Conference programme pdf, 5.68Mb - World Health Organization
Conference programme pdf, 5.68Mb - World Health Organization
Conference programme pdf, 5.68Mb - World Health Organization
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Thursday 15 th September 2011<br />
12<br />
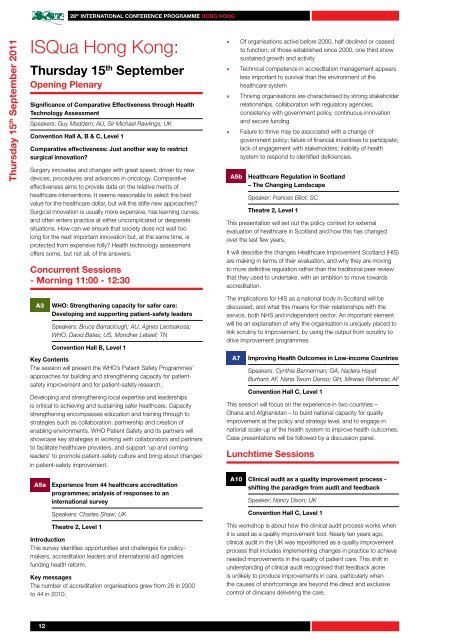
28 th InTErnaTIonal ConfErEnCE ProgrammE Hong Kong<br />
ISQua Hong Kong:<br />
Thursday 15 th September<br />
opening Plenary<br />
Significance of Comparative Effectiveness through <strong>Health</strong><br />
Technology assessment<br />
Speakers: Guy Maddern; AU, Sir Michael Rawlings; UK<br />
Convention Hall a, B & C, level 1<br />
Comparative effectiveness: Just another way to restrict<br />
surgical innovation?<br />
Surgery innovates and changes with great speed, driven by new<br />
devices, procedures and advances in oncology. Comparative<br />
effectiveness aims to provide data on the relative merits of<br />
healthcare interventions. It seems reasonable to select the best<br />
value for the healthcare dollar, but will this stifle new approaches?<br />
Surgical innovation is usually more expensive, has learning curves,<br />
and often enters practice at either uncomplicated or desperate<br />
situations. How can we ensure that society does not wait too<br />
long for the next important innovation but, at the same time, is<br />
protected from expensive folly? <strong>Health</strong> technology assessment<br />
offers some, but not all, of the answers.<br />
Concurrent Sessions<br />
- morning 11:00 - 12:30<br />
A3 WHo: Strengthening capacity for safer care:<br />
Developing and supporting patient-safety leaders<br />
Speakers: Bruce Barraclough; AU, Agnes Leotsakosa;<br />
WHO, David Bates; US, Mondher Letaief; TN<br />
Convention Hall B, level 1<br />
Key Contents<br />
The session will present the WHO’s Patient Safety Programmes’<br />
approaches for building and strengthening capacity for patientsafety<br />
improvement and for patient-safety research.<br />
Developing and strengthening local expertise and leaderships<br />
is critical to achieving and sustaining safer healthcare. Capacity<br />
strengthening encompasses education and training through to<br />
strategies such as collaboration, partnership and creation of<br />
enabling environments. WHO Patient Safety and its partners will<br />
showcase key strategies in working with collaborators and partners<br />
to facilitate healthcare providers, and support ‘up and coming<br />
leaders’ to promote patient-safety culture and bring about changes<br />
in patient-safety improvement.<br />
A5a Experience from 44 healthcare accreditation<br />
<strong>programme</strong>s; analysis of responses to an<br />
international survey<br />
Speakers: Charles Shaw; UK<br />
Theatre 2, level 1<br />
Introduction<br />
This survey identifies opportunities and challenges for policymakers,<br />
accreditation leaders and international aid agencies<br />
funding health reform.<br />
Key messages<br />
The number of accreditation organisations grew from 26 in 2000<br />
to 44 in 2010.<br />
» Of organisations active before 2000, half declined or ceased<br />
to function; of those established since 2000, one third show<br />
sustained growth and activity<br />
» Technical competence in accreditation management appears<br />
less important to survival than the environment of the<br />
healthcare system<br />
» Thriving organisations are characterised by strong stakeholder<br />
relationships, collaboration with regulatory agencies,<br />
consistency with government policy, continuous innovation<br />
and secure funding<br />
» Failure to thrive may be associated with a change of<br />
government policy; failure of financial incentives to participate;<br />
lack of engagement with stakeholders; inability of health<br />
system to respond to identified deficiencies.<br />
A5b <strong>Health</strong>care regulation in Scotland<br />
– The Changing landscape<br />
Speaker: Frances Elliot; SC<br />
Theatre 2, level 1<br />
This presentation will set out the policy context for external<br />
evaluation of healthcare in Scotland and how this has changed<br />
over the last few years.<br />
It will describe the changes <strong>Health</strong>care Improvement Scotland (HIS)<br />
are making in terms of their evaluation, and why they are moving<br />
to more definitive regulation rather than the traditional peer review<br />
that they used to undertake, with an ambition to move towards<br />
accreditation.<br />
The implications for HIS as a national body in Scotland will be<br />
discussed, and what this means for their relationships with the<br />
service, both NHS and independent sector. An important element<br />
will be an explanation of why the organisation is uniquely placed to<br />
link scrutiny to improvement, by using the output from scrutiny to<br />
drive improvement <strong>programme</strong>s.<br />
A7 Improving <strong>Health</strong> outcomes in low-income Countries<br />
Speakers: Cynthia Bannerman; GA, Nadera Hayat<br />
Burhani; AF, Nana Twum Danso; GH, Mirwais Rahimzai; AF<br />
Convention Hall C, level 1<br />
This session will focus on the experience in two countries –<br />
Ghana and Afghanistan – to build national capacity for quality<br />
improvement at the policy and strategy level, and to engage in<br />
national scale-up of the health system to improve health outcomes.<br />
Case presentations will be followed by a discussion panel.<br />
lunchtime Sessions<br />
A10 Clinical audit as a quality improvement process -<br />
shifting the paradigm from audit and feedback<br />
Speaker: Nancy Dixon; UK<br />
Convention Hall C, level 1<br />
This workshop is about how the clinical audit process works when<br />
it is used as a quality improvement tool. Nearly ten years ago,<br />
clinical audit in the UK was repositioned as a quality improvement<br />
process that includes implementing changes in practice to achieve<br />
needed improvements in the quality of patient care. This shift in<br />
understanding of clinical audit recognised that feedback alone<br />
is unlikely to produce improvements in care, particularly when<br />
the causes of shortcomings are beyond the direct and exclusive<br />
control of clinicians delivering the care.