of Azt after a single oral doseof 500mg. Concentration of Azt achieved in sputum (mean peak 1.56mg/L), bronchialIIJucosa (mean peak 3.89mg/L) and alveolar macrophages (mean peak 23mg/L) wereHustained for 4 days well above an MIC of most respiratory pathogens includingstreptococci. Predominant portion of absorbed Azt remains un metabolized in the body.When metabolism occurs, it is primarily by de methylation. Metabolites have no antimicrobial activity. 20. This long effect makes it an ideal agent suitable for widely spacedintervals of administration.
AIMTo study the utility of once weekly oral Azithromycin in prevention of group ABeta hemolytic streptococcal throat colonization, infection and acute rheumatic fever.METHODSConsecutive patients attending the RHO clinic of SCTIMST, who were willing lo befollowed up as per protocol during the period between June 1999 to Murch 200 I, notallergic to pcnici11in and Azithromycin were randomized to receive either weekly oral500mg Azithromycin or Phenoxy methyl penicillin 250mg twice daily in this open lube!study. All patients gave informed consent.For study purpose, following definitions were made.I) Streptococcal coloni:zation: Those with positive throat culture alone.2) Streptococcal throat infection : Those associated with positive throat swab culture andtwo f(>ld rise in ASO titre ..\) Rheumatic fever: Diagnosis based on modified Jones criteria and newly set echocriteria for mitral regurgitation and aortic regurgitation.4) Patients getting GAS throat infection were considered to have rheumatic reactivationunless proved otherwise. Every attempt was made to prevent rheumatic reactivation. Allpatients were instructed to report immediately if they develop sore throat lor evaluationund sledge hammer treatment as per WHO recommendation at the curliest, to eradicatethe nidus of infection.10
5} Cure of GAS infection was defined as negative throat culture at the end of I 0 days.Further evaluation f(x rheumatic fever recurrence was done at 3 weeks.It was planned to cross over between the groups i r secondrecurrence occurred. A third recurrence was supposed be taken as an indication to changeover to B.P. Patients were evaluated at randomization, at one month, 3 months and 6months clinically by ASO and throat swab culture. End points supposed were uhsencc ofstreptococcal colonization, infection or rheumatic fever at the end of 6 months./.AI/ORATORY STUDIESLab personnel were blinded with regard to treatment arms.Throat culture,sL~nsitivity and serology were done by standard methods. Throat swab was obtained usingsterile swab and immediate plating was done in blood agar. Gram stain was done alter 48hr of culture and sub culture was done whenever nescessary. ASO was done using latexugglutination in serial dilutions.11
RESULTIt was an open lubel study.Treatment arms were selected us1ng the tublc ofrundom numbers.All patients included in this study gave informed consent. Thosepatients with co-morbid problems and non-compliance and staying l~1rawuy who couldnot come for follow up were excluded from the study. There were a total of 4X patientsof which 20 (42 1 %) were males and 28 (58%) females. Mean age was 29.4 years undmedian was 30 years.l9 patients were from poor socio-economic class and the rest weremiddle class. Base line characters were comparable in both groups. The median age offirst attack of rheumatic fever by history was 11.5 years. All patients who had rheumaticJ'ever, reported antecedent sore throat at the time of their first ever attack. l\tl it ral valvedisease was the most common RHO, of which mitral- stenosis was the predominantlesion. 19 patients (39.5%1) had PTMC prior to inclusion the study. Most pulient hadclass II symptoms (56.3%1 ).Rest were Class I. 94%) of patients were in normal sinusrhythm. Rest had atrial fibrillation. None had angina or syncope. J 5 patients ( 31.-VYtl) hadpalpitation. One patient wus hypertensive. One was marfanoid. Hemoptysis was presentin J patients ((>.25%). I patient had a co-existing small ASD with less than 2: ILen to Right shunt by cardiac catheterization. CV A had complicuted 7 patients ( 14.(1%)prior to study.One patient among the 48 had an episode of rheumatic fever one month prior tothe enrolment. None of the other patients had recent history of rheumatic f'cver. Mediandural ion since the last episode of rheumatic fever in study population was I 0 years. 2patients in Azt group and 3 patients in penicillin group gave history of throat pain lasting12
3-4 days within the last one year prior to entry into the study. One patient hud receiveduntibiotic from the local doctor. None of the rest had consulted a doctor.UASI~LINE CHARACTERSTotal No of Patients 48Penicillin group 221\zilhromycin group 26Mean Age29.3 yrsMedian Age30 yrsMule 20Female 28Socio economic statusPoor 19(39.6%)Middle Class 29(60.4%)RhythmNSR 45(93.8%)Atrial Fibrillation 3 (6.2°;(>)SymptomsClass 2 27(56.25%)('luss ] 21(43.75 1 %)l.esionsPost mitral valvotomy I
DATA ON FIRST ATTACK OFRHEUMATIC FEVER1\kan ageI :everSore throatArthralgiaChoreall.t: yrs50'!;(,50'%41 'Y.,NilBASELINE CIIARACTERESTICS OF BOTH THE GROUPSAZITHROMYCINPENICII.LINMEAN AGE 29.2 .10SEXMALE II 10FEMALE 15 12SOCIOECONOMIC CLASS 54.6'% 4'\A%11/0 IU I. FEVER 54% 50";,RIIDMS 419 5i1)MR 4/9 '>i
