Heartbeat March 2020
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>March</strong> <strong>2020</strong><br />
Sandwell and West Birmingham<br />
NHS Trust<br />
The pulse of community health, Leasowes, Rowley Regis, City Hospital, Sandwell General and the Midland Metropolitan University Hospital<br />
Issue 126<br />
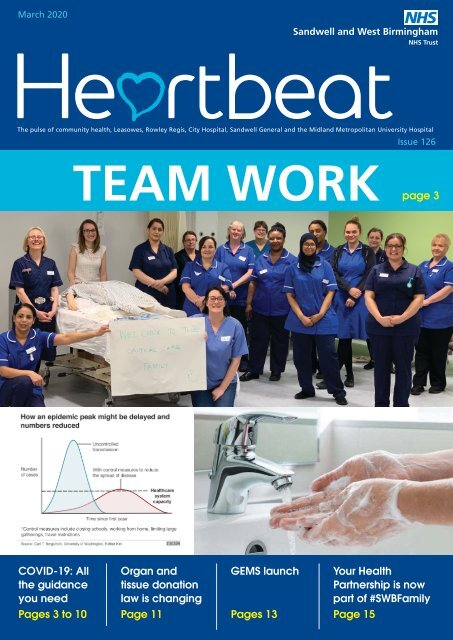
TEAM WORK<br />
page 3<br />
COVID-19: All<br />
the guidance<br />
you need<br />
Organ and<br />
tissue donation<br />
law is changing<br />
GEMS launch<br />
Your Health<br />
Partnership is now<br />
part of #SWBFamily<br />
Pages 3 to 10<br />
Page 11<br />
Pages 13<br />
Page 15
Welcome to the <strong>March</strong> edition of<br />
<strong>Heartbeat</strong>.<br />
We find ourselves in this unique and<br />
unparalleled situation. In tough times<br />
our workplace has shown just how<br />
caring and kind it is – something we<br />
can all be proud of.<br />
This month we bring you stories from<br />
across the organisation. Please enjoy<br />
and catch up on the latest news from<br />
your colleagues.<br />
Contact us<br />
Communications Team<br />
Ext 5303<br />
swbh.comms@nhs.net<br />
Communications Department<br />
Ground Floor, Trinity House<br />
Sandwell Hospital<br />
Published by<br />
Communications Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
Designed by<br />
Medical Illustration,<br />
Graphics Team<br />
Sandwell and West Birmingham<br />
Hospitals NHS Trust<br />
Submit an idea<br />
If you’d like to submit an idea<br />
for an article, contact the<br />
communications team<br />
Ext 5303<br />
swbh.comms@nhs.net<br />
HELLO<br />
Stay updated<br />
We send out a Communications<br />
Bulletin via email every day and you<br />
can now read <strong>Heartbeat</strong> articles<br />
throughout the month on Connect.<br />
Don't forget you can follow us on:<br />
FROM THE CHAIR<br />
Everyone matters as we work<br />
with flexibility and kindness<br />
I have been overwhelmed over recent<br />
weeks by the dedication of colleagues<br />
in our acute medical unit, teams in<br />
theatres, the new Care Homes Service,<br />
primary care and our midwives too,<br />
all working differently to help meet<br />
the challenge of COVID-19. The Board<br />
stands with you. The compassion of<br />
our teams is inspiring particularly in<br />
our A&Es and acute medical areas. I<br />
know that many of you are frightened<br />
and concerned, and that you have<br />
loved ones who echo those fears. At<br />
a senior clinical and managerial level<br />
we are needing to make sense of what<br />
has to happen, learning from London<br />
and overseas, and trying to balance<br />
a Trust response, with one from the<br />
wider region, and consider national<br />
instructions too.<br />
Last Friday we reviewed progress as a Board<br />
and talked through with Toby, Liam and the<br />
team how the first few weeks of mobilisation<br />
had gone. It is clear locally and nationally<br />
that PPE is a real issue with some stock<br />
inflow being patchy. We have gone above<br />
PHE recommendations in many cases. We<br />
have a few hoarders internally and our initial<br />
supply to community settings was not clear<br />
to all colleagues. With the new stock rooms<br />
at the Lyng, D18 and so on, and with the<br />
army now organising the drop, I believe<br />
we can get to a place where – if we can<br />
sort scrubs – we can be confident of<br />
coming on shift with what you need, even<br />
as we expand.<br />
Testing for staff is a nationwide issue. I was<br />
pleased that we were pretty much first out<br />
of the start gate ten days ago with<br />
swabbing, and huge thanks to our<br />
community testers for that. Now the<br />
country is gearing up to “test, test, test”<br />
and I know we will want to make sure that<br />
local GPs, social workers, nurses and ward<br />
service officers are at the forefront. With<br />
the strength of our laboratories within Black<br />
Country Pathology I am sure we are well<br />
placed to begin to get on top of this. The<br />
evidence from overseas seems clear that part<br />
of the curve flattening comes from getting<br />
organised and targeted tests.<br />
However heroic the language used nationally<br />
or locally, the pandemic will bring tragedy<br />
into households and trauma for teams who<br />
see people die before their time, and possibly<br />
without some of their family members able<br />
to visit. We have emphasised psychological<br />
wellbeing and I would urge you to use the<br />
services on offer. Confide in colleagues.<br />
Take time out. Find space to support others.<br />
Where you can, find private places to discuss<br />
your concerns, without showing our patients<br />
the anxiety we share. With social distancing,<br />
and better use of technology, we can find<br />
safe ways to give each other time and<br />
respect and try to support one another.<br />
I know that being asked to work so<br />
differently is an extraordinary request - being<br />
asked to move to a hotel room (or caravan).<br />
I share your worry about other patients<br />
delayed from our care. I am pleased we<br />
have prioritised End of Life Care with the<br />
changes at Leasowes. It is really important<br />
that we look after people with underlying<br />
health conditions among our students, staff<br />
and volunteers. I suspect we are getting<br />
our response broadly right, but sometimes<br />
precisely wrong. Everyone matters and<br />
we need to work hard to find individual<br />
solutions, with flexibility and kindness. We<br />
really do want to hear from you to learn<br />
of your concerns so please get in touch.<br />
We support the difficult decisions you are<br />
having to make as we gear up and see more<br />
patients needing our care. The Trust and NHS<br />
will come through this, as will the country.<br />
How we look after each other now will<br />
define what comes next. Stay well and wash<br />
your hands, often.<br />
Richard Samuda, Trust Chairman<br />
Harjinder Kang, Vice-Chairman<br />
Kate Thomas, Non-Executive Director<br />
Lesley Writtle, Non-Executive Director<br />
Marie Perry, Non-Executive Director<br />
Mick Laverty, Non-Executive Director<br />
Mike Hoare, Non-Executive Director<br />
Waseem Zaffar, Non-Executive Director<br />
Chairman, Richard Samuda
Our Trust’s plan to manage<br />
the pandemic<br />
Treating and caring for a significantly<br />
larger number of patients who may<br />
become increasingly unwell has been<br />
the main challenge for us caused by<br />
coronavirus. We now have a clear plan<br />
in place to manage both the patient<br />
needs and help all colleagues stay<br />
healthy and at work.<br />
Our plan has six parts:<br />
1. Expanding our critical<br />
care capacity<br />
Intensive care will expand into D16 at City<br />
Hospital and Newton 1 (OPAU) at Sandwell<br />
Hospital as this is required. Anaesthetists<br />
and intensivists will run these facilities with<br />
nurses and health care assistants. In order to<br />
properly staff these newly expanded areas<br />
we will need an additional 160 colleagues<br />
to join that team, who will come initially<br />
from theatres but will also need colleagues<br />
in some speciality roles and other ward<br />
areas. Our training has been developed to<br />
equip colleagues with the skills they need.<br />
2. Changes to medical rotas in<br />
our assessment areas and wards<br />
Doctors in higher level training and those<br />
who have been recently working on our<br />
medical wards and assessment units have<br />
to date been staffing these areas. We will<br />
increasingly need to look to doctors from<br />
other areas supporting the rotas including<br />
from surgical and less acute specialties.<br />
Information on the training available is on<br />
Connect.<br />
3. Non-ward based clinicians<br />
to be moved to work on our<br />
wards<br />
With the expanded critical care units and<br />
extra wards open we know we will need<br />
the support of about 100 nurses and<br />
health care assistants, who currently work<br />
in other areas, to care for patients in our<br />
community and acute wards. Training has<br />
been developed and individuals are being<br />
contacted directly to be asked to take on a<br />
new ward-based role.<br />
4. New hires and other<br />
colleagues deployed differently<br />
We are still recruiting! Our therapy support<br />
to our ward areas remains vital and we<br />
know that we will need an increase in<br />
colleagues worked as ward clerks, health<br />
care assistants and ward service officers.<br />
People may be asked to fulfil one of these<br />
roles with the appropriate training.<br />
COVID-19<br />
5. Payment for working<br />
differently<br />
If you are deployed to work in a different<br />
role you will be paid the higher amount<br />
of either your existing salary or new<br />
salary. We will aim to accommodate your<br />
personal circumstances in developing<br />
shift patterns and, where possible, will<br />
move pairs of people from teams to<br />
new roles. Our bank shift rates will also<br />
increase.<br />
6. Integrated care at scale<br />
Acute and community services remain<br />
integrated and we will look to move<br />
roles between different areas. We<br />
continue to support primary care<br />
with staffing and personal protective<br />
equipment (PPE), in particular the<br />
two GP practices in our areas that are<br />
operating solely for COVID-19 patients –<br />
Aston Pride and Parsonage Street.<br />
Thank you to all colleagues who<br />
are and will be working in different<br />
ways to support patients and each<br />
other. You are truly our NHS Heroes.<br />
Intensive care training began on 30 <strong>March</strong> <strong>2020</strong><br />
3
Trust areas turn red and blue<br />
COVID-19<br />
So that it is clear for all colleagues, our wards and clinical<br />
departments are now designated either red or blue.<br />
Red Areas<br />
Blue Areas<br />
Red wards are areas where there are patients being cared for<br />
who are either confirmed as having COVID-19 or displaying<br />
COVID-19 symptoms. In these areas it is vital that the correct<br />
personal protective equipment (PPE) is worn. Each ward door<br />
has an image of what PPE should be worn on entry and for<br />
what procedures.<br />
Blue wards are areas where the patients have no symptoms<br />
of COVID-19. In these areas the PPE requirements are to wear<br />
a fluid-resistant surgical face mask, disposable apron and<br />
disposable gloves.<br />
Our lifts<br />
Minimising the risk of infection spread is vital. Because of this our lifts are also designated as either red or blue: red for the transfer<br />
of patients with COVID-19 symptoms and blue for all other lift usage<br />
4
Managing your health and wellbeing<br />
during COVID-19<br />
Taking care of yourself and in particular,<br />
your psychological health is as<br />
important as your physical health in the<br />
extraordinary times we find ourselves<br />
living in. Self-care is different for<br />
everyone and finding coping mechanisms<br />
that work for you will help to boost your<br />
emotional and mental wellbeing.<br />
To help you stay healthy during this time we<br />
have a wide array of resources available.<br />
