Nov 2016
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Choroidal melanoma: a spotter’s guide<br />
BY PETER HADDEN*<br />
There are not many truly life-threatening<br />
ocular conditions, but choroidal melanoma<br />
is certainly one of them. Overall, about 50%<br />
of people diagnosed with it will, in the fullness<br />
of time, die from it, so one can certainly say that<br />
it is something no one wants to miss. Missing it<br />
has been the subject of lawsuits in the USA and,<br />
even in New Zealand, this diagnosis has graced<br />
the adverse comments section of our Health and<br />
Disability Commission, wondering if “x failed to<br />
provide services with reasonable care and skill…”.<br />
Luckily, that happened 16 years ago (before my<br />
time, may I add!), but we certainly don’t want it to<br />
come up again. So how can we avoid that?<br />
Obviously the first step is not to miss the<br />
diagnosis. Unfortunately, although melanoma is<br />
rare, naevi are not and sometimes the differences<br />
can be subtle. Furthermore, the only time when<br />
maybe we might be able to make a difference to<br />
the prognosis, ie. reduce the risk of metastatic<br />
disease in the future, is if we can catch and treat<br />
melanomas when they’re small, which of course is<br />
when they are most easily confused for naevi.<br />
One study found that, for small indeterminate<br />
pigmented tumours, ie. ones that might be<br />
naevi or might be melanoma, there was a 5%<br />
cumulative chance of metastatic death for<br />
each of the following risk factors: margin at the<br />
disc, lipofuscin, symptoms and subretinal fluid.<br />
Therefore if you’ve got all four there’s a 20%<br />
chance you’ll be dead in a few years.<br />
Some bright spark then came up with a<br />
mnemonic to help people remember what to look<br />
for if you think you’ve seen a naevus but don’t<br />
want to miss a small melanoma (small being less<br />
than 2.5mm thick). That mnemonic is “To find<br />
small ocular melanoma”. This stands for thickness,<br />
fluid, symptoms, orange pigment and margin at<br />
the disc. Naturally of course others subsequently<br />
pointed out that this didn’t really cover everything;<br />
ophthalmologists routinely do an ultrasound<br />
(B-scan) on all such lesions and therefore we<br />
routinely add two letters to this, looking for<br />
hypoechogenicity and characteristic shapes (as<br />
well as the thickness, which ultrasound is very<br />
good at measuring). Then of course, documented<br />
growth is another risk factor. Fortunately many<br />
of you probably don’t have ultrasound anyway so<br />
you don’t have to remember those two letters, but<br />
do remember to look at old photos to see if it has<br />
changed.<br />
It might be helpful at this juncture to go over<br />
what each of these “suspicious features” actually<br />
are:<br />
T is for thickness<br />
If it’s more than 2mm thick, that’s a bad sign. This<br />
suspicious feature actually is best appreciated by<br />
ultrasound, since on ultrasound you can measure it<br />
very easily, as previously mentioned. But if you’ve<br />
got OCT, you can switch on “enhanced depth<br />
imaging” (EDI) or push the OCT machine forward<br />
so that the image flips and you can get a pretty<br />
image of the choroid and usually you can measure<br />
the thickness of the tumour on this, but only if it’s<br />
less than about 1mm thick.<br />
F is for fluid<br />
Subretinal fluid is a danger sign. Naevi can often<br />
have a bit of fluid over the top of them, which<br />
doesn’t matter, but if it’s leaking fluid around it,<br />
that’s bad (unless of course it’s from something<br />
else, like a choroidal neovascular membrane, which<br />
you can get with naevi). Often you can see this<br />
around the tumour or, if you get the patient to look<br />
down, you might notice an inferior serous retinal<br />
detachment. However, even a small bit of fluid is<br />
important to spot and so if you’ve got a camera,<br />
try putting it on autofluorescence; if it’s leaking<br />
fluid, this will show up white beside the tumour.<br />
OCT of course also comes in handy here, as it will<br />
show fluid directly.<br />
S is for symptoms<br />
If your patient has an itchy eye, that’s a symptom<br />
but it really doesn’t have anything to do with<br />
whether there’s a naevus or melanoma in the<br />
fluid. Pain doesn’t matter either (unless it’s huge,<br />
melanoma is not associated with pain, and most<br />
people would suspect that something’s amiss if<br />
you have a really massive melanoma that takes up<br />
the whole eye. The symptoms that really matter<br />
are visual loss (not attributable to some other<br />
cause, of course), field loss or flashes. The flashes<br />
that you get with melanoma are different from the<br />
Moore’s lightening streaks of vitreoretinal traction.<br />
They tend to last longer, maybe a few minutes,<br />
move slowly around, sometimes in circular<br />
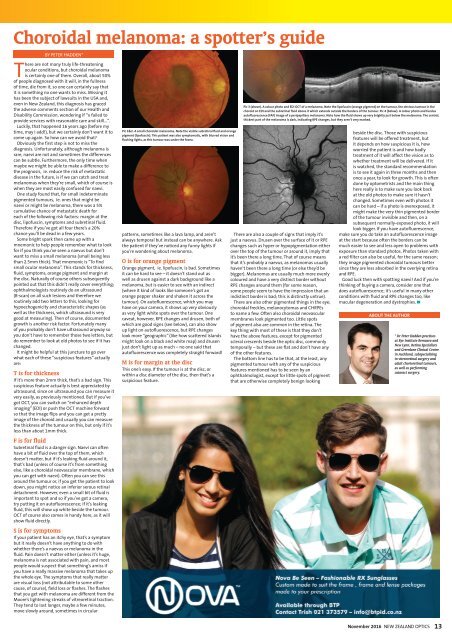
Pic 1&2. A small choroidal melanoma. Note the visible subretinal fluid and orange<br />
pigment (lipofuscin). This patient was also symptomatic, with blurred vision and<br />