During the study, 4 patients (15.4%) in Azt !,TfOup had sore throat und fever.Lymphadenopathy was seen in two of them. All 4 patients who had sore throat hadpositive throat culture for GAS and elevated ASO indicating GAS infection of throat.None did confirm the criteria for diagnosis of rheumatic fever reactivation.The following is the summary of those who had recurrence of GAS infection:A I: had GAS throat infection while into 3 months of the study .He presented with fever,sore throat and cervical lymph adenopathy .He is a 24 year old man doing agriculturerelated work, belonging to low middle class family. He is in NSR and has mild MR ashis cardiac lesion. He was given curative treatment and in 10 days his throat culture wasnegative. His cardiac status remained same. He was continued on weekly Az.t with nofurther recurrence./\2: had recurrence of GAS sore throat within 3 months of study. He is a J I yr oldmumwl laborer, presented with fever and sore throat. This patient has had PTMC forsevere MS I year back and is in sinus rhythm. He has class I-II symptoms.AJ: is a 42 year old medical nurse, had sore throat and fever with cervicalLymphadenopathy within one month of starting the study drug. She bas mild M R ascardiac lesion. Patient is in NSR./\4: is a clerk ,37 year old lady having mild MS and MR as cardiac lesions with class 1-11symptoms, presented with fever and sore throat within 2 months of study. she is in sinusrhythm and her curdiac status remained same.All patients who had sore throat reported within 3 days of onsets1ncr they wereinstructed to do so. Sledge hammer therapy was instituted as per WHO recommendation.15
They were followed up for 4 weeks and no evidence for rheumatic reactivation could bedemonstrated in any of them- acute phase reactants and PR interval remained normal.No patient had arthritis, carditis, chorea, subcutaneous nodules or erythema murginatum.As per protocol, study drug was continued in all of them. No further recurrence ofinfection occurred in any of the patients. 3 patients ( 11,51% ) in the Azt groupcomplained of stomach upset, and 1 patient (3.8%) had a change in appetite.None in the penicillin group reported any problem.Clinical status of heart disease remained same throughout the study period in allpatients. None required hospitalization for any purpose. Though drug compliance wasexpected, default can not be excluded as therapy was not supervised.16
DISCUSSIONThe present study to evaluate utility of Azt in secondary prophylaxis of rheumaticlever could enroll only patients with established rheumatic heart disease, since our centeris a tertiary care hospital. No patient at entry to study had isolation of GAS in throatt~ulture or rheumatic fever.Median age of study population was 30 years. This is because of the referral basisof our centre, which primarily caters those patients requiring interventions. Almost all of..the first episode of rheumatic tever was treated by the local paediatrician or pediatricrcfcrrul hospitals. Female sex predominated in the population studied.lntervenlionalpmctice in our institute may be the cause that more patients had MS requiring valvotomy.l'u~thistory of sore throat and arthritis was present in 50% of patients. Incidence ofurthritis in the literature is 75'%.None of our patients in the penicillin group had treatment failure_ ie, either GASthroat infection or colonization. Reported penicillin V tolerance however is 25- 40%.(24 ).Andrews et al reports 5 -- 10 1 )1(, of patients not responding to penicillin tlh:rupy forlonsillopharyngitis. Since penicillin resistance is unknown in GAS sore throut, ubility ofthe bacteria to enter a protected environment beyond the reach of antibiotics has beenoffered as an attractive explanation lor treatment failure(25).A significant number of patients ( 15.4 1 Yo) in Azt group had GAS throat infectionus evidenced by clinical pharyngitis, positive throat culture and elevated ASO. But, noneltad rheumatic fever recurrence as per modified Jones criteria. After curative treatment,17
when the study drug was continued, no recurrence was noted.There is no duta in theliterature on the usc of Azt in the secondary prophylaxis of rheumatic fever. However,there is a report by Giovanni Ghirga et al on occurrence of rheumatic lever atlcr asuccessful treatment of GAS throat infection by Azt(26).Erythromycin, anotherMacrolide, has been reported with a I 5-24'% chance of recurrence(27). Why Azt failed toprevent GAS infection in 15.4% of patients is not very clear. One possibility is that drugdosage was too widely spaced. Though Azt has a long half life drug concentration mightnul have been adequate in this high risk population at the end of dosage interval. It is notknown whether shorter intervals of drug dosage would be of help. Other possibilitiesinclude poor patient compliance, failure of the drug to reach in adequate concentration inthe mucosa, microbial tolerance to azithromycin, recurrent exposure of puticnts toviwlent strains of GAS, suppression of natural immunity and disturbance of normal floraof throat. Azithromycin inhibits growth of alpha streptococci that are normal defenders ofplwryngeal mucosa against pathogens at lower MIC(21 ).Gregory c Gray et al reported superiority of weekly oral Azt in prevention ofugcnts causing respiratory disease over penicillin when used as prophylaxis in 101 (> US111arinc trainees at high risk of respiratory disease. Azithromycin group reported less sided'lccts, respiratory symptoms and serological evidence for streptococcal, mycoplasmalami chlamydia! infections( 15). This paradigm could be extended to prevention of acutecoronary events, since studies do highlight the role of infections in their genesis.Thomas ct al studied Azt and penicillin-V for the treatment of streptococcalpharyngitis. In both the groups 99%, were clinically cured or improved. GAS could becrudicated in 91 '% in Azt compared to 96% of penicillin group. Of the patient who had18