Free and confidential<br />
counselling<br />
The Trust offers a free and confidential<br />
counselling service. If you would like<br />
to speak to someone you can call<br />
extension 3306 and ask for a counselling<br />
appointment.<br />
A drop-in counselling service can be<br />
accessed via one of the Trust’s accredited<br />
counsellors on the following days and times:<br />
Mondays: 7pm - 9pm. Linda can be<br />
reached on 07973 664125.<br />
Thursdays: 7 pm - 9 pm. Tony can be<br />
reached on 07970 225929.<br />
You can also access 24/7 counselling<br />
through Health Assured Counselling on<br />
0800 783 2808.<br />
Resilience coaching –<br />
confidential 1-1 support<br />
Resilience Coaching is a 1-1 confidential<br />
conversation and delivered using technology<br />
to make it as easy as possible for colleagues<br />
to access. If you would like to have an<br />
initial conversation to see if this might help,<br />
please email richard.burnell@nhs.net Visit<br />
Connect for further information.<br />
Unmind<br />
Unmind is a mental health platform that<br />
empowers you to proactively improve your<br />
mental wellbeing. Using scientifically-backed<br />
assessments, tools and training you can<br />
measure and manage your personal mental<br />
health needs, including digital programmes<br />
designed to help with stress, sleep, coping,<br />
connection, fulfilment and nutrition.<br />
How to access Unmind:<br />
• Go to nhs.unmind.com/signup<br />
• Sign up with your NHS email address<br />
• Download the Unmind app from your<br />
app store - your organisation name<br />
is NHS<br />
If you do not see your NHS email domain or<br />
have another support query, please visit the<br />
FAQs and support for more information.<br />
Free access to wellbeing apps<br />
NHS staff have been given<br />
free access to several<br />
wellbeing apps from now<br />
until the end of December<br />
<strong>2020</strong> to support your mental<br />
health and wellbeing.<br />
Headspace<br />
Headspace is a science-backed app in<br />
mindfulness and meditation, providing unique<br />
tools and resources to help reduce stress,<br />
build resilience, and aid better sleep.<br />
How to access Headspace:<br />
• Go to www.headspace.com/nhs to<br />
access this app.There is an option to<br />
select clinical or non-clinical staff to start<br />
enrolling.<br />
• You will need to use your NHS email<br />
address to sign up<br />
Access their FAQs and support for more<br />
information.<br />
COVID-19<br />
Sleepio and Daylight<br />
(developed by Big Health)<br />
Sleepio is a clinically-evidenced sleep<br />
improvement programme that is fully<br />
automated and highly personalised,<br />
using cognitive behavioural techniques<br />
to help improve poor sleep.<br />
Daylight is a smartphone-based app that<br />
provides help to people experiencing<br />
symptoms of worry and anxiety, using<br />
evidence-based cognitive behavioural<br />
techniques, voice and animation.<br />
How to access Sleepio:<br />
• Go to sleepio.com/access<br />
• Sign up for an account using your<br />
name and email address<br />
• Click ‘Personalise Sleepio’<br />
• Get started.<br />
How to access Daylight:<br />
• Go to trydaylight.com/access<br />
• Answer a few short questions to<br />
tailor the programme to you<br />
• Sign up for an account using your<br />
name and email address<br />
• Download the Daylight smartphone<br />
app (search ‘Daylight - Worry Less’<br />
on both iPhone and Android)<br />
• Get started.<br />
For technical support please<br />
contact hello@sleepio.com or<br />
hello@trydaylight.com<br />
Priority shopping at<br />
supermarkets<br />
Many of the major supermarkets have a<br />
reserved time for NHS workers to do their<br />
shopping outside of busy periods.<br />
• Sainsbury’s - every day from 7.30 am<br />
- 8 am<br />
• Asda - Monday, Wednesday and Friday<br />
8 am – 9 am<br />
• Tesco - Every Sunday, priority browsing<br />
hour before checkouts open<br />
• Co-op - Monday – Saturday, 8 am –<br />
9 am and Sunday 10 am – 11 am<br />
• Marks and Spencer - Tuesday and<br />
Friday – the first hour of opening<br />
• Morrisons - Monday to Saturday, the<br />
first hour of opening<br />
• Iceland - Monday to Friday, the final<br />
hour of trading.<br />
• Aldi - open 30 minutes early on<br />
Sundays for NHS, police and fire service.<br />
Priority entry will be given to those with<br />
an NHS badge at any time of the day.<br />
Why not visit our very own pop<br />
up shop?<br />
Your Trust Charity has recently launched a<br />
pop up shop at Sandwell Hospital. This shop is<br />
specifically for our frontline colleagues.<br />
You are able to purchase essential items such<br />
as pasta, fruit, toilet roll and cleaning products.<br />
Only card and contactless payments are accepted<br />
and items are limited to one per person.<br />
The pop up shop is located in seminar room<br />
seven, learning and development. The shop will<br />
be open on the following days and times:<br />
• Monday, Wednesday and Friday<br />
• 7.30am – 10am and 13.30 – 16.00<br />
We are working with a local business near<br />
City Hospital to try and secure priority<br />
entrance to staff with preference on<br />
selected goods. We’re also working hard to<br />
provide colleagues in the community with<br />
access to care packages. Watch this space<br />
for more information!<br />
5
Face visor<br />
Disposable<br />
gloves<br />
FFP3<br />
Long<br />
sleeved<br />
gown<br />
Scrubs<br />
Surgical<br />
face mask<br />
Disposable<br />
apron<br />
Disposable<br />
gloves<br />
This does not mean that in COVID ward areas this protection<br />
must be worn all the time or by all entrants<br />
Face visor<br />
Disposable<br />
gloves<br />
FFP3<br />
Long<br />
sleeved<br />
gown<br />
Taking care to protect each other<br />
COVID-19<br />
Know when to self-isolate<br />
For colleagues who have symptoms of<br />
either a persistent cough or a raised<br />
temperature the guidance is that you selfisolate<br />
for a minimum of 7 days from<br />
the date your symptoms started. When<br />
self-isolating, notify your line manager and<br />
confirm the date of your self-isolation and<br />
discuss whether you are able to undertake<br />
any work at home.<br />
On day 8, if your symptoms have improved,<br />
you feel better and you have no fever you<br />
are able to return to work.<br />
Isolation when living in a symptomatic<br />
household<br />
If you live in a household where one of your<br />
household develops symptoms, then all<br />
members of the household must selfisolate<br />
at home for a period of 14 days.<br />
This isolation period starts from the date<br />
that the first person in the household began<br />
showing symptoms. If you are a patientfacing<br />
colleague we would strongly<br />
recommend that you move into one of<br />
our hotel rooms.<br />
Staff who have had contact with<br />
patients who are confirmed positive for<br />
COVID-19<br />
If you have been in contact with patients<br />
who are confirmed positive for COVID-19<br />
you can remain at work if you do not have<br />
symptoms. If you become symptomatic<br />
at any point, you must self-isolate in<br />
line with the guidance.<br />
Hotel accommodation is on offer to you<br />
You may find you have to remove yourself<br />
from your normal home, either to protect<br />
your loved ones or ensure you are able to<br />
help the NHS by staying well. We would<br />
urge colleagues to consider this option,<br />
which all of the NHS is working through.<br />
Leaving loved ones and established<br />
households is not easy, but as travel gets<br />
tougher, shift patterns change, and it<br />
becomes ever more vital to be ready for an<br />
evolving patient care emergency.<br />
To book a room please contact the team on<br />
swbh.hotel-booking@nhs.net<br />
If your request is out of hours, you will get<br />
an out of office email with instructions of<br />
the number to call in order to book your<br />
room.<br />
In addition, we have got on-site<br />
accommodation available for up to seven<br />
days aimed primarily at people working<br />
exhausting shift patterns or live far away.<br />
You can connect with that offer through<br />
our accommodation service via IVOR. We<br />
have paused refurbishment work on some<br />
rooms while we face the first phase of<br />
COVID-19.<br />
Personal Protective Equipment (PPE)<br />
What should I wear?<br />
Our guidance on the correct PPE to use has<br />
been in most cases ahead of the national<br />
guidance from Public Health England and<br />
is to ensure that we protect all colleagues<br />
caring for patients who may or may not<br />
have COVID-19.<br />
For all contacts with patients you<br />
should wear:<br />
• Fluid-resistant surgical mask<br />
• Disposable gloves<br />
• Disposable apron<br />
This now includes all visits to patients in<br />
their own homes and clinic appointments.<br />
Sandwell and<br />
West Birmingham<br />
LOW<br />
INFECTION<br />
AREA<br />
On entering this ward<br />
you MUST wear a<br />
surgical mask<br />
In blue areas you should wear:<br />
• Fluid-resistant surgical mask<br />
• Disposable gloves<br />
• Disposable apron<br />
NHS Trust<br />
Please ensure you wear the<br />
correct PPE in this area.<br />
In red areas you should wear:<br />
• Fluid-resistant surgical mask<br />
• Disposable gloves<br />
• Disposable apron<br />
If you are doing aerosol-generating<br />
procedures (AGPs) or you are providing<br />
close care (within 1 metre) of a +COVID<br />
patient who is at risk of rapid deterioration<br />
you should wear:<br />
• FFP3 mask that you have been face<br />
fitted for<br />
• Face visor<br />
• Long-sleeved gown<br />
• Disposable gloves<br />
• Disposable apron<br />
Sandwell and<br />
West Birmingham<br />
HIGH<br />
INFECTION<br />
RISK AREA<br />
Aerosol<br />
Generating<br />
Procedure (AGP)<br />
Hand washing<br />
COVID-19 suspected<br />
or confirmed or not<br />
been screened<br />
for symptoms<br />
Hand washing<br />
NHS Trust<br />
Close care of +COVID-19<br />
patients (less than 1 metre)<br />
where rapid deterioration<br />
is likely<br />
Hand washing<br />
Where should I get my PPE from?<br />
PPE stocks are available in all ward<br />
areas, clinical departments and<br />
community bases. There are stocks<br />
available from distribution hubs<br />
across the Trust including Rowley<br />
Regis Hospital, the Lyng, D18 at City<br />
Hospital and the Bryan Knight Suite<br />
at Sandwell Hospital.<br />
PPE stations are in place outside wards.<br />
These allow staff coming onto a ward<br />
to put on the correct PPE before<br />
entering. It is primarily intended for the<br />
use of porters, therapists, pharmacists,<br />
transport colleagues and ward service<br />
officers. Wards should not use the<br />
station to replenish their own stocks.<br />
This must be sought from their site<br />
distribution hub.<br />
How do I get FIT tested?<br />
More FIT testing sessions are in<br />
place and you can book your own<br />
appointment by calling 5050. You don’t<br />
need to take a mask with you. You will<br />
be supplied with the correct FFP3 mask<br />
as part of your FIT test.<br />
6
It’s not all about hospitals: Read about<br />
