E-brochure - Online Guide
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
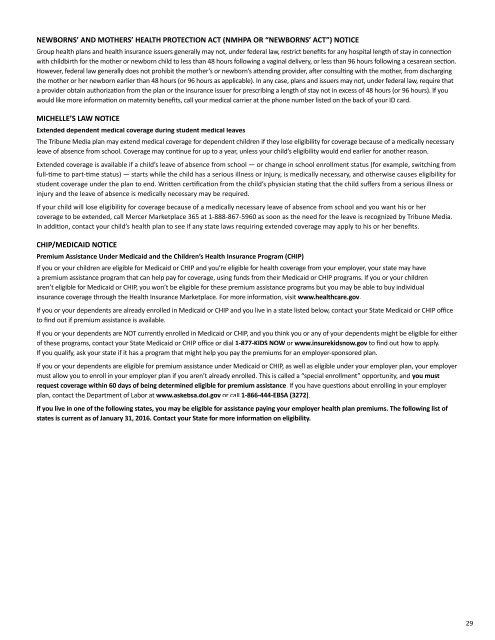
NEWBORNS’ AND MOTHERS’ HEALTH PROTECTION ACT (NMHPA OR “NEWBORNS’ ACT”) NOTICE<br />
Group health plans and health insurance issuers generally may not, under federal law, restrict benefits for any hospital length of stay in connection<br />
with childbirth for the mother or newborn child to less than 48 hours following a vaginal delivery, or less than 96 hours following a cesarean section.<br />
However, federal law generally does not prohibit the mother’s or newborn’s attending provider, after consulting with the mother, from discharging<br />
the mother or her newborn earlier than 48 hours (or 96 hours as applicable). In any case, plans and issuers may not, under federal law, require that<br />
a provider obtain authorization from the plan or the insurance issuer for prescribing a length of stay not in excess of 48 hours (or 96 hours). If you<br />
would like more information on maternity benefits, call your medical carrier at the phone number listed on the back of your ID card.<br />
MICHELLE’S LAW NOTICE<br />
Extended dependent medical coverage during student medical leaves<br />
The Tribune Media plan may extend medical coverage for dependent children if they lose eligibility for coverage because of a medically necessary<br />
leave of absence from school. Coverage may continue for up to a year, unless your child’s eligibility would end earlier for another reason.<br />
Extended coverage is available if a child’s leave of absence from school — or change in school enrollment status (for example, switching from<br />
full-time to part-time status) — starts while the child has a serious illness or injury, is medically necessary, and otherwise causes eligibility for<br />
student coverage under the plan to end. Written certification from the child’s physician stating that the child suffers from a serious illness or<br />
injury and the leave of absence is medically necessary may be required.<br />
If your child will lose eligibility for coverage because of a medically necessary leave of absence from school and you want his or her<br />
coverage to be extended, call Mercer Marketplace 365 at 1-888-867-5960 as soon as the need for the leave is recognized by Tribune Media.<br />
In addition, contact your child’s health plan to see if any state laws requiring extended coverage may apply to his or her benefits.<br />
CHIP/MEDICAID NOTICE<br />
Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP)<br />
If you or your children are eligible for Medicaid or CHIP and you’re eligible for health coverage from your employer, your state may have<br />
a premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP programs. If you or your children<br />
aren’t eligible for Medicaid or CHIP, you won’t be eligible for these premium assistance programs but you may be able to buy individual<br />
insurance coverage through the Health Insurance Marketplace. For more information, visit www.healthcare.gov.<br />
If you or your dependents are already enrolled in Medicaid or CHIP and you live in a state listed below, contact your State Medicaid or CHIP office<br />
to find out if premium assistance is available.<br />
If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and you think you or any of your dependents might be eligible for either<br />
of these programs, contact your State Medicaid or CHIP office or dial 1-877-KIDS NOW or www.insurekidsnow.gov to find out how to apply.<br />
If you qualify, ask your state if it has a program that might help you pay the premiums for an employer-sponsored plan.<br />
If you or your dependents are eligible for premium assistance under Medicaid or CHIP, as well as eligible under your employer plan, your employer<br />
must allow you to enroll in your employer plan if you aren’t already enrolled. This is called a “special enrollment” opportunity, and you must<br />
request coverage within 60 days of being determined eligible for premium assistance. If you have questions about enrolling in your employer<br />
plan, contact the Department of Labor at www.askebsa.dol.gov or call 1-866-444-EBSA (3272).<br />
If you live in one of the following states, you may be eligible for assistance paying your employer health plan premiums. The following list of<br />
states is current as of January 31, 2016. Contact your State for more information on eligibility.<br />
29