ecurrence, clinical evidence of infection was seen in 23'% of patients treated with Aztand 70'% of patients treated with penicillin. Side effects were insignincunl and similar inhoth the groups. Thomas et al hud 4%, failure in acute GAS infection treatment withAzt.22. Our study showed a recurrence of infection as high as 15.4'%. This is dclinilclyhigh for a low volume of puticnts. It is arguable that these are patients with establishedRll D and constitute a high risk group. Again, as the age of patients inc reuse, theincidence of inlcction could have been lower, which was not the case.As the truemcidcnce of GAS inlcction in the adult population in India with RHD is not available,this study points to a possible high incidence, warranting definite continuation ofprophylaxis well into adult life. The fact that rheumatic fever did not occur despite GASin fcction is not unexpected as number of patients who had GAS throat infection was lowund rheumatogcnicity of the struin was not looked for.Bruna Facinclli et al explains the potentially serious difficulty that could ansefrom the use of macrolides to kill intracellular GAS. They found a significant associationbetween the gene of macrolide resistance and protein Fl invasion (prt Fl) which suggestthat the macrolide resistant strains arc more invasive than sensitive ones. These strains inthe same cusc would be resistant to penicillin also. In the general population surveys,uhout 50-60 1 111 of serotype of GAS were found to have the prt Fl gene(28).Intracellular accumui::Jtion of macrolidcs have been shown in lcucocytcs hut not inepithelial celb, which ure probably the principal cells targeted by GAS. In lcucocytes1\:t.l accumulates predominantly in lysosomes, where as intracellular GAS is found inplwgosomes and cytosol(25).19
lntrucellular localizution of antibiotics does not necessarily correlate with theiructivity against intracellular pathogens.This discordance could due be in part tomacrolide induceJ suppression of nuclear factor K Beta in epitheliul cells, which in turnwntrols cytokine proJuction by target cells and affect their ability to kill puthogens or inpart because the antibacterial activities of cytokine and macrolides are synergistic oradJitive at the intracellular sites where macrolides do accumulate in a high concentrution.Macrolide accumulation in epithelial cell is less, this could be the reason why GASescape in throat epithelium. Only GAS capable of persisting in cukaryotic cells for along time without lysing the cell will be capable of evading host defense mechanism andtl1e activity of extra cellular antibiotics for extended periods. This challenge, infection setut epithelium, however could be enough lo generate a systemic immunologic responsethut could potentially puve way for rheumatic fever(25). Other unexplored problems arevariability in GAS colonization, drug resistance and change in virulence of GAS.At this point of time and with present number of patients and dose, A;t is not aspromising as penicillin lor GAS prevention. However, Azt could be un alternative forthose who are allergic to penicillin and sulfa at a higher or more frequent dose. Becauseor the significant recurrence ,it is proposed to redesign the study and continue asbiweekly oral 500 mg Azithromycin and twice daily 250 mg oral penicillin, pendingethical committee cleurance.('()ST EFFI~CTIVENESSTreatment cost of weekly oral 500 mg Azt and twice daily 250 mg oral Penicillinis same. A biweekly regime of' Azt will obviously be twice as expensive.20
CONCLUSIONAzithromycin 500 mg orally once in a week is not effective in prevention ofret:urrcnce of streptococcal throat infection and cannot be recommended for rheumaticfever prophylaxis.DRAW BACKS OF THE STUDYI. Higher age of study population, well above the rheumatic fever age.2. Small number of patientsJ. No patient with acute rheumatic fever was enrolled for study, all were patients withestablished rheumatic heart disease.4. No clwractcrization of the rhcumatogcnicity of the strain was attempted ..'i. Additional studies on immunity, PCR based detection and antibody assays arc neededto give a solid foundation for chemoprophylaxis.21
REFERENCESI. Gene H Stollcnnan: Changing streptococci and prospects for the global eratlication ofrheumatic fever .Perspectives in Biology and Medicine,40,2. Winter 1997 165-89.2 .. Zulfikar Ahammcd M: Progress in Pediatric cardiology, volume Ill Rheumaticlever- 1999.:1. Community control of rheumatic heart diseases in developing counties. I .a majorpublic health problem. WHO chronicle 1980; 198034:389-954. Ani! Grover et al Criteria for success and failure in rheumatic fever prophylaxis: a lookhl~yond Duckett Jones. rndian Journal of cardiology vol 3 no 1-4, 57-63.5. Narula et al, Sccontlary prevention of Rheumatic fever; theory ,practice, and analysisof available stutlies Rheumatic fever,. American Registry of Pathology,191 >9.(t. Krishna swamy et al Demands on tertiary care for cardiovascular diseases in India;unulysis of data for I %0-89.Bull WHO t 991 ;69:325-30.7. Feinstein et al Reheumutic fever in children and adolescents a long term epidemiologicstudy of subsequent prophylaxis, streptococcal infections and clinical scquulae. Vi.Clinical features of streptococcal infection and rheumatic recurrences. Ann.intcrn Med1%4;60 (suppl 5):(>8-86.8. Stroud Wd et al the clinical importance of infection of the respiratory tract inrheumatic fever .lAMA 1939; 113;902. REFERENCES:1>. Taranta A. Wood HF. Feinstein AR, Simpson R, Kleinberg E. Rheumatic rever inchildren and adolescents. A long term epidemiologic sh1dy of subsequent prophylaxis,Htrcptococcal infection, and clinical sequalae. IV. Relation of the rheumatic feverrecurrence rate per streptococcal infection to the titer of streptococcal antibodies.Ann. Intern. Med. 1%4,60 (Suppl 5): 47- 57.I 0. Stroud WD. The clinical importance of infection of the respiratory tract in rheumatickver .lAMA 19:19, 113: 902.II. Boone .lA, Levine SA. The prognosis in potential rheumatic heart disease undrheumatic mitral insunicienty. Am J Ped 1989; 114: 334-5.12. Boxcrbaum. B, Prevention of rheumatic fever. J. Pediat 1990, 117: 842.13. Boxcrbaum. B, Prevention of streptococcal neurosis. Primary care 1981; 8: 583-91,22