our community response to COVID-19<br />
Mel Roberts<br />
Group Director of<br />
Operations - Primary<br />
Care, Community<br />
and Therapies<br />
Most of the services in the community<br />
have had to think quickly about how they<br />
previously delivered care and what they<br />
need to do now. This has meant that<br />
some of the developments have needed to<br />
happen at pace. Community teams have<br />
been amazing in how quickly they have<br />
responded to these changes and developed<br />
their own ideas about how to provide care<br />
safely for our vulnerable patients. Services<br />
that were deemed more ‘routine’ or nonessential<br />
have either been scaled back or<br />
are being offered virtually via technology.<br />
Helen Hurst<br />
Director of<br />
Midwifery<br />
Babies will not stop arriving and unlike<br />
many other services, we cannot reschedule<br />
for a later date! Our service comes with a<br />
time specific package, an incubation period<br />
all of its own - 40 weeks approximately. So,<br />
how can we do things differently?<br />
Well, we have a developed a business<br />
continuity plan based on guidance from<br />
the Royal College of Obstetricians and<br />
Gynaecology that covers the impact on our<br />
available workforce. Our consultants in both<br />
obstetrics and neonates are undertaking<br />
clinics remotely where possible and we have<br />
aligned the pathways to reduce the need<br />
for multiple appointments. Our sonography<br />
team and obstetricians have developed a<br />
plan for screening of unborn babies, with<br />
reduced attendances. Our community<br />
Face to face activity has been reduced to<br />
minimise the infection control risk.<br />
Admission avoidance visits across the<br />
community continues to be a priority as<br />
does support to discharge patients from<br />
ward areas to ensure patient flow.<br />
There is no doubt that these are difficult<br />
times. Everyone is affected personally<br />
in a different way. There are anxieties,<br />
mostly around PPE and safety. Front line<br />
colleagues are worried because community<br />
work in patients’ own homes can be quite<br />
unknown until you get there. But there<br />
are also worries about family situations<br />
– elderly relatives, childcare and loved<br />
ones. Colleagues are coping remarkably<br />
well during what is a very uncertain time.<br />
There is a real sense that we are all in this<br />
together and a willingness to be flexible to<br />
do what needs to get us all through.<br />
teams are working from their bases on<br />
the whole, undertaking post-natal triaging<br />
and ensuring our most vulnerable families<br />
continue to have care in their homes, whilst<br />
we deliver other care via postnatal clinics.<br />
Inpatient (maternity and neonates) services<br />
have created hot zones and pathways<br />
to care for our women and babies with<br />
confirmed or suspected COVID-19. These<br />
areas are also used by our community staff,<br />
ensuring we are working together as one<br />
family.<br />
We are all anxious, worried and scared.<br />
But we are coming together united in<br />
one belief that we will persevere. We will<br />
ensure all our staff, women and families are<br />
supported during this unprecedented time<br />
and things that we put in place now will<br />
help to shape our service to come.<br />
As midwives our worry is that women will<br />
choose not to engage with us as they are<br />
scared and we see an increase in mortality<br />
and morbidity that we have worked so hard<br />
to reduce. Now, more than ever, we need to<br />
listen and advise.<br />
COVID-19<br />
Dottie Tipton<br />
Primary Care<br />
Liaison Manager<br />
There have been several changes to GP<br />
practices and how they work. We now<br />
have two ‘hot’ sites set up to manage<br />
symptomatic patients from practices across<br />
Sandwell and West Birmingham - Parsonage<br />
Street that previously housed the Walk in<br />
Centre and our own Lyndon Health Centre,<br />
and Aston Pride Health, which was a branch<br />
practice of Newtown Health Centre. All<br />
patients will be booked into appointments<br />
at these sites by their own GP Practice<br />
or by colleagues in NHS 111. Walk-in<br />
appointments are not available.<br />
Practices across Ladywood, Perry Barr and<br />
Sandwell have swiftly moved all services<br />
to a telephone triage model, much like<br />
our hospital outpatient clinics. For a few<br />
patients that will mean they will be invited<br />
into practice to be seen, if the consultation<br />
by phone or video is not enough.<br />
A home visiting service went live on 30<br />
<strong>March</strong> with an initial capacity of 10 slots<br />
per day and plans to expand. The service<br />
will take referrals from practices for patients<br />
who need a home visit but do not require<br />
district nurse input. Some practices have<br />
seen as much as 25 per cent reduction in<br />
available workforce and therefore practices<br />
are looking to reduce the number of sites<br />
that patients are seen face to face.<br />
It’s not all plain sailing, though and practices<br />
are worried about a number of things<br />
including whether they can have access<br />
to staff testing which we are looking to<br />
support.<br />
Cheryl Newton<br />
Group Director of<br />
Nursing - Women<br />
and Child Health<br />
Children and families in our communities<br />
still require support, even more so with the<br />
requirements of self-isolation and social<br />
distancing. The formal and informal support<br />
networks for families with newborn,<br />
toddlers or school age children are now<br />
significantly reduced which can mean<br />
people need more support from us, not less.<br />
We are using various technology to give<br />
them access to our community children’s<br />
nursing team when they need us.<br />
We recognise that some of our families with<br />
increased vulnerabilities may still need face<br />
to face contact and this is being maintained<br />
where possible. We have developed<br />
business continuity plans across all of the<br />
children’s community services. Our staff<br />
groups are adopting a flexible approach to<br />
providing on-going support to our children<br />
and families. We are utilising technology<br />
to provide virtual appointments where<br />
appropriate and offering face to face<br />
contacts for those children who<br />
require it.<br />
The impact of self- isolation and social<br />
distancing on the emotional health and<br />
well-being of our communities remains<br />
to be seen. Our main aim is to help<br />
families continue to reach out to our<br />
services for support during this time and<br />
we want to ensure that the child’s voice<br />
is still heard as families deal with the<br />
extraordinary circumstances we all find<br />
ourselves.<br />
7
It's never been more important to<br />
clean, clean, clean<br />
COVID-19<br />
Do you know how to wash your<br />
hands the NHS way?<br />
Washing your hands is an essential part<br />
of infection, prevention and control.<br />
All colleagues must wash their hands<br />
or use hand sanitiser on entering and<br />
exiting clinical areas. Clinical colleagues<br />
are reminded of the five moments of<br />
handwashing:<br />
1. Before touching a patient<br />
2. Before clean/aseptic<br />
procedures<br />
3. After body fluid<br />
exposure/risk<br />
4. After touching a patient<br />
5. After touching patient<br />
surroundings.<br />
Washing your hands is one of the simplest<br />
ways you can protect yourself and others<br />
from illnesses. Washing your hands properly<br />
removes dirt, viruses and bacteria to stop<br />
them from spreading to other people and<br />
objects, which can spread illnesses. It can also<br />
help stop people from picking up infections<br />
and spreading them to others.<br />
As we all try to navigate life with the<br />
threat of COVID-19 we’ve highlighted<br />
some easy to follow steps to ensure<br />
your hands are squeaky clean.<br />
1. Wet your hands with water<br />
2. Apply enough soap or hand wash to<br />
cover your hands<br />
3. Rub your hands together<br />
4. Use one hand to rub the back of the<br />
other hand and clean in between the<br />
fingers. Do the same with the other<br />
hand<br />
5. Rub your hands together and clean in<br />
between your fingers<br />
You must wash your hands thoroughly for no<br />
less than 20 seconds each time<br />
6. Rub the back of your fingers against<br />
your palms<br />
7. Rub your thumb using your other<br />
hand. Do the same with the other<br />
thumb.<br />
8. Rub the tips of your fingers on the<br />
palm of your other hand. Do the<br />
same with other hand<br />
9. Rinse your hands with water<br />
10. Dry your hands completely with a<br />
disposable towel where possible<br />
11. Use the disposable towel to turn off<br />
the tap.<br />
Ward services officers on the frontline<br />
The unsung heroes of our Trust who<br />
continue working on the frontline<br />
helping our workplace stay one step<br />
ahead of COVID-19 are our army of<br />
ward services officers. Compassionate<br />
and dedicated, our ward services<br />
officers continue to battle with<br />
COVID-19 by keeping our sites clean<br />
and tidy.<br />
With their high standards of hygiene our<br />
ward services officers have taken on the<br />
challenge of ensuring that our wards and<br />
departments are spotlessly clean so that<br />
clinical colleagues can continue providing<br />
safe and effective care.<br />
To find out more about the work of the<br />
ward services team, <strong>Heartbeat</strong> caught up<br />
with Ward Service Officers (WSOs) Christine<br />
Jukes and Julie Brazier. Giving an insight in<br />
to the work of WSOs Christine said, “We<br />
owe it to all of the patients at our Trust to<br />
make sure that we have a clean hospital<br />
for them to come in to and likewise for<br />
colleagues to work in. COVID-19 has simply<br />
reminded us how important our role is in<br />
making sure that the virus does not have an<br />
opportunity to settle, transfer or take hold<br />
in our hospital. Every one of my colleagues<br />
understands that the role they play in<br />
the current situation really does have an<br />
impact.”<br />
Ward Services Officers Christine Jukes and Julie Brazier "in action"<br />
Echoing the words of her colleague, Julie<br />
said, “I’ve worked here for 20 years and<br />
it’s fair to say COVID-19 has been a bit of<br />
a wake up call for everyone. We're now<br />
more focused than ever on making sure<br />
every surface and touch point is spotlessly<br />
clean and kept clean throughout each day.<br />
COVID-19 is very easy to pass on through<br />
droplets and touch so our work is extremely<br />
important.<br />
“However, it’s not all mops, buckets and<br />
dusters. As WSOs we’re an extra set of eyes<br />
on the wards. Whilst we clean, we have<br />
an opportunity to interact with patients.<br />
When we get them a drink we have an<br />
opportunity to have a chat and gain an<br />
insight in to their health and wellbeing and<br />
more often than not they’ll tell us when<br />
they’re feeling well and when they’re not.<br />