flashing lights, as this tumour was under the fovea.<br />
patterns, sometimes like a lava lamp, and aren’t<br />
always temporal but instead can be anywhere. Ask<br />
the patient if they’ve noticed any funny lights if<br />
you’re wondering about melanoma.<br />
O is for orange pigment<br />
Orange pigment, ie. lipofuscin, is bad. Sometimes<br />
it can be hard to see – it doesn’t stand out as<br />
well as drusen against a dark background like a<br />
melanoma, but is easier to see with an indirect<br />
(where it kind of looks like someone’s got an<br />
orange pepper shaker and shaken it across the<br />
tumour). On autofluorescence, which you may<br />
have on your camera, it shows up very obviously<br />
as very light white spots over the tumour. One<br />
caveat, however, RPE changes and drusen, both of<br />
which are good signs (see below), can also show<br />
up light on autofluorescence, but RPE changes<br />
look more “geographic” (like how scattered islands<br />
might look on a black and white map) and drusen<br />
just don’t light up as much – no one said that<br />
autofluorescence was completely straight forward!<br />
M is for margin at the disc<br />
This one’s easy. If the tumour is at the disc, or<br />
within a disc diameter of the disc, then that’s a<br />
suspicious feature.<br />
Pic 3 (above). A colour photo and EDI OCT of a melanoma. Note the lipofuscin (orange pigment) on the tumour, the obvious tumour in the<br />
choroid on EDI and the subretinal fluid above it which extends outside the borders of the tumour. Pic 4 (below). A colour photo and fundus<br />
autofluorescence (FAF) image of a peripapillary melanoma. Note how the fluid shows up very brightly just below the melanoma. The central,<br />
thickest part of the melanoma is dark, indicating RPE changes, but they aren’t very marked.<br />
There are also a couple of signs that imply it’s<br />
just a naevus. Drusen over the surface of it or RPE<br />
changes such as hyper or hypopigmentation either<br />
over the top of the tumour or around it, imply that<br />
it’s been there a long time. That of course means<br />
that it’s probably a naevus, as melanomas usually<br />
haven’t been there a long time (or else they’d be<br />
bigger). Melanomas are usually much more evenly<br />
coloured and have a very distinct border without<br />
RPE changes around them (for some reason,<br />
some people seem to have the impression that an<br />
indistinct border is bad; this is distinctly untrue).<br />
There are also other pigmented things in the eye;<br />
choroidal freckles, melanocytomas and CHRPEs<br />
to name a few. Often also choroidal neovascular<br />
membranes look pigmented too. Little spots<br />
of pigment also are common in the retina. The<br />
key thing with most of these is that they don’t<br />
have the above features, except for pigmented<br />
scleral crescents beside the optic disc, commonly<br />
temporally – but these are flat and don’t have any<br />
of the other features.<br />
The bottom line has to be that, at the least, any<br />
pigmented tumour with any of the suspicious<br />
features mentioned has to be seen by an<br />
ophthalmologist, except for little spots of pigment<br />
that are otherwise completely benign looking<br />
beside the disc. Those with suspicious<br />
features will be offered treatment, but<br />
it depends on how suspicious it is, how<br />
worried the patient is and how badly<br />
treatment of it will affect the vision as to<br />
whether treatment will be delivered. If it<br />
is watched, the standard recommendation<br />
is to see it again in three months and then<br />
once a year, to look for growth. This is often<br />
done by optometrists and the main thing<br />
here really is to make sure you look back<br />
at the old photos to make sure it hasn’t<br />
changed. Sometimes even with photos it<br />
can be hard – if a photo is overexposed, it<br />
might make the very thin pigmented border<br />
of the tumour invisible and then, on a<br />
subsequent normally-exposed photo, it will<br />
look bigger. If you have autofluorescence,<br />
make sure you do take an autofluorescence image<br />
at the start because often the borders can be<br />
much easier to see and less open to problems with<br />
exposure than standard photos. Photos taken with<br />
a red filter can also be useful, for the same reason;<br />
they image pigmented choroidal tumours better<br />
since they are less absorbed in the overlying retina<br />
and RPE.<br />
Good luck then with spotting naevi! And if you’re<br />
thinking of buying a camera, consider one that<br />
does autofluorescence; it’s useful in many other<br />
conditions with fluid and RPE changes too, like<br />
macular degeneration and dystrophies. ▀<br />
ABOUT THE AUTHOR<br />
* Dr Peter Hadden practises<br />
at Eye Institute Remuera and<br />
New Lynn, Retina Specialists<br />
and Greenlane Clinical Centre<br />
in Auckland, subspecialising<br />
in vitreoretinal surgery and<br />
adult chorioretinal tumours,<br />
as well as performing<br />
cataract surgery.<br />
<strong>Nov</strong>ember <strong>2016</strong><br />
NEW ZEALAND OPTICS<br />
13