14. Y .Chandrusekhar, secondary prevention of Rheumatic fever: Theory, practical andunulysis of available studies: Rheumatic fever, Narula J. Virmani R, Reddy KS, TandonJ{ cl al; American Registry of Pathology, 1999.15. Gregory C, Gray, MD, M.P.H, .Joel Escamilla PHD, Kenneth C. Hyerms, MD, MPH;.ld'lcry.P, Stnnswing et al: Hyper endemic streptococcus pyogenes infection despiteprophylaxis with penicillin G Benzathine NE.IM .July I I, I 991, 92- 97.16. WHO statistical index 199- 1995.17. S. Padmavathy: Rheumatic fever and Rheumatic heart disease in India at the turn ofthe centurylndian heart .Journal 2001; 53: 35-37.18. Gregory C. Gray, Dennis C. MC Phate, Maija Leinonen et al.Weekly oral Azithromycin us prophylaxis for agents causing Acute respiratory diseaseCl D 1998: 26 Jan. t 03 --- 110.19. Robert C. Moellering, .IR, MD, Introduction: Revolutionary changes in the Macrolideand Azalide Antibiotics. The Ann.J. Med. Sept.l2, 1991, 91, Suppl. 3A Volume 1991.20. Jerome .1, Schentaz, Pharm D, Charles H, Ballow Pharm.D, Tissue directed,Pharmacokinetics, The Am . .1. Med. Volume 91, (Suppl 3A) 3A- 5S.21. Harold C. New MD, clinical microbiology of Azithromycin. The Am . .1. Med.Volume 9I (Suppl 3A) 3A -- 12S.22. Thomas M. Hooton M.D, A comparison of Azithromycin and penicillin V for thelrcutment of streptococcal pharynigitis. The Am. J. Med. Volume 91 (Suppl. JA) JA-2JS.23. Scott Hopkins M.D, clinical toleration and safety of Azithromycin. The Arn . .1. med.Volume 91 (Suppl 3A) 3A- 40S.24. Ron Dagom et al. an epidemic of penicillin tolerant group A streptococcalpharyngitis in children living in a closed community. Mass treatment with erythromycin.TheJ.Inf.Dis. Volume 156. No.3 Sept.l987514-516.25. Andreas podbielski, Bernard kneikemegcr Commentary. The Lancet. Vol. 358. July7, 2001.2Cl. Goivanni Ghirga M.D et al. Inefficacy of a 3 day course of Azithromycin inpreventing acute rheumatic fever allcr group A streptococcal infection (Scarlet fever) inUll 8 year old child. Letters . .1. of pediatrics. Volume 134, No I -123,- 124.27. G. Shimos, K. Bedevis, I Parasakalia, et al Emergence of group A Beta hemolyticstreptococci resistant to Erythromycin in Athens, Greece.23
28. Bruna Facinclli cl al The Lancet Vol 358.july 7,2001.2
FAMILY STUDY OFFOUR PROBANDS WITH1-IYPERPTROPHIC CARDIOMYOPATHYDUE TODELETION MUTATIONS IN MYH 7 ANDMYBPC3.25
INTRODUCTIONFamilial hypertrophic cardiomyopathy is an inherited autosomal dominant diseasecharacterized by myocardial hypertrophy disproportionate to hemodynamic load {I ).Inappropriate myocardial hypertrophy predominantly involves interventricular septumund anterolateral LV wall in the presence of a non dilated hyperdynamic LV with orwithout L VOT gradient.Hallmark of HCM .is disarray of myofibril and myolibers,usually in excess of 5%, of total myocardium (2). Familial HCM occurs as an autosomaldominant Mendelian inheritance in at least 50% of cases, the rest may be sporadic due tomutations.At least 9 genes are responsible and not less than 125 mutations are(kscribed. Mutation in MHY 7 gene accounts for 30% of described HCM cases (3)Other genes involved are cardiac Troponin .Tin lq 31 in 15%, Alpha Tropomyosin 15q2in 5 1 % myosin binding protein C. II p 13 - q 13 in 10% and rarely ventricular myosinregulatory light chain and ventricular myosin essential light chain in chromosome 12 ()2und 3p respectively. All the mutations identified in Indian patients recently arcunprecedented ( 4). As such, Indian population is ethnically diverse. Ethnical diversitymay be reflected in Indian patients with HCM also. This could very well broaden thescope of genetic and clinical epidemiology of the disease.Recently. more thun onegenetic alteration is reported contributing to severity of disease (5-7).26
In 4 probands, diagnosed to have HCM earlier by clinical evaluation ami curdiaccutheterization, 3 novel delation mutations, E Delta 927 in MYH7 , 25 bp Delta intron32 and CC Delta 453 in MYBPC3 genes were identified. This study aims at identifyingthe profile of entire living members of the families of the probands including manifestdisease, morphologic disease and genotypes.METHODSProbands were registered patients of SCTIMST with the diagnosis of HCM,confirmed by clinical usscssment as well as cardiac catheterization. All living membersof the families underwent a thorough clinical evaluation, ECG and cchocardiography.All patients were genotyped. Inappropriate myocardial hypertrophy in the absence of anobvious cause was tuken as criteria for morphological diagnosis.ECG abnormalitiesnoticed included T wave changes, left ventricular hypertrophy, abnormal Q waves andlcrt atrial enlargement. In order to confirm that the mutations are specific for HCM, I 00individuals without HCM were also screened and genotyped.GENETIC ANALYSISGenetic anulysis of all samples were done at the co-operating study group at MaxPlank Institute in Germany .QIAmP Blood Kits (Quiagen) were used to extruct genomicDNA from EDTA blood samples. Oligonucleotides and annealing temperatures for eachPCR primer was used. Amplified exons were examined for sequence variations by thesingle-strand conformation polymorphism (SSCP) and fluorescence --assisted mismatch27