We’re able to work with the rest of the<br />
ward team and get involved.”<br />
8
Supporting colleagues - swabbing<br />
for safety<br />
Our focus on keeping our colleagues<br />
safe has never been stronger than<br />
it is right now under the strain of<br />
COVID-19 and to support colleagues<br />
affected by the virus we have<br />
restarted our staff swabbing clinics.<br />
The commitment shown by colleagues<br />
delivering frontline care to patients has<br />
been amazing. As a Trust, we have a<br />
vital part to play in making sure that<br />
colleagues have access to healthcare<br />
and testing to ensure they can protect<br />
themselves, their families and the people<br />
around them.<br />
Colleagues who are symptomatic and<br />
self-isolating now have the opportunity<br />
to book into our COVID testing clinics.<br />
These are drive-in clinics that colleagues<br />
can book in to and then be tested from the<br />
comfort of their car.<br />
To find out more about the drive-in swab<br />
testing clinics, <strong>Heartbeat</strong> caught up with<br />
Practice Educator, Digital Lead Nurse and<br />
now staff swab tester Andrew Churm. He<br />
said: “We are doing community testing to<br />
support our colleagues who we appreciate<br />
are working in difficult environments<br />
such as accident and emergency and the<br />
acute medical unit. This type of testing<br />
means that staff can get back to work to<br />
help support their colleagues. We may be<br />
outside doing the swabbing in a car park<br />
COVID-19<br />
but we see it as being part of a wider<br />
team effort.”<br />
Andrew added: “The team are doing a<br />
fantastic job across our sites, they are<br />
pulling together and there is a good<br />
uptake from staff which we’re pleased<br />
about.”<br />
If you are symptomatic and you<br />
want to book into one of the clinics,<br />
simply call 0121 507 2664 and select<br />
option 5.<br />
Colleagues who are symptomatic can book an appointment at our COVID testing clinics<br />
9
When is working from home the<br />
right thing to do?<br />
COVID-19<br />
Doing what we can to reduce the<br />
risk of spreading the infection<br />
remains essential and we know that<br />
many colleagues have asked or been<br />
asked to work from home. Every<br />
employee is essential to this Trust<br />
and working from home does not<br />
mean that you are less important.<br />
The NHS is a team.<br />
With over 1800 roles in our organisation<br />
we can’t produce a list of everyone who<br />
should and shouldn’t be working at<br />
home so please consider the following<br />
guide:<br />
• If you work administratively,<br />
managerially or clinically in<br />
a patient facing area, we do not<br />
recommend that you work from<br />
home.<br />
• If you provide ancillary work, for<br />
example as a porter or driver,<br />
supporting patient care, including<br />
transporting samples or stock, we<br />
do not recommend that you work<br />
from home.<br />
• If you work in a corporate /<br />
backbone function, for example<br />
in finance, governance or HR, it<br />
may be possible for you to work<br />
from home.<br />
If you are able to work from home<br />
there are circumstances where we may<br />
ask you to return to site, and return to<br />
Some colleagues have asked or been asked to work from home<br />
undertake different work in support of the<br />
pandemic response.<br />
We cannot provide computer equipment for<br />
everyone working from home. Our priority<br />
is clinical areas for technology. But we have<br />
published on Connect simple guidance for<br />
how you can use technology which you can<br />
download to run or be part of meetings,<br />
and how you can potentially get access to<br />
drives and documents.<br />
If you wish to work from home and are<br />
covered by the bullet points above we<br />
would ask you to do four things:<br />
1) Talk to your line manager and<br />
discuss this with them. Their<br />
agreement is required.<br />
2) Send an email explaining your<br />
job role and the decision you<br />
and your manager have made to<br />
swbh.wfh@nhs.net. This will help<br />
us know who is away but well.<br />
3) Download the myConnect App onto<br />
your phone so you can keep up to<br />
date with our guidance and stay in<br />
touch with the Trust.<br />
4) Make sure it is clear on your Trust<br />
emails and Trust telephone extension<br />
answerphone that you are working<br />
from home due to COVID.<br />
Your role in supporting the social<br />
distancing and restrictions to travel are<br />
greatly appreciated and will help to<br />
slow down the spread of the virus.<br />
Changing your role and volunteering<br />
for the fight<br />
The Trust issued working from<br />
home guidance which expires on<br />
7 April. The main reason for that<br />
timeline was to make sure we had<br />
organised the technology to support<br />
the changes that have to happen.<br />
We wanted to make sure that key<br />
computing resources were not being<br />
deployed mainly for non-clinical<br />
work. Those arrangements are in<br />
hand.<br />
The other factor is our need to create<br />
groups of colleagues, allied to medical<br />
students and other volunteers, able to<br />
collaborate in key non-clinical tasks, many<br />
in patient facing areas. Bank and agency<br />
arrangements are not going to be sufficient<br />
to manage a sustained pandemic response.<br />
Sickness including isolation means we are<br />
working to a plan that assumes a 30%+<br />
absence rates.<br />
Chief Executive, Toby Lewis, told <strong>Heartbeat</strong><br />
about the intentions now; “This is a truly<br />
difficult and unprecedented situation.<br />
With this in mind we are doing two things:<br />
Finalising the list of where we need help.<br />
There are obvious priorities like cleaning and<br />
portering. But there are other things that<br />
can be done remotely.<br />
“And completing an analysis of all roles<br />
beyond the clinical space to work which<br />
have to be maintained and who therefore<br />
is potentially available for other work for<br />
a temporary period. Our preference is for<br />
corporate colleagues to volunteer into<br />
new roles, but ultimately there is likely to<br />
be an insistence process which kicks off<br />
before Easter. Of course anyone returning<br />
to site for these roles would have access to<br />
isolation accommodation, like our hotels,<br />
alongside those working in existing clinical<br />
teams.”<br />
10
Celebrating our<br />
stars of the week<br />
Star of the Week<br />
Tracy Weston<br />
Ward Sister<br />
Congratulations to Ward Sister, Tracy<br />
Weston who has gone above and<br />
beyond in supporting her colleagues to<br />
get to grips with Unity.<br />
Star of the Week<br />
Cath Price<br />
Labour Ward Manager<br />
Congratulations to Cath Price, Labour<br />
Ward Manager who has gone above<br />
and beyond in supporting colleagues to<br />
transition to her department.<br />
Cath was nominated for the weekly Star<br />
Award by her colleague Charlotte Duhig for<br />
Tracy Weston was nominated for the weekly<br />
accolade by Health Informatics Matron,<br />
Sharon Reynolds who was pleasantly<br />
surprised whilst supporting Tracy with some<br />
Unity training.<br />
Nominating Tracy for the award, Sharon<br />
wrote, “I have sat with Tracy today to<br />
complete her training on accessing live<br />
safety plan data. During the session we<br />
reviewed patients risk assessments and care<br />
plans.<br />
“Her staff clearly have a good<br />
understanding of Unity and the workflows<br />
as her patients all had care plans initiated<br />
and were being used to document nursing<br />
care. This is the first ward I have seen use<br />
the care plans in Unity really well.”<br />
the support she had given Charlotte as she<br />
began working on the labour ward.<br />
Nominating Cath for the award, Charlotte<br />
wrote, “I was very nervous and daunted<br />
about my new role as a band 7. Cath<br />
and the team on labour ward made<br />
the transition from working in low risk<br />
maternity care to high risk very smooth.<br />
“Cath took time every shift to make sure<br />
I was coping and ensure my learning was<br />
on track. The team on labour ward were<br />
so supportive and encouraging, giving<br />
me feedback and taking time to discuss<br />
problems I encountered.<br />
“Cath is a fabulous team manager with<br />
an open door policy. She always makes<br />
time to listen even though she has a<br />
large workload; she’s always smiling and<br />
constantly caring.”<br />
Well done Cath!<br />
Star of the Week<br />
Jessica Arnold<br />
Service Manager<br />
Congratulations are in order for Star<br />
of the week Jessica Arnold, Service<br />
Manager in the Mortuary Service.<br />
Jessica was nominated for the weekly<br />
award by Matron, Joanne Thomas, after<br />
supporting the ward with a rapid release.<br />
Nominating Jessica for the award, Joanne<br />
wrote, “Jessica helped support us with<br />
a rapid release from Priory 4, this was<br />
achieved within 40 minutes and was only<br />
achievable by the coordination of the ward<br />
and Jessica. However, not only was this<br />
an excellent achievement, following the<br />
rapid release – Jessica then spent time with<br />
a newly appointed band 7 explaining the<br />
procedure – teaching and giving the band<br />
7 eLearning sites and reading material to<br />
facilitate an out of hours rapid release.<br />
“During this teaching, the mortuary<br />
was very busy with doctors and patients<br />
being received, however the compassion<br />
and dedication to both patients, doctors<br />
and teaching all at the same time was<br />
commendable. She truly went the extra<br />
mile.”<br />
Well done Jessica!<br />
Star of the Week<br />
Fran D’Souza<br />
Advanced Physiotherapist<br />
Congratulations to Advanced<br />
Physiotherapist, Fran D’Souza who<br />
went above and beyond the call of the<br />
duty in supporting a frail and elderly<br />
patient to be discharged.<br />
Fran was nominated for the weekly award<br />
by her colleague Hannah Jenns. Nominating<br />
Fran for the award, she wrote, “Fran went<br />
the extra mile to ensure a frail, elderly<br />
patient was able to be discharged home as<br />
planned, equipment needs changed at the<br />
last minute and it wasn’t possible for what<br />
was needed to go in on time. Fran kept<br />
everyone involved in the loop and reassured<br />
everyone. She went out of her way to<br />
collect and deliver equipment and then<br />
check in on the patient the morning after<br />
discharge to ensure all went smoothly.<br />
“The patient involved was very pleased to<br />
be able to go home that day and it also<br />
prevented another unnecessary few days in<br />
hospital.”<br />
Well done Fran!<br />
Well done to all of our<br />
winners. Keep a look out for<br />
<strong>March</strong>'s winners in the next<br />
edition of <strong>Heartbeat</strong>.<br />
11
Organ and tissue donation law<br />
is changing<br />
CORPORATE AND GENERAL<br />
NEWS<br />
12<br />
This month, guest writer, Dr<br />
Niroshini Karunasekara gives us an<br />
insight into the upcoming changes<br />
in the law around organ and tissue<br />
