March 2019 digital v1
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
tuberculous granuloma. Liver function test<br />
and renal function test was normal. He was<br />
registered in government DOTS regime.<br />
By 2 months, the pain and swelling<br />
disappeared. By 6 months, ESR become<br />
25. Completed chemotherapy by 9 months.<br />
Rejoined in his company at Ernakulam after 7<br />
months post op.<br />
2yrs follow up<br />
Patient has no complaints. On examination<br />
terminal 10 degrees of flexion limited.<br />
Otherwise healthy.<br />
Differential diagnosis<br />
1. Tuberculosis. 2. Pigmented villo-nodular<br />
synovitis 3. Rheumatoid arthritis 4. Seronegative<br />
arthropathy.<br />
Tuberculosis of the knee causes triple<br />
dislocation due to hamstring spasm and<br />
contracture. These are flexion, posterior<br />
dislocation, lateral rotation and adduction of<br />
tibia. In advance cases in adults, arthrodesis<br />
is done by using Charnley’s compression<br />
arthrodesis. Other causes of triple deformity<br />
are polio and rheumatoid arthritis. DOTS<br />
treatment was for 6 months with 2 months<br />
of four-drug regime and 4 months two-drug<br />
regime. At my request, the medical officer<br />
in charge of DOTs programme extended<br />
treatment up to 9 months<br />
X-ray AP and lateral view of right knee showing<br />
peri articular osteoporosis<br />
The author is additional<br />
professor in Orthopedics,<br />
Govt. Medical College,<br />
Kollam, India.<br />
TUBERCULOSIS OF CALCANEUM<br />
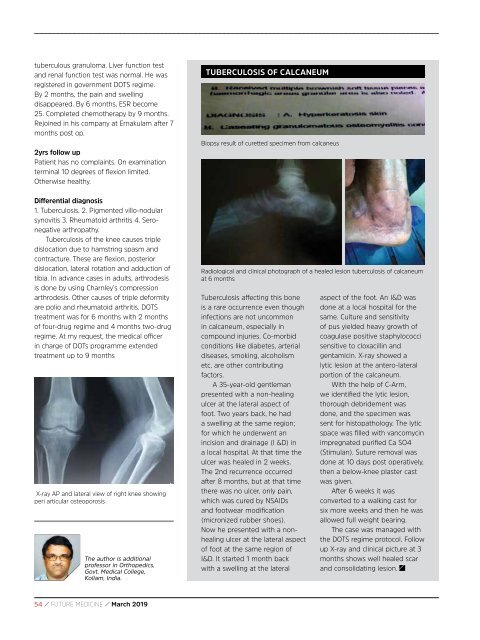
Biopsy result of curetted specimen from calcaneus<br />
Radiological and clinical photograph of a healed lesion tuberculosis of calcaneum<br />
at 6 months<br />
Tuberculosis affecting this bone<br />
is a rare occurrence even though<br />
infections are not uncommon<br />
in calcaneum, especially in<br />
compound injuries. Co-morbid<br />
conditions like diabetes, arterial<br />
diseases, smoking, alcoholism<br />
etc. are other contributing<br />
factors.<br />
A 35-year-old gentleman<br />
presented with a non-healing<br />
ulcer at the lateral aspect of<br />
foot. Two years back, he had<br />
a swelling at the same region;<br />
for which he underwent an<br />
incision and drainage (I &D) in<br />
a local hospital. At that time the<br />
ulcer was healed in 2 weeks.<br />
The 2nd recurrence occurred<br />
after 8 months, but at that time<br />
there was no ulcer, only pain,<br />
which was cured by NSAIDs<br />
and footwear modification<br />
(micronized rubber shoes).<br />
Now he presented with a nonhealing<br />
ulcer at the lateral aspect<br />
of foot at the same region of<br />
I&D. It started 1 month back<br />
with a swelling at the lateral<br />
aspect of the foot. An I&D was<br />
done at a local hospital for the<br />
same. Culture and sensitivity<br />
of pus yielded heavy growth of<br />
coagulase positive staphylococci<br />
sensitive to cloxacillin and<br />
gentamicin. X-ray showed a<br />
lytic lesion at the antero-lateral<br />
portion of the calcaneum.<br />
With the help of C-Arm,<br />
we identified the lytic lesion,<br />
thorough debridement was<br />
done, and the specimen was<br />
sent for histopathology. The lytic<br />
space was filled with vancomycin<br />
impregnated purified Ca SO4<br />
(Stimulan). Suture removal was<br />
done at 10 days post operatively,<br />
then a below-knee plaster cast<br />
was given.<br />
After 6 weeks it was<br />
converted to a walking cast for<br />
six more weeks and then he was<br />
allowed full weight bearing.<br />
The case was managed with<br />
the DOTS regime protocol. Follow<br />
up X-ray and clinical picture at 3<br />
months shows well healed scar<br />
and consolidating lesion.<br />
54 / FUTURE MEDICINE / <strong>March</strong> <strong>2019</strong>