( FAM) analysis. The SSCP analysis was carried out with 5% glycerol ut both 14 degreeC and 22 degree C.DNA fragments were visualized by silver staining (8). When anabnormal SSCP/FAM pattern was observed, the corresponding amplicon was cloned forsequencing. Sequencing analysis with PCR product in order to identify the exact startposition of the deletion was done. Then blunt-ended PCR products were made by PjitTurbo DNA polymerase (Stratagene), cloned into PCR -Blunt II- Topo vectors(Invitrogen) and then sequenced each allele.Insert lengths ( identicul in I 0 sepurateclones) were confirmed by Eco RI digestion and gel analysis. Double stranded plasmidDNA was obtained using Quiagen Plasmid Midi Kits (Quiagen) and sequenced by meansof using the Dye terminator kit (Amersham Pharmacia Biotech inc) on an ALF expressHcqucncer DNA were washed and hybridized to the sequencing primers for real-timeDNA sequencing using PSQ 96 (Pyrosequencing AB, Uppsala, Sweden). The nucleotidesequence was determined from the single peak in the pyrogram.28
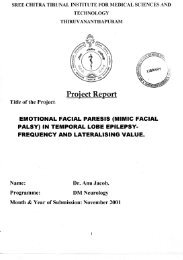
RESULTSThree novel deletion mutations were identified in 2 genes frequently associatedwith HCM in the probands and their families, one in MYH7 and 2 in MYBPC3.Pedigree of all families in 3 generations were plotted. In one family, 2 mutations in the 2different genes were segregating (MM). Four families were, that of MM, HH, MiR andNP.29
Ul:1 01:2 111:3 U1:4111:1 01:2 Hl:3 111:4 Ul:5 111:6111:1Pedigree of all families: Squares and circles indicate male and female members, respectively.Open, closed and slashed symbols indicate unaffected, carrier affected, and deceasedmembers, respectively. Hatched symbols indicate asymptomatic carriers of the mutation. Thearrows point to the proband.Mathimohan (MM) family has two mutations: M: 25 nt deletion in intron 31 in MYBPC3 gene anB refers 3 nt deletion in codon 927 exon 23, MYH7 gene.Micheal Ruban (MiR) family has only one mutation 25 nt deletion in intron 31 in MYBPC3 geneHariharan Family (HH) and Narayanan Pillai family have the same mutation that is, 2 nt deletioin exon 16, codon 453, MYBPC3 gene.30
MM FAMILYProband MM is a 29 year old man (II:6) with clinical onset of disease at the ageof 19 years.He presented with class II DOE, AOE and cxcrtional syncope andpalpitation. An S4 was audible. No murmur. ECG showed no L VH, no Q waves. Tinversion in lead II. Jl(, avF and V6 present.His echo showed asymmetric septalhypertrophy (A SH) mild MR and systolic anterior movement of anterior mitral leaflet(SAM). No L VOTO was present. IVS measured 23/27 and posterior wall 13/20. LVdiastolic dysfunction was present.Cardiac catheterization contirmcd non-obstructiveHCM. His genetic analysis showed presence ofMYH7 mutation.Father of the index patient (1:1) and one younger brother (11:7) had sudden cardiac death(SCD). 1:1 was symptomatic by age 40 with chest pain. SCD occurred at age 52, nofurther details available.11:7 was symptomatic from 16 years of age with dysponea on effort and presyncope,had SCD at 20 years of age.I :2, mother of proband is 65 years old, has class II DOE, and palpitation. She haseffort related syncope lor the last 4 years. S4 was audible. ECG showed no LVI-I, TWave flattening in avL, VI, V4,- V6 were present. ECG showed mild concentric LVI-I,no SAM, no MR, No LVOTO. Genetic analysis showed MYBPC 3 mutation.II: 1 is a 45 years old female, symptomatic from 43 years of age with DOE class II andatypical chest pain. ECG showed no LVH. T wave flattening in avL present. ECHOshowed mild concentric L VH. No MR, No SAM, No LVOTO. She is on Beta blockerlor stage IHBP. Her genetic analysis showed MYBPC mutation.31
11:2 is a 40 year old lady, symptomatic for one year with DOE class II, has no anginaor syncope. ECG showed QRS axis of- 30, incomplete LBBB pattern, no LVH, T waveinversion in V6. Echo showed ASH (IVS 18/18, PW 19/17). Moderate MR, no SAM, noLVOTO. She is on Beta blocker. Genetic analysis showed MYH7 mutation.II: 3 is a 38 year old lady, genetically carrier for MYBPC intron 3 mutation.II: 4 is a 36 year old man, genetically a carrier of MYPC intron 3 mutation.11:5 is a 32 year old lady, symptomatic for the last 15 years with class III AOE, DOE.S4 audible. ECG showed LVH, T inversion in L II, III avF and V6. ECHO showedsevere ASH (JVS 21/25, PW12/14) mildly dilated LA, mild MR. LVOT gradient of35mm Hg at rest. SAM+. LV diastolic dysfunction present. Patient is on Beta blocker.She has both mutations- MYH7 and MYBPC3.Ill: 1 is 17 year old son of Il:2 symptomatic from 13 years of age with DOE class ll withhistory of single episode of syncope.ECG showed L VH by voltage, incomplete inRBBB. T inversion in L II, III, avF, V4 V5, V6. ECHO showed mild concentric LVH,mildly increased cchogenicity of IVS, AW, LW. Mitral e>a. No MR, no SAM, noLVOTO.Ill :2 is 13 year old daughter of 11:2 genetically normal. She has history offever ut the age of 4 years and is on penicillin prophylaxis. Genetic analysismutations.Ill :3 is 7 years old daughter of 11:4, genetically normal.Ill :4 is 9 year old son of 11:5, has atypical chest pain since 7 years ofnormal. ECG showed LVH by voltage. T inversion in VI V2Echo showed no evidence of HCM. He has MYH7 mutation.32