donation.<br />
In what is shaping up to be an<br />
unprecedented year for our NHS,<br />
there is a concern that the imminent<br />
introduction of the donor opt-out system<br />
in England may be overshadowed.<br />
The Organ Donation Act 2019 was<br />
passed by Parliament resulting in the<br />
planned implementation of an opt-out<br />
system. The change in the legislation<br />
applies to both organ and tissue<br />
donation. In real terms, it means that<br />
all patients will be considered to have<br />
consented to donation unless otherwise<br />
stated.<br />
When discussing this topic, it is<br />
important to distinguish between organ<br />
donation and tissue donation. Organ<br />
donation has strict criteria regarding<br />
who is eligible to donate and deals<br />
with organs such as lungs, heart, liver,<br />
kidneys, pancreas and small bowel.<br />
Tissue donation, on the other hand,<br />
includes heart valves, corneas, skin, bone<br />
and tendons and almost everyone is<br />
considered suitable.<br />
Although incorporated within the<br />
act, the subject of tissue donation<br />
will still need to be broached by<br />
medical professionals for the patient’s<br />
information to be passed onto the<br />
National Referral Centre (NRC).<br />
According to NRC data, tissue donation<br />
is a huge area that is still overlooked<br />
nationally. A reluctance to approach<br />
families near or after death means that<br />
many potential donors are missed, and<br />
tissues are not utilised.<br />
Unlike with organ donation, patients<br />
do not need to die in an emergency<br />
department or intensive care unit to<br />
donate tissue after death. Crucially, a<br />
donation must take place within 24 - 48<br />
hours of death. This means introducing<br />
the topic early to a patient’s family is<br />
vital. This will help to maximise the<br />
number of tissue donations in the UK.<br />
In 2011, NICE published guidelines<br />
aimed at improving donor identification<br />
and consent rates. Not only does this<br />
document recommend that all potential<br />
donors should be identified as early as<br />
possible, but also that donation should<br />
be considered as a usual part of end-oflife<br />
care.<br />
20 May <strong>2020</strong> is the date the organ and tissue donation law in the UK changes to opt-out<br />
We conducted a quality improvement project<br />
within our Trust that was designed to assess<br />
our compliance with these expected standards<br />
in post-bereavement care. Specifically, we<br />
looked at whether we are providing the<br />
next of kin with information regarding tissue<br />
donation.<br />
Information was collected from the<br />
bereavement book on each ward within the<br />
Trust, as well as both emergency departments<br />
from September 2018 to September 2019.<br />
We found that of the 586 entries assessed,<br />
only 6 entries (1 per cent) stated that tissue<br />
donation had been discussed with the next of<br />
kin. This discussion is vital to gain consent for<br />
the data to be passed onto the NRC allowing<br />
them to contact families. Common reasons<br />
why this may not be happening on the wards<br />
At SWBH these results have been presented<br />
at local meetings and several strategies<br />
have been initiated to raise awareness of<br />
tissue donation before the implementation<br />
of the new law. These include:<br />
• A series of educational sessions<br />
which have been delivered to<br />
various groups of healthcare<br />
professionals including doctors,<br />
ward staff and emergency<br />
department staff<br />
• A teaching programme for all<br />
professional development nurses<br />
within the Trust so that they can<br />
disseminate information and<br />
include; a lack of awareness about tissue<br />
donation, apprehension of broaching<br />
the subject, and, common cultural or<br />
religious misconceptions.<br />
These results reflect a similar picture<br />
across the UK. It is clear that without<br />
staff engagement, the Organ Donation<br />
Act 2019 will not be as effective as<br />
perhaps expected or hoped with regards<br />
to tissue donation. As 20 May <strong>2020</strong>,<br />
the date for the new legislation rapidly<br />
approaches, staff must be aware of<br />
these changes and also educated and<br />
trained to identify potential donors,<br />
provide information to their next of<br />
kin in a sensitive way, and refer to the<br />
appropriate donation lead for their area.<br />
continually update the nurses on<br />
the wards<br />
• Assessing the feasibility of adding<br />
a mandatory section onto the<br />
patient’s electronic records to<br />
address organ and tissue donation.<br />
These strategies are in keeping with the<br />
principles and recommendations set out<br />
by The Organ Donation Taskforce, the UK<br />
Donation Ethics Committee and GMC<br />
guidelines.<br />
If you have any questions or<br />
queries, please feel free to email<br />
n.karunasekara@nhs.net to find<br />
out more.
GEMS – our valuable pieces<br />
of learning<br />
CORPORATE AND GENERAL<br />
NEWS<br />
Any colleague can identify a learning GEM<br />
<strong>March</strong> saw the launch of our long<br />
awaited learning GEMS initiative to<br />
support colleagues to learn from<br />
our knowledge and experience for<br />
positive results.<br />
GEMS are part of the welearn programme<br />
and are valuable pieces of learning that<br />
have taken place. <strong>Heartbeat</strong> caught up<br />
with Claire Hubbard, Deputy Director of<br />
Governance, Knowledge and Learning who<br />
told us more.<br />
“We are really excited to launch the GEMS<br />
initiative as anyone within the organisation<br />
can take part regardless of their profession.<br />
Any colleague can identify a GEM from<br />
a variety of sources for example, audits,<br />
incidents, learning from excellence,<br />
complaints and observation.”<br />
Claire continued: “We know that an<br />
awful lot of learning happens across our<br />
workplace every day. GEMS will let us<br />
share this knowledge, across the whole<br />
Trust. We want to be an organisation<br />
that is curious.<br />
“And there are many benefits too.<br />
Colleagues from different services and<br />
groups will be able to see what others<br />
are doing as a result of their learning.<br />
Many similar issues in different areas,<br />
and accessing the GEMS store will let<br />
other colleagues see what has been<br />
introduced with success elsewhere.<br />
“By creating a culture where we share<br />
learning, we open ourselves up to being<br />
open to change. Doing this will bring<br />
benefits to patients, particularly around<br />
improving their experience of services.”<br />
Anyone can identify GEMS. Discuss<br />
these with you line manager, or at team<br />
or directorate meetings. Your Group<br />
will need to agree that learning has<br />
happened before a GEMS submission<br />
can be made.<br />
The application is available on<br />
Connect. Once complete, email to<br />
swbh.welearngems@nhs.net<br />
13
Putting the personal into PDRs<br />
CORPORATE AND GENERAL<br />
NEWS<br />
It’s that time of the year where we’re<br />
all being asked to reflect on the past<br />
year and evaluate our performance.<br />
Our Aspiring to Excellence personal<br />
development reviews (PDRs) are<br />
conducted Trust-wide and everyone<br />
is required to have one completed by<br />
30 June.<br />
The appraisal process is your time to<br />
have an open conversation with your<br />
line manager and reflect on what went<br />
well, what could be done differently<br />
and, perhaps most importantly; it’s a<br />
chance for you to focus on your personal<br />
development.<br />
As part of your PDR, you can discuss<br />
your future aspirations and agree upon<br />
a personal development plan. There is a<br />
wide array of training, development and<br />
support available to all colleagues, at all<br />
levels, within our Trust. You may wish to<br />
consider anything from formal training<br />
and apprenticeships to shadowing, a<br />
secondment or getting involved in an<br />
Aspiring to Excellence PDR form<br />
upcoming project.<br />
During your PDR discussion, you will review<br />
your SMART objectives. If you are new to the<br />
organisation or your role, this is the time to<br />
agree upon these together with your manager.<br />
All objectives should be specific, measurable,<br />
achievable, realistic and timely.<br />
All PDRs will result in a performance score<br />
for the previous year, this score is from one<br />
– four and an aspiration score from A– D.<br />
Your discussion will follow the same format<br />
regardless of where you work. The PDR<br />
document has a clear format and will help<br />
to shape your discussion. You will have the<br />
chance to review your performance objectives,<br />
evidence your achievements and discuss how<br />
you’ve performed against our Trust promises.<br />
Be sure to prepare for your PDR. This is<br />
your chance to discuss your work and agree<br />
on a score that’s reflective of what you’ve<br />
contributed to your role, our patients' and the<br />
Trust over the past 12 months.<br />
When completing your PDR you must ensure<br />
that you are 100 per cent compliant with your<br />
mandatory training. It is essential that we are<br />
all safe at work and that patients are safe in<br />
our care. If you're not up to date with your<br />
mandatory training you’ll be unable to progress<br />
through your next pay increment. You will also<br />
be unable to achieve more than a performance<br />
level 2 on your PDR. To easily access your<br />
e-learning visit https://connect2.swbh.nhs.uk/<br />
learning-development/mandatory-list/.<br />
If you are a line manager you need to<br />
complete a short PDR refresher training<br />
session before conducting PDRs. It will<br />
ensure you're up to date on any changes<br />
and also focus on the setting and writing<br />
of SMART objectives. This session can be<br />
booked via my learning on ESR. Should<br />
you have any queries or difficulties<br />
booking onto a session, please email<br />
swbh.landd@nhs.net<br />
City Hospital welcomes new cohort<br />
of students<br />
Our newest cohort of the University College Birmingham (UCB) students at their induction day at<br />
City Hospital<br />
At the start of the decade, City Hospital<br />
welcomed a new group of students to<br />
our Trust.<br />
The University College Birmingham (UCB)<br />
students have joined us for their five month<br />
placement which is part of their extended<br />
diploma in health and social care to help<br />
them attain their full qualification.<br />
“On passing the course, it will mean that<br />
the students will be able to gain entry into<br />
either university or higher education. Once<br />
they have finished the placement it will<br />
enable them to decide whether they want<br />
to specialise in areas such as adult, children’s<br />
nursing or midwifery,” said Janet Stokes, UCB<br />
Employability Tutor.<br />
The placements at City Hospital will give the<br />
students a fantastic opportunity to experience<br />
the care setting first hand which will be<br />
instrumental in their development as the<br />
