Dive Pacific Iss 171 Oct- Nov 2019
New Zealand's dive magazine featuring in this issue: Shooting big sharks, up close; Spearfishing at night!; Remembering a great Kiwi dive pioneer, Wade Doak; Forgotten Vanuatu wreck's claim to fame; The invasive Lionfish - in depth, plus all our expert columnists
New Zealand's dive magazine featuring in this issue: Shooting big sharks, up close; Spearfishing at night!; Remembering a great Kiwi dive pioneer, Wade Doak; Forgotten Vanuatu wreck's claim to fame; The invasive Lionfish - in depth, plus all our expert columnists
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
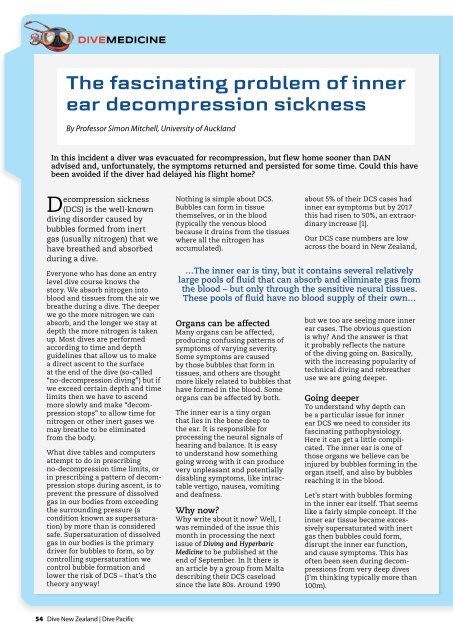
DIVEMEDICINE<br />
The fascinating problem of inner<br />
ear decompression sickness<br />
By Professor Simon Mitchell, University of Auckland<br />
In this incident a diver was evacuated for recompression, but flew home sooner than DAN<br />
advised and, unfortunately, the symptoms returned and persisted for some time. Could this have<br />
been avoided if the diver had delayed his flight home?<br />
Decompression sickness<br />
(DCS) is the well-known<br />
diving disorder caused by<br />
bubbles formed from inert<br />
gas (usually nitrogen) that we<br />
have breathed and absorbed<br />
during a dive.<br />
Everyone who has done an entry<br />
level dive course knows the<br />
story. We absorb nitrogen into<br />
blood and tissues from the air we<br />
breathe during a dive. The deeper<br />
we go the more nitrogen we can<br />
absorb, and the longer we stay at<br />
depth the more nitrogen is taken<br />
up. Most dives are performed<br />
according to time and depth<br />
guidelines that allow us to make<br />
a direct ascent to the surface<br />
at the end of the dive (so-called<br />
“no-decompression diving”) but if<br />
we exceed certain depth and time<br />
limits then we have to ascend<br />
more slowly and make “decompression<br />
stops” to allow time for<br />
nitrogen or other inert gases we<br />
may breathe to be eliminated<br />
from the body.<br />
What dive tables and computers<br />
attempt to do in prescribing<br />
no-decompression time limits, or<br />
in prescribing a pattern of decompression<br />
stops during ascent, is to<br />
prevent the pressure of dissolved<br />
gas in our bodies from exceeding<br />
the surrounding pressure (a<br />
condition known as supersaturation)<br />
by more than is considered<br />
safe. Supersaturation of dissolved<br />
gas in our bodies is the primary<br />
driver for bubbles to form, so by<br />
controlling supersaturation we<br />
control bubble formation and<br />
lower the risk of DCS – that’s the<br />
theory anyway!<br />
Nothing is simple about DCS.<br />
Bubbles can form in tissue<br />
themselves, or in the blood<br />
(typically the venous blood<br />
because it drains from the tissues<br />
where all the nitrogen has<br />
accumulated).<br />
Organs can be affected<br />
Many organs can be affected,<br />
producing confusing patterns of<br />
symptoms of varying severity.<br />
Some symptoms are caused<br />
by those bubbles that form in<br />
tissues, and others are thought<br />
more likely related to bubbles that<br />
have formed in the blood. Some<br />
organs can be affected by both.<br />
The inner ear is a tiny organ<br />
that lies in the bone deep to<br />
the ear. It is responsible for<br />
processing the neural signals of<br />
hearing and balance. It is easy<br />
to understand how something<br />
going wrong with it can produce<br />
very unpleasant and potentially<br />
disabling symptoms, like intractable<br />
vertigo, nausea, vomiting<br />
and deafness.<br />
Why now?<br />
Why write about it now? Well, I<br />
was reminded of the issue this<br />
month in processing the next<br />
issue of Diving and Hyperbaric<br />
Medicine to be published at the<br />
end of September. In It there is<br />
an article by a group from Malta<br />
describing their DCS caseload<br />
since the late 80s. Around 1990<br />
about 5% of their DCS cases had<br />
inner ear symptoms but by 2017<br />
this had risen to 50%, an extraordinary<br />
increase [1].<br />
Our DCS case numbers are low<br />
across the board in New Zealand,<br />
…The inner ear is tiny, but it contains several relatively<br />
large pools of fluid that can absorb and eliminate gas from<br />
the blood – but only through the sensitive neural tissues.<br />
These pools of fluid have no blood supply of their own…<br />
but we too are seeing more inner<br />
ear cases. The obvious question<br />
is why? And the answer is that<br />
it probably reflects the nature<br />
of the diving going on. Basically,<br />
with the increasing popularity of<br />
technical diving and rebreather<br />
use we are going deeper.<br />
Going deeper<br />
To understand why depth can<br />
be a particular issue for inner<br />
ear DCS we need to consider its<br />
fascinating pathophysiology.<br />
Here it can get a little complicated.<br />
The inner ear is one of<br />
those organs we believe can be<br />
injured by bubbles forming in the<br />
organ itself, and also by bubbles<br />
reaching it in the blood.<br />
Let’s start with bubbles forming<br />
in the inner ear itself. That seems<br />
like a fairly simple concept. If the<br />
inner ear tissue became excessively<br />
supersaturated with inert<br />
gas then bubbles could form,<br />
disrupt the inner ear function,<br />
and cause symptoms. This has<br />
often been seen during decompressions<br />
from very deep dives<br />
(I’m thinking typically more than<br />
100m).<br />
54 <strong>Dive</strong> New Zealand | <strong>Dive</strong> <strong>Pacific</strong>