MM family has 12 genetically related individuals.2 sudden cardiacdeaths occurred in this family. There are 7 patients with disease and 2 who arc carriers.Proband has class II symptoms and one mutation in MYH 7. Beta myosin heavy chainmutation was seen in 4 more patients. None with this mutation failed to express diseuse.Myosin binding protein C mutation was seen in 2 patients and 2 are carriers. One patienthad both mutations and was most severely symptomatic.Mil~ Ji'AMILY:Proband (l:l ) is 67 year old, symptomatic for 10 years with palpitation andAOE(from age 57. He has no angina or syncope. Patient has atypical burning chest pain.Clinically S4 present. No murmur. ECG showed a QRS axis of+ 30, LVH, T inversionin Ll, LII, avL V2 - V6. Echo showed concentric LVH, mild MR, no SAM, severediastolic LV dysfunction, no L VOTO. His TMT was mildly positive in 1996. Cathshowed increased LV filling pressure, and CAG showed mid LAD bridge.Geneticanalysis showed 25 hp delta intron 32 mutation of MYBPC3.1:2, wife of proband MiR is normal.II: I is MiR's brother's daughter, 51 year old asymptomatic lady; clinically normal, hasno ECG change, echo showed mild concentric LVH, no SAM, no MR and no LVOTO.She has MYBPC3 mutation.II :2 is a 40 year old, normal.11:3 is a 36 year old lady, asymptomatic carrier.11:4 is a 23 year old lady, asymptomatic carrier.33
Ill: I is the 19 year old daughter of I I :2. she is normal.Fldcr borthcr and both parents of proband died at their old age, cause of death is notknown. Only the proband is symptomatic. Other affected (II:I) patient has only mildconcentric LVH by echo and is asymptomatic at 51 years. Carries are all past 20 years.This mutation in their family is behaving in a similar manner compared to MM family -late onset and relatively benign course. (Reduced penetrance until 6 1 h decade of life).HH FAMILY & NJ> FAMILYHH and NP families had mutations in exon of MYBPC 3.l-Ienee they arepresented together.IIH FAMILYProband of HH family (ll:2) is a 40year old man who presented with clinicalonset of disease ut the age of 31. He has DOE class II and palpitation. His parents haddied at young age due to non-cardiac problems. (Father died of pulmonary tuberculosisat the age of 46 and mother of pneumonia at the age of 37). They had no known cardiacproblems. Clinically he has audible S4, no murmur. ECG showed QRS axis +W, LVI-I,LAE and T inversion in lead avL V5, V6. ECHO showed asymmetric septal hypertrophy(IVS 17/24, PW 9115), mild LA enlargement, mild SAM and no LVOT gradient. Mid,basal IVS, apex and apicolatcral wall arc involved. He has LV diastolic dysfunction.Cuth done in 1993 showed elevated LV filling pressure, no gradient at rest, but a gradientui'J5 mm of hg on isoprenaline Genetic analysis showed mutation.34
If:( is a 46 year old man, having class II angina and stage II hypertension. His ECGshowed T wave changes, no LVH. Echo was normal. He has mutant gene. CAD is notruled out.11:3 is a 38 year old lady, normal.11:4 is a 37 year old man, symptomatic from 34 years of age. Clinically normal. ECGshowed LYH by voltugc, T waves changes and abnormal Q waves. Echo shoed no LVH,no SAM, No MR, No LVOTO. However echo suggested increased echogenicityof' fVS.I fc has mutation by genetic analysis. Patient is on Beta blocker.11:5 is 34 year old man, smoker and alcoholic, is asymptomatic. He is clinically normal.ECG showed Q in V3, T inversion in aVL and no LVH. Echo showed mild concentricL VH. No SAH no MR, & no LVOTO. Mid JVS is hyperechoeic. Patient is on Betablocker. He has mutation.Ill: 1 is 15 year old son off I: 1, normal.Ill :2 is 16 year old daughter of II: 1, clinically normal. She is carrier.11:3 is 13 year old son of lf:2, nomml.Ill :4 is 11 year old daughter of II:2 she is a carrier.I II: 5 and llf :6 arc normal. Parent II :3 is also genetically normal.No SCD occurred in HH family.There arc 4 patient with morphologic HCM. Two are carriers. Afnicted patients arebeyond 30 years of age and arc only mildly symptomatic, indicating a less severe form ofdisease.35
Nl, FAMILYProband (11:8) is a 54 year old man with clinical onset of disease at th ugc of 40with class II angina, , dysponoea and pre-syncope. His halter showed VPC's and NSVT.Clinically he had cardiac enlargement, palpable S:4 and 3/6 dynamic LVOT murmur.ECG showed LVII, LAE, T inversion in LI, aVL, V4- V6 and Q in aVL. Echo showedasymmetric septal hypertrophy (IVS 19/26, PW 10/21) SAM, mild to moderate MR andL VOT gradient of 45mm Hg.His cardiac catheterization showed bisferiens aortictrueing, septal hypertrophy and SAM. L VEDP was 28 mm Hg.He had an RVOTgradient of lOmm Hg, a Waves were prominent in JVP. Coronaries were normal. He isun Atcnolol and Amiodarone.I: I father of proband died at the age of 76, cause of death is not known.I :2 ;mother of proband ;died at the age of 72, was not known to have heart disease.II: 1 had SCD at age 72, no further details available.11:2 is a 72 year old man ,normal. No mutation.II :3 had SCD at the age of 43. He was known to have heart disease, but no furtherdetails are available.II :4 had SCD at age 55. No details available.11:5 had SCD at 52 years of age. He was known to have heart disease, hut no furtherdetails available.II:(, is a 59 year old lady, has stage I HBP, normal.11:7 is the twin sister of proband ,is normal.Ill: I 31 year old daughter of II :2 ,normal.111:2 47 year old son of 11:3, normal.36