majority of students have career aspirations<br />
of working in the clinical sector of the NHS<br />
in the future.<br />
Rachel Andrews, Senior Sister from the<br />
deteriorating patient and resuscitation team<br />
will be one of many colleagues supporting<br />
the UCB students whilst they’re at the Trust<br />
and believes it will be a fantastic learning<br />
experience for them.<br />
She said: “The students will gain first-hand<br />
experience on their five month placements,<br />
which will give them a real insight in to the<br />
day to day challenges within the hospital.<br />
The placements will be a real learning<br />
curve for the students but having already<br />
met them, I’m certain they will be a huge<br />
success and a real asset to the wards and<br />
departments they are attending, and<br />
organisation as a whole.”<br />
Good luck to all the students from the<br />
UCB who have started their placements<br />
at the Trust!<br />
14
Milestone merger becomes reality as<br />
Your Health Partnership joins Trust<br />
1 April marks a special date in our Trust<br />
as it’s when we officially welcome<br />
Your Health Partnership (YHP) to our<br />
organisation. Working as an additional<br />
directorate, it marks the start of a new<br />
phase for both our organisation and<br />
Your Health Partnership.<br />
Speaking to <strong>Heartbeat</strong>, Dr Simon Mitchell,<br />
Co-Executive Partner at YHP, said: “This is an<br />
exciting time for us. We have an incredible<br />
team and culture. We’re excited about<br />
working with, and as part of, the wider<br />
organisation.<br />
“We have created a successful business<br />
and we thrive on innovation. Working<br />
together, we will be able to help the most<br />
vulnerable in our society, the housebound,<br />
outpatients, and so many more people. Jointly<br />
we will be able to build resilience and bring<br />
greater improvements in healthcare to our local<br />
communities.”<br />
Primary Care Liaison Manager, Dottie Tipton,<br />
will be working ever closer with YHP as of 1<br />
April. She told us: “YHP joining our Trust is a<br />
truly special moment. It is a testament to their<br />
team, the rapidly scaling business they have<br />
created and their passion.”<br />
So, what will the move look like in reality?<br />
YHP partners and managers will continue to<br />
oversee the running of the practices within<br />
the directorate, whilst our Trust will have<br />
responsibility for delivering the contracts that<br />
the service currently holds. The YHP run Carters<br />
Green Medical Centre will move to the new<br />
CORPORATE AND GENERAL<br />
NEWS<br />
£6 million development which is being<br />
built at our Sandwell Hospital site.<br />
Toby Lewis, Chief Executive said: “Whilst<br />
this is currently a challenging time for<br />
everyone with COVID-19 we can’t<br />
overlook YHP joining our Trust. We have<br />
worked together to get this merger just<br />
right, and we are pleased to welcome<br />
everyone into our organisation. We share<br />
a common vision and that is a solid basis<br />
for any new relationship. I am confident<br />
we will go from strength to strength<br />
together.”<br />
Your Health Partnership have joined the SWB family<br />
<strong>2020</strong> - International Year of the Nurse and Midwife<br />
April <strong>2020</strong> - National Autism Month<br />
2 April Public Trust Board<br />
9.30am - 1pm, Webex<br />
5 April Palm Sunday<br />
9 April Maundy Thursday<br />
10 April Good Friday<br />
12 April Easter Sunday<br />
13 April Easter Monday<br />
16 April QIHD<br />
Afternoon, Trust-wide<br />
17 April Palm Sunday<br />
21 April Clinical Leadership Executive<br />
2pm - 5pm<br />
Post Graduate Centre, City Hospital<br />
22 April TeamTalk<br />
1pm - 2pm, Webex<br />
23 April St George’s Day<br />
World Book Night<br />
24 April Ramadan begins<br />
29 April Yom HaAtzmaut –<br />
Jewish holiday<br />
15
CORPORATE AND GENERAL<br />
NEWS<br />
Shout out has been a regular feature<br />
in <strong>Heartbeat</strong> and it is fantastic to see<br />
colleagues regularly taking the time<br />
to give positive feedback to each<br />
other.<br />
We regularly receive positive feedback<br />
from our patients too, and this month<br />
we wanted to share some of those<br />
heart-warming messages which have<br />
been sent via our website and social<br />
media platforms.<br />
To – Zain Shah<br />
Zain is one of the Trust volunteers. Treats<br />
everyone with respect, is very pleasant,<br />
polite and very helpful. Great energy when<br />
up and down the corridor guiding people<br />
and engages so well with everyone. Will<br />
always ask how you are and always there<br />
with a smile on his face. Keep up the good<br />
work you absolutely brighten up my day<br />
and no doubt many others feel exactly the<br />
same way.<br />
From – Harpal Tiwana<br />
To – Paediatric Diabetic Team<br />
Well done to the Paediatric Diabetic Team<br />
who have the best results in the West<br />
Midlands for blood sugar control and<br />
better than the national average in the<br />
recent national audit. Keep up the good<br />
work and congratulations!<br />
From – Maria Atkinson<br />
To – Peter Smith<br />
A top nurse, always going well and beyond<br />
the call of duty to make sure patient<br />
transfers are done safely and efficiently. A<br />
true gem in AMU!<br />
From – Kenny Tingson<br />
To – Laura Morris<br />
An exceptionally dedicated, hardworking<br />
nurse. I am proud to call her my colleague<br />
and as a team we are lucky to have her.<br />
From – Sophie Fox<br />
To – Charlene Bennett<br />
Charlene always goes above and beyond<br />
to help us to co-ordinate CT scans around<br />
patient's out-patient appointments. She is<br />
always so helpful and friendly.<br />
From – Elizabeth Broome<br />
To – Charlotte Street<br />
Thank you for all the help and support you<br />
have given me for last pass few weeks. It is<br />
nice to know I can call or message you any<br />
time. Once again thank you!<br />
From – Joey Bhirth<br />
To – Kully Sidhu<br />
An exceptional team member! Highlighted<br />
as being caring and compassionate by<br />
doctors, nurses and patients. A true asset to<br />
the team and the respiratory hub!<br />
From – Jacqueline Moore<br />
To – Abiola Adesina and Emma Race<br />
We couldn't have got through a<br />
challenging shift without these fantastic<br />
health care assistants going the extra mile<br />
supporting staff nurses with safe rapid<br />
patient flow, whilst always providing the<br />
gold standard care required.<br />
From – Levie O'Gorman<br />
To – Sylvia Haywood<br />
Thanks for being a great manager from all<br />
of the admin team.<br />
From – Angela Jones<br />
To – Tiffany Jones<br />
One of the most amazing managers I have<br />
come across from the start of my nursing<br />
career (from my fist placement as a student<br />
nurse to present almost 4 years qualified).<br />
You are honestly doing an amazing job,<br />
the way you motivate your team, I've never<br />
worked anywhere were everyone is so<br />
happy to be at work.<br />
From – Vanessa Wright<br />
To – Claire Bingham<br />
Thank you Claire for all your help and<br />
support on tonight’s shift D17 - you are<br />
just fab!<br />
From – Charity Sibanda<br />
To – All the palliative HCAs and DET team<br />
working with the Palliative Care Hub<br />
A massive thank you to all of the HCAs<br />
and DET team for the wonderful care<br />
and support they provide to many of<br />
our patients at a very challenging and<br />
emotionally demanding time. They are<br />
always willing to help and go the extra<br />
mile, with a smile on their face and<br />
treat everyone with dignity, respect and<br />
compassion. We would be lost without you.<br />
From – Molly Casey<br />
To – Fit Testers<br />
Shout out for your kind support with a<br />
particularly difficult situation during the<br />
last hour of a palliative gentleman's life.<br />
Your compassion for our patients is a credit<br />
to you all. Thank you.<br />
From – Yvette Bayley<br />
To – Mandy Mason<br />
I would like to thank Mandy for coming to<br />
help out on neonatal when we was really<br />
busy. Mandy went out of her way to come<br />
and help from her own ward (M1) and help<br />
feed our babies, nothing was too much<br />
trouble.<br />
From – Sarah Shaw<br />
16
Mental health act administrator joins<br />
forces with our Trust<br />
Takesha Sam is helping colleagues to better understand the Mental Health Act<br />
With approximately one in four people<br />
in the UK experiencing a mental health<br />
problem each year, we continue as an<br />
organisation to place a significant focus<br />
on this as well as mental wellbeing.<br />
As mental health disorders can have a<br />
considerable impact on the health of<br />
individuals, we have a duty of care to<br />
ensure we are effectively managing patient<br />
care and treatment.<br />
Newly appointed Takesha Sam is a mental<br />
health act administrator working across our<br />
directorates. Takesha is taking the lead on<br />
ensuring we are meeting our obligations<br />
when dealing with patients with psychological<br />
disorders or mental ill-health. This in part<br />
involves following the correct procedures and<br />
completing accurate paperwork.<br />
Mental health awareness is another aspect<br />
CORPORATE AND GENERAL<br />
NEWS<br />
of Takesha’s role. This will see her<br />
implementing processes to help<br />
colleagues better understand the Mental<br />
Health Act (MHA) and how to apply<br />
it. By managing the administration<br />
of the MHA, Takesha is working<br />
with individuals and teams to ensure<br />
compliance with the MHA, advising on<br />
legal requirements relating to detained<br />
patients such as the renewal of sections.<br />
Speaking to <strong>Heartbeat</strong>, Takesha said,<br />
“My focus is ensuring colleagues<br />
are aware of relevant legislation and<br />
processes. This could be anything<br />
from processing paperwork when a<br />
patient is detained, to ensuring we<br />
have the correct consent in place when<br />
treating patients. Currently, I’m creating<br />
flowcharts that will shortly be circulated<br />
to colleagues.”<br />
If you have any queries, please<br />
feel free to contact Takesha via<br />
t.sam@nhs.net.<br />
From HCA to nursing associate –<br />
the sky’s the limit for Jenni Meeson<br />
Within our organisation, there is a<br />
strong focus on personal development.<br />
With opportunities available to all<br />
colleagues, it’s something we’re<br />
passionate about. Whether you choose<br />
an apprenticeship, external learning<br />
or a degree level qualification, there’s<br />
something for everyone.<br />
Jenni Meeson has taken advantage of the<br />
learning opportunities available at our Trust.<br />
Having worked here for 15 years, for the<br />
most part, she's worked as a health care<br />
assistant (HCA). That all changed when she<br />
decided to take the next step in her career<br />
and become a nurse associate apprentice.<br />
She joined the programme almost two years<br />
ago and, it has been an invaluable learning<br />
experience for Jenni.<br />
The apprenticeship covers all four domains<br />
of nursing – adult, children’s, learning<br />
disabilities, plus mental health. Jenni has<br />
found this hugely informative and, it’s been<br />
enhanced by the clinical work placements<br />
she’s completed and, offsite learning at the<br />
University of Wolverhampton.<br />
Jenni Meeson, Nurse Associate Apprentice<br />
Speaking to <strong>Heartbeat</strong> Jenni explained, “I<br />
worked as a HCA in the community for 15<br />
years. Over that time I worked with a lot of<br />
different teams and developed transferable<br />
skills. That in part, helped me decide to<br />
become a nurse associate apprentice. It<br />
has given me the chance to build on what<br />
I already know and I can now do things I<br />
couldn’t do before such as compressions<br />
and drug rounds.”<br />
With just five months left of her<br />
apprenticeship, Jenni took a moment<br />
to reflect on her learning experience. “I<br />
complete 30 hours each week for my work<br />
placement and a day at university. I’ve had<br />
to do assignments, exams and presentations<br />
as part of my apprenticeship. Ultimately<br />
when I qualify I will gain a foundation<br />
degree as a nursing associate. It will be a<br />
proud moment.”<br />
She added, “I would encourage anyone<br />
interested in becoming a nurse associate to<br />
apply. Once you’ve qualified that’s just the<br />
beginning of your journey - it’s up to you<br />
where you progress to. I feel particularly<br />
grateful that the Trust has invested in this<br />
apprenticeship. I’m also pleased that when<br />
I qualify it will enable me to be a registered<br />
practitioner governed by the Nursing and<br />
Midwifery Council.”<br />
If you’d like to find out more about<br />
becoming a nurse associate apprentice,<br />
email zoetaylor1@nhs.net for some<br />
more information.<br />
17
My Friend Jen – A story about a girl<br />
who’s a little bit different<br />
CORPORATE AND GENERAL<br />
NEWS<br />
Acclaimed sickle cell author,<br />
Jenica Leah recently launched her<br />
second book in the My Friend Jen<br />
series. Coinciding with World Book<br />
Day on 5 <strong>March</strong>, the launch held<br />
in Birmingham celebrated the<br />
release of her latest book called<br />
The Check Up.<br />
The inspirational story told by her friend<br />
follows Jen as she embarks upon a<br />
hospital visit for her sickle cell check-up.<br />
He introduces her by saying, “My friend<br />
Jen is as fun as can be. She wears her hair<br />
big and high for everyone to see.”<br />
Whilst this may be fiction, the story itself<br />
is rooted in fact. Jenica has sickle cell<br />
and is a patient of ours at City Hospital.<br />
Speaking exclusively to <strong>Heartbeat</strong>, she<br />
remarked, “City Hospital is where I have<br />
been cared for since I was a teenager.<br />
They have a dedicated sickle cell and<br />
thalassaemia centre that provides day<br />
care for patients, which I attend.”<br />
When talking about her motivation to<br />
create these books, Jenica said, “I’ve<br />
had sickle cell from birth and, I was in<br />
and out of hospital growing up. I didn't<br />
understand my condition, so I grew up in<br />
Jenica Leah with Eddie Edmead, Major Grants Manager, at the launch of the latest book in the My<br />
Friend Jen series.<br />
isolation, unable to explain what I had or how<br />
it affected me.”<br />
“Living with an invisible illness has led me to<br />
create my children’s book series, My Friend Jen.<br />
I want other children growing up with sickle<br />
cell to have the peace of mind growing up that<br />
I didn’t have. I pride myself on not letting my<br />
condition stop me achieving my goals. I want<br />
other children to grow up and have that same<br />
motivation.”<br />
Eddie Edmead, Major Grants Manager for Your<br />
Trust Charity, attended the book launch.<br />
He said, “It was great to catch up with Jen<br />
again. We have worked together before<br />
for the launch of her first book. This was a<br />
fantastic event that was well put together.<br />
It was great to see so many people there<br />
to support her and help raise awareness of<br />
sickle cell.”<br />
If you’d like to find out more about<br />
Jenica’s journey head on over to<br />
www.myfriendjen.co.uk.<br />
Friends and family – the true test of<br />
the patient experience<br />
The Friends and Family Test has been<br />
a staple in our workplace since its<br />
introduction in 2013. It is however<br />
changing to better meet the needs and<br />
challenges of our organisation and<br />
patient groups.<br />
The Friends and Family Test (FFT) is a<br />
quick and simple way for patients to give<br />
feedback about their experience. It is a<br />
continuous improvement tool that gives<br />
patients the opportunity to anonymously<br />
feedback to our Trust about their care and<br />
treatment.<br />
Friends and Family Tests provide a way<br />
to continuously track the experiences of<br />
patients across our organisation. This allows<br />
us to respond quickly and effectively should<br />
an issue become evident, and likewise, to<br />
celebrate any positive developments.<br />
Feedback can draw our attention to any<br />
immediate or specific issues, as well as<br />
identifying themes. Along with questions<br />
about the overall experience, we will also<br />
be asking patients whether we met their<br />
expectations and if there is anything else<br />
they can tell us.<br />
Individuals can still give feedback via SMS<br />
text message, interactive voice messages<br />
(IVM) or FFT postcards. The mandatory<br />
requirement to ask for feedback at specific<br />
times will be removed. This will enable<br />
patients to give feedback in real-time -<br />
allowing us to address any issues promptly.<br />
For more information about the<br />
changes to the Friends and Family<br />
Test, contact Shila Patel on ext 5188.<br />
Alternatively, please email<br />
shila.patel@nhs.net.<br />
Checklist<br />
• Ensure FFT posters and leaflets<br />
are visible in your area<br />
• Inform patients that they will be<br />
contacted for anonymous<br />
feedback, but there is an ‘opt out’<br />
option should they wish to do so.<br />
• Return all completed postcards<br />
to Shila Patel, Bryan Knight Suite,<br />
Sandwell Hospital making sure<br />
your ward/department name is<br />
clearly written on each postcard.<br />
• Log on to the envoy portal<br />
weekly to view feedback/<br />
comments received to identify<br />
themes or issues raised. Take<br />
action where you can to<br />
implement any quick wins and<br />
follow up with any other issues<br />
that may arise.<br />
18
Year of the Nurse and Midwife<br />
Each month we profile some of our wonderful nurses and midwives as<br />
part of our <strong>2020</strong> Year of the Nurse and Midwife celebrations.<br />
Read on to find out about the career pathway of FGM Specialist Midwife,<br />
Alison Byrne.<br />
She’s the caring midwife who<br />
victims of female genital<br />
mutilation (FGM) receive help<br />
from when they need treatment.<br />
Alison Byrne has been dedicated<br />
to the specialist FGM service<br />
since it was conceived in 2002<br />
to treat and care for pregnant<br />
women within the West<br />
Midlands.<br />
The mum-of-two joined Sandwell and<br />
West Birmingham NHS Trust two years<br />
ago to develop the service further within<br />
the area. Since joining she has led the<br />
opening of a new FGM clinic for nonpregnant<br />
women which will be run by<br />
our organisation. “I have worked within<br />
the FGM field for 18 years and still feel<br />
incredibly passionate about making a<br />
difference for the women who have<br />
undergone<br />
.<br />
the procedure,” said Alison,<br />
when speaking to <strong>Heartbeat</strong>.<br />
“For the pregnant women, it is mainly<br />
to create a positive birth experience and<br />
for non-pregnant women, it addresses<br />
any physical and psychological issues<br />
they may be enduring. I strive to ensure<br />
Alison Byrne<br />
FGM Specialist Midwife<br />
Alison Byrne - championing the rights of<br />
women and making a stand against FGM<br />
that women that come and see us have<br />
the highest standards of care, and I use<br />
a holistic approach to do this. I think it’s<br />
really important that when we are treating<br />
victims of FGM, we are compassionate<br />
and empathetic towards these women<br />
who have undergone such a horrific and<br />
unnecessary experience.”<br />
Alison runs regular clinics at City Hospital<br />
where women’s needs are assessed and<br />
identified. She then creates a care plan<br />
for them. The new FGM clinic, is based<br />
at Summerfield Primary Care Centre in<br />
Winson Green, and works on a similar basis.<br />
Speaking of the project, she said, “The<br />
launch of the FGM clinic was part of a pilot<br />
within NHS England. It makes it so much<br />
easier for women to access this service in<br />
a community setting through any referral<br />
pathway across the Midlands.”<br />
Alison has been recognised for her work,<br />
winning a Royal College of Midwives award<br />
for the service when it first opened. “My<br />
work has taken me to many meetings and<br />
led to various collaborations with national<br />
organisations which I enjoy immensely.”<br />
It’s no surprise to learn that it’s the<br />
continuation of this work with women and<br />
their families that drives Alison. “Within<br />
these communities that I care for, I have<br />
seen the most inspirational people with an<br />
incredible attitude to life,” she added. “I<br />
admire them greatly and am truly inspired<br />
by every one of them. They are my heroes.”<br />
19
Long service awards show dedicated<br />
NHS workers lead by example yet again<br />
CORPORATE AND GENERAL<br />
NEWS<br />
In the last few weeks we have<br />
been reminded of how important<br />
the National Health Service is and<br />
how grateful we are to have it.<br />
Not just as colleagues within our<br />
organisation but as a nation. We<br />
are indeed very lucky to have the<br />
service we do, and our organisation<br />
is very lucky to have the dedicated<br />
colleagues it does.<br />
Across the country we've seen a very<br />
genuine outpouring of affection<br />
towards the NHS and its staff. Before<br />
the Coronavirus became a pandemic,<br />
we ourselves at Sandwell and West<br />
Birmingham took some time to<br />
acknowledge those who have dedicated<br />
themselves to helping the community as<br />
part of the NHS and as a part our Trust.<br />
In February our Chairman, Richard<br />
Samuda hosted our most recent NHS<br />
Service Recognition Ceremony, where<br />
he acknowledged the dedication of<br />
well almost 150 colleagues who have<br />
served the NHS dutifully for 20 years<br />
or more. These included more than 80<br />
Helen Whiles receives her award from Chairman,<br />
Richard Samuda<br />
staff hitting the two decade mark, with 50 at<br />
three decades whilst an astonishing 17 got to<br />
celebrate 40 years’ service as part of the NHS.<br />
Among the 17 includes Helen Whiles who<br />
has spent her career here. Working her way<br />
up from a student technician working in<br />
Stroke of good fortune at<br />