111:3 42 year old son of 11:3, symptomatic for 15 years with DOE class II: and presyncope. He is clinically normaL ECG showed ST-T changes. No LVH.ECHO showedmild AML and PML prolapse, mild MR. No LVOTO or SAM. Genetically, he hasmutation.111:4 is 42 year old son ofll:3, smoker and alcoholic has history ofrheumatic chorea atthe age of 10 years. He is clinically nom1al. ECG is normal. ECHO showed mild MR,AR and MS and TR. No SAM or L VOTO. He is a carrier of mutation.111:5 is 32 year old daughter of II:4. She is a carrier.I 11:6 29 year old daughter of 11:4, Normal.111:7 40 year old son of II:5, has DOE class II, and atypical chest pain. Clinically normaLI Ius LVH, LAE, normal Q waves and T inversion in Ll, avL V4 to V6 in ECG.ECHO showed asymmetric septal hypertrophy (IVS 35/44, PW 13/19), SAM, Mod. MRnnd L VOT gradient of 30. He has mutation.II I: 8 is 22 year old duughter of II :6; normal.In N.P family, 4 SCD occurred, all beyond 5 1 h decade. Disease onset was about 30 yearsin all. 2 patients had signi flcant ASH with LVOTO. 4 cases of SCD arc likely to beobligate carriers.37
DISCUSSION7/22 patients (77.3%) had DOE, 6/22 (27.3%) have angina, SCD occurred 6/22(27.3'Yt•) 6/16 had ASH (27.3%). SAM was seen in 5/16.(31.3%). All patients hadabnormal ECG. Q waves in 11/16 (67%) ST-T changes were universal, 11/16 had LVH .(67%). rn the established literature, 90% patients with HCM have DOE, 75 %·_hasungina, associated CAD is seen in 20% of older patients. AR is seen in 10%( Only oneputient had AR in this study). Normal Echo is found only in 25%. ECG is reportedabnormal in almost all, especially those with LVOTO. Most frequent finding is ST -- Tchanges. Abnormal Q wave are seen in 20-50% (22)In MM family 2 separate mutations of MYBPC and Beta MYH7 are segregating.Either mutation is associated with different degrees of HCM severity in same family.HCM resulting from Beta MYH7 gene is more severe than MYBPC 3 mutation. Diseasepcnetranee was complete in all Beta MYH7 mutation at E delta 927. All patients withthis mutation were symptomatic before the age of20. All adults but one had ASH, allhad L VH, and T wuve chunges in ECG, 2 had SAM, 3 had MR, 2 had syncope andungina.The E Delta 927 deletion maps to the rod region which appears to harbor frequentlyHCM -- related point mutations. 12-15. Deletion of glutamic acid at the codon 927 doesnot altered a diagnostic restriction site or followed coding sequences. The aftectedamino acids correspond (or lie adjacent) to the B- MHC head-tail junction 16 and may becritical for the flexibility of this region implicated in force transmission to the thickfilmnent 17, 18. It becomes evident that a one amino acid deletion like E detla 927 leads38-~--------------------
to u frame shin in the heptad repeat pattern. Assuming that the deleted allele is expressedin the myocardium, it is tempting to speculate that the mutation interferes with normalheart muscle set up at the level of MHC dimerization. Abnormal dimerization leads to aless rigid rod and therefore an impaired transmission of the force generated in the myosinhead. Considering it's disruptive nature, E delta 927 mutation is the molecular cause forthe serious type of HCM observed in the proband's family. The glutamic acid in thisposition has been highly conserved phylogenetically in myosin genes from dictylosteiodato man, suggesting an important role for the function of the protein.Second mutation seen in same family was in MYBPC3 in the intron 32. Thisleads to disruption to inability of MYBPC to incorporate into sarcomere at A bands.Patients are less symptomatic and onset clinically was beyond 40 years of age. All adultswith the mutation had LVH. MR was seen in one patient, none had SAM. Echo wise,LVH was concentric in all. All had DOE and history of syncope was present in. onlyone, oCCUlTing at an age beyond 60years. Penetrance is only 50 1 %. In general, thismutation is not expressed at middle age. Delayed expression of disease and favorableoutcome may hinder recognition of heritable nature of mutation in MYBPC3.The patient who had both the mutation is significantly symptomatic. She hasMR, LVOTO, SAM and LV diastolic dysfunction with Cl. III AO E, DOE.ASH,Here;mutation is likely to be additive. This study is in agreement with the conclusion thatdisease expression is more pronounced in patients who had two mutation (6), one inBeta MYHC and other in MYBPC gene. Such a constellation has been reported once inthe literature. ( 7) Similarly until now ;only two compound heterozygous for mutationsin MYH7 gene have been described (5, 6) finding support to the notion that HCM may39
esult from complex inheritance patterns.It is probable that the younger brother ofproband who had SCD at the age of 19, had both the mutation, where as his father whohad SCD at the age 52 had only MYH7 E delta 927 mutation, since mother doesn't havethis mutation and 3 of her children have.ln NP and HH family, deletion mutation m Exon 16 of MYBPC3 was seen.Families are unrelated.They showed characteristic phenotype features of MYBPCmutation. Penetrance was delayed until 4-5 1 h decade of life and disease is milder. Due tothe deletion of two nucleotides in codon 453, predicted premature termination occurred incodon 473 to produce truncated protein without the terminal domain 19, which binds totitin and myocin. The mutation in NP family seems to be associated with a particularphenotype. Hence patients have a malignant history of SCD at 5 111 and 6 111 decade. HigherIVS thickness is seen in symptomatic patients of this family though the disease on set isdeluycd compared to MYH7 mutations. Fatalities were not less.As expected with most autosomal diseases in HH family, the same mutation is running arelatively benign course.It should also bo remembered that risk of SCD do not correlate well with morphology,but with early onset disease, family history of SCD and abnormal exercisehcmodynamics(22).Molecular mechanism of the mutation is not very clear. The study supports that all thegenes involved in the development of HCM should probably be tested even if a particularphenotype is observed (20).40