recruiting event<br />
the dispensaries, procurement and on the<br />
wards, all the way to Chief Technician for<br />
City Hospital - prior to the merging of the<br />
two hospital trusts at Sandwell and City.<br />
Emily Horwill spoke to <strong>Heartbeat</strong> about<br />
her friend, jokingly referred to within the<br />
management team as 'Aunty Helen' for her<br />
kind and caring nature to both staff and<br />
patients.<br />
"I have only known Helen for two years<br />
since joining the organisation and Helen<br />
has been really welcoming to me from my<br />
first day. She is currently embracing her<br />
new role as chief technician for medicines<br />
optimisation and can regularly be found on<br />
the wards liaising with ward staff about our<br />
Pyxis, Unity and Abloy systems to make sure<br />
we’re getting the best from them.<br />
"She always enthusiastically takes on board<br />
and participates in change within the<br />
department and has a brilliant work ethic<br />
- and her memory of the organisation is a<br />
brilliant resource. Not to mention a source<br />
of many stories and tall tales! We're very,<br />
very lucky to have her."<br />
Many congratulations Helen and to all<br />
our celebrated colleagues at 20, 30 and<br />
40 years.<br />
MEDICINE AND EMERGENCY<br />
CARE<br />
Valentine’s Day was a busy one for<br />
everyone at our organisation – but<br />
not all the action took place at the<br />
site of the Midland Metropolitan<br />
University Hospital.<br />
At the same time as our relaunch event<br />
at Midland Met, back over at Sandwell<br />
Hospital, members of our existing nursing<br />
team were welcoming people who may<br />
one day be a part of the team that works<br />
at our “super-hospital.”<br />
Members of the stroke services team<br />
were on hand to speak to prospective<br />
candidates as part of the Trust’s latest<br />
recruitment day. The event aimed to fill a<br />
number of roles across a team which has<br />
Members of the stroke services team<br />
an expansive development plan for <strong>2020</strong>; as it<br />
reorganises and further develops the services<br />
it offers. One such project is the new SWAT<br />
team - thankfully not an armed response unit,<br />
but rather the newly formed stroke wellbeing<br />
activity team operating out of Sandwell.<br />
Over the course of the day, a number<br />
of the team spoke to nurses, students<br />
and HCAs that were interested in either<br />
applying for roles, or finding out more<br />
about the service. They also provided lots<br />
of information about flexible working<br />
practices, what the team does and its<br />
plans for the future.<br />
“I’m delighted to say we made a number<br />
of offers over the course of the day and<br />
are adding four band 5, nurses, to our<br />
amazing stroke services team”, Lead<br />
Stroke and Neurology Matron, Jo Thomas<br />
told <strong>Heartbeat</strong>. “Going forward we know<br />
there’s a lot of work to do. We have<br />
several projects that we look forward to<br />
working on over the year. It’s our goal<br />
to make the service and its staff the very<br />
best - this is just the first step towards<br />
achieving that.”<br />
20
Conference shares methods to<br />
improve dignity in care<br />
Our medicine and emergency group<br />
played host to a dignity in care<br />
conference back in February.<br />
The conference had over 120 delegates in<br />
attendance from both clinical and nonclinical<br />
backgrounds including nurses,<br />
midwives, portering and security.<br />
Julie Thompson, Group Director of<br />
Nursing for Medicine and Emergency<br />
Care helped facilitate the all-day event<br />
at our Sandwell Education Centre. The<br />
aim of the session was to share methods<br />
to help improve dignity in care across<br />
the organisation. Presenters at the event<br />
included Dr Moe Thaw Oo, Consultant<br />
Geriatrician and Physician, as well as<br />
Helen Mallard, Lead Nurse.<br />
Dr Oo believes that we must ensure that<br />
dignity in care is equally applied and<br />
consistent for all patients, in particular,<br />
our elderly and more vulnerable patients<br />
He said: “We face many challenges with<br />
our more senior patients, such as more<br />
complex needs and even language barriers.<br />
Even with these challenges, we must ensure<br />
we offer consistency in care and make sure<br />
the dignity of our patients is at the forefront<br />
of our minds. This will ensure they receive<br />
the best possible care from us.”<br />
Helen and her team have applied the ABCD<br />
model in our emergency department (ED)<br />
in regards to dignity in the care they offer.<br />
This method focuses on attitude, behaviour,<br />
compassion and dialogue. She said, “Every<br />
patient that attends ED deserves the same<br />
standards of care. I always encourage<br />
everyone to really think about behaviours<br />
and gestures as this can easily impact on a<br />
patient’s experience, especially in ED.<br />
She went on to say, “Compassion and<br />
dialogue are equally important. This is why<br />
we think that one of the quick wins to this<br />
is caring, showing empathy and simply<br />
treating others how you would wish to be<br />
treated.”<br />
Following on from the success of the<br />
MEDICINE AND EMERGENCY<br />
CARE<br />
event, the Trust has seen well over<br />
200 people sign up to become<br />
dignity ambassadors. “I have been<br />
overwhelmed with the positive<br />
response after the dignity in care<br />
event. It’s amazing to have so many<br />
dignity ambassadors from a variety of<br />
multi-disciplinary teams,” said Julie.<br />
She added, “A dignity ambassador is<br />
someone that upholds the standards<br />
for dignity which is treating people<br />
with respect. This involves being a<br />
patient advocate and feeding back<br />
within our dignity forums. To have<br />
such a large number of people in<br />
these types of roles will mean that our<br />
patients will be treated with kindness,<br />
respect and compassion. It will<br />
ultimately result in better care.”<br />
AMU kicks off journey to be #proud<br />
During one week in February<br />
colleagues from acute medicine at<br />
City and Sandwell were given the<br />
opportunity to share their views and<br />
tell each other why they are #proud to<br />
be part of the team.<br />
The initiative was part of an ongoing<br />
programme to improve morale and<br />
engagement among colleagues.<br />
Senior Sister, Claire Obiakor told <strong>Heartbeat</strong>:<br />
“The event was the result of some work we<br />
have been doing in the AMU improvement<br />
group. It was aimed at helping colleagues<br />
to understand their roles and responsibilities<br />
and how each member of staff contributes<br />
to the overall objectives of the department.<br />
“The team thought a week-long event<br />
where colleagues could pop in would help<br />
create the right environment for colleagues<br />
to find out more about their roles and<br />
responsibilities, ask questions, and more<br />
importantly give us feedback about changes<br />
that could be made to improve colleague<br />
and patient welfare.<br />
“We were thrilled with the engagement<br />
across the two sites. We had colleagues<br />
from Sandwell managing stalls at City and<br />
vice versa. It was excellent cross site team<br />
working. Food and drink was also provided<br />
which is always a nice treat for everyone.”<br />
The AMU improvement group are now<br />
reviewing the feedback and identifying<br />
quick wins so that colleagues can start to<br />
see improvements immediately.<br />
“Any major change will be gradual,”<br />
added Claire. “One common theme was<br />
resourcing - we are currently recruiting<br />
but it will take time for new people to<br />
be in post. Communication was another<br />
theme – however I think the team will<br />
see a marked difference already. Certainly<br />
the #proud event was the start of making<br />
improvements to the way we communicate.<br />
Colleagues in AMU share their reasons for being #proud<br />
“We plan to ensure that we continue with<br />
these events so colleagues can continue to<br />
feel confident that they can have a say and<br />
contribute to the direction of our team.<br />
“And as we prepare for the Midland Met,<br />
we are offering cross site secondments<br />
for Band 6 colleagues and all new starters<br />
will be expected to rotate across City and<br />
Sandwell. It is a very exciting time ahead<br />
and our aim is to ensure everyone is happy<br />
at work which is essential for the team’s<br />
overall health and wellbeing. If the team are<br />
happy, our patients will be happy.”<br />
21
Mouth care pilot leads to magic in<br />
every smile<br />
MEDICINE AND EMERGENCY<br />
CARE<br />
Patients across four wards at City<br />
and Sandwell hospitals have been<br />
all smiles during the pilot of a new<br />
campaign to improve the oral health<br />
of inpatients.<br />
In January colleagues working on D11<br />
D26, Priory 4 and Newton 4 started the<br />
Mouth Care Matters trial. This involved<br />
them receiving specific training and<br />
equipment to carry out effective mouth<br />
care on patients.<br />
Colleagues have been ensuring that every<br />
patient cleans their teeth/dentures at<br />
least twice a day and those with complex<br />
mouth care needs are assisted with more<br />
frequent care.<br />
<strong>Heartbeat</strong> caught up with Julie Thompson,<br />
Director of Nursing, Medicine and<br />
Emergency Care who told us more.<br />
“Mouth Care Matters is a guide seeking to<br />
improve the oral health of inpatients. Poor<br />
oral health of a hospitalised patient can<br />
result in an increase in hospital-acquired<br />
infections, namely hospital and ventilator<br />
acquired pneumonia, as well as poorer<br />
nutrition. This can result in an increase<br />
in the length of stay and care costs,<br />
alongside poorer quality of life and dignity<br />
for patients.<br />
“This pilot focuses on reducing the rates<br />
of hospital-acquired pneumonia (HAP).<br />
Evidence shows a clear link between a<br />
Staff Nurse, Rachel Paintin with some of the oral<br />
care products<br />
good individualised mouth care regime and the<br />
reduction in the development of HAP.”<br />
Colleagues have welcomed and supported<br />
the trial. Practice Development Nurse, Grace<br />
Omoleye told <strong>Heartbeat</strong>: “It’s important<br />
for patients to feel whole and to not feel<br />
uncomfortable about their mouths when visitors<br />
come.<br />
“The products that we use keep the mouth and<br />
gums moist so prevent sores and infections. I<br />
really like the lip gloss for that reason. Some<br />
patients need to have their teeth cleaned<br />
whilst using the suctioning tool. This is so good<br />
because you use one tool that brushes, cleans<br />
and suctions the debris away at the same time.”<br />
Grace continued, “The products are single-use<br />
only and are specially packaged so they can<br />
stay by the patient’s bedside and not a risk from<br />
an infection prevention perspective. It means<br />
that they are easily to hand when you need<br />
to perform mouth care as part of the patient’s<br