AcknowledgementsI am indebted to the members of the family of MM, MiR, HH and NP who generouslycooperated in this study.Study was a co-operative project of HCM withMux Plank institute for physiological and clinical research, Department of ExperimentalCardiology,Benekcstr.2,D-6123 Bad Nauheim, Germany.Service de Biochimie B, U 523 INSERM, Institute de Myologic, Batiment Babinski,Hospital de Ia salpetriere, Paris, France.Department of Biochemistry, Center for For Advaned studies in functional Genomics,School of Biological Studies ,Madurai Kamaraj University,Madurai.-695 011, India.Department of cardiology Sree Chitra Tirunal Institute For Medical Sciences AndTechnology. Trivandrum India.41
ReferencesI. WATKINS H, SEIDMAN JG, SEIDMAN CE. Familial hypertrophic cardiomyopathy:u genetic model of cardiac hypertrophy. Hum Mol Genet 1995; 4:1721-1727.2. BLAIR E, REDWOOD C, ASHRAFIAN H, OLIVERIA M, BROXHOLME J, KERRB, SALMON A, OSTMANN-SMITH I, WATKINS H. Mutations in they2 subunit ofAMP-activated protein kinase cause familial hypertrophic cardiomyopathy: evidence forthe central role of energy compromise in disease pathogenesis. Hum Mol Genet 2001;10(1): 1215-1220. .3. DALLOZ F, OSJNSKA HAND ROBBINS J. Manipulating the contractile apparatus:genetically defined animal models of cardiovascular disease. J Mol Cell Cardiol200 I;33:9-25.4. SAKTHIVEL S, JOSEPH PK, RAJAMANICKAM C, VOSBERG HP. A novelmissense mutation (712Arg-Leu) in the cardiac B-myosin heavy chain gene causinghypertrophic cardiomyopathy in an indian family. Hum Mutat 1999; 15: 298-299.5. NISHI H, KIMURA A, HARADA H, KOGA Y, ADACHI K, MATSUYAMA K,KOYANAGI T, Y ASUNAGA S, IMAIZUMI T, TOSHIMA H, SASAZUKI T. Amyosin missense mutation, not a nuiJ allele, causes familial hypertrophiccurdiomyopathy. Circulation 1995; 91: 2911-2915.6. JESCHKE B, UHL K, WEIST B, SCHRODER D, MEITINGER T, DOHLEMANN C,VOSBERG HP. A high risk ofhypertrophic cardiomyopathy associated with a compound·genotype of two mutated B-myosin heavy chain genes. Hum Genet 1 998; I 02:299-304.7. RICHARD P, ISNARD R, CARRIER L, DUBOURG 0, DONATIEN Y, MATH lEUB, BONNE G, GARY F, CHARRON P, HAGEGE A, KOMAJDA M, SCHWARTZ KAND HAINQUE B. Double heterozygosity for mutations in the B-myosin heavy chainand in the cardiac myosin binding protein-C genes in a family with hypertrophiccardiomyopathy . .I Med Genet 1999: 36: 542-545.8. OR ITA M, IWAHANA H, KANAZA W A H, HAY ASH! K AND SEKJY AT.Detection ofpolymorphisms of human DNA by gel electrophoresis as single-strandconformation polymorphisms. Proc Nat/ A cad Sci USA 1989; 86: 2766-2770.9. VERPY E, BIASOTTO M, MEO T, TOSI M. Efficient detection of point mutations oncolor-coded strands of target DNA. Proc Nat/ A cad Sci USA 1994; 91: 1873-7.I 0. VERPY E, BIASOTTO M, BRAI M, MISIANO G, MEO T, TOSI M. Exhaustivemutation scanning by fluorescence-assisted mismatch analysis discloses new genotypephenotypecorrelations in angiodema [see comments]. Am J Hum Genet 1996; 59: 308-19.42
11. RONAGHJ, M eta/., ( 1996) Real-time DNA sequencing using detection ofpyrophosphate release. Anal Biochem 242:84-89.12. SAKTHIVEL S, VOSBERG H-P, RAJAMANICKAM C. Oligonucleotide ligationassay for rapid and sensitive identification of carriers of a missense mutation in thecardiac B-myosin heavy chain gene causing hypertrophic cardiomyopathy in an Indianfamily. Current Science 2000; 12(80): 1588-1592.13. EPSTEIN NO, COHN GM, CYRAN F, FANANAPAZIR L. Differences in clinicalexpression of hypertriophic cardiomyopathy associated with two distinct mutations in theU-myosin heavy chain gene. A 908 Leu-Val mutation and a 403 Arg-Gin mutation.Circulation 1992; 86: 345-352.14. WATKINS H, ROSENZWEIG A, HWANG DS, LEVIT, MCKENNA W,SEIDMAN CE, SEIDMAN JG. Characteristics and prognostic implications of myosinmissense mutations in familial hypertrophic cardiomyopathy. N Eng! J Med 1992; 32!-i:1108-1114.t 5. WATKINS H, ROSENZWEIG A, HWANG DS, LEVI T, MCKENNA W,SEIDMAN CE, SEIDMAN JG. Characteristics and prognostic implications of myosinmissense mutations in familial hypertrophic cardiomyopathy [see comments]. N Engl.!Med 1992; 326: 1108-14.16. NISHI H, KIMURA A, HARADA H, ADACHI K, KOGA Y, SASAZUKI T,TSHIMA H. Possible gene dose effect of a mutant cardiac B-myosin heavy chain gene onthe clinical expression of familial hypertrophic cardiomyopathy. Biochem Biophys ResCommun 1994; 200: 549-556.17. RIMM DL, SINARD JH, POLLARD TD. Location of the head-tail junction ofmyosin. J Cell Bioi 1989; 108: 1783-9.18. RAYMENT l, HOLDEN HM, SELLERS JR, FANANAPAZIR L, EPSTEIN NO.Structural interpretation of the mutations in the B-cardiac myosin that have beenimplicated in familial hypertrophic cardiomyopathy. Proc Nat/ Acad Sci USA 1995; 92:3864-3868.19. KNIGHT P J. Dynamic behaviour of the head-tail junction of myosin. J Mol Bioi1996; 255: 269-74.20. CARRIER L, BONNE G, BAHREND E, ET AL. Organization and sequence ofhuman cardiac myosin binding protein C gene (MYBPC3) and identification of mutationspredicted to produce truncated proteins in familial hypertrophic cardiomyopathy.Circulation Res 1997; 80: 427-434.21. RICHARD P, CHARRON P, CHRISTOPHEL, LECLERCQ C, LEDEUIL C,CARRIER L, DUBOURG 0, DESNOS M, BOUHOUR J-B, SCHWARTZ K,DAUBERT C, KOMAJDA M, HAINQUE B. Homozygotes for a R869G mutation in the43
13-myosin heavy chain gene have a severe fonn of familial hypertrophic cardiomyopathy.J Mol Cell Cardiol. 2000; 32: 1575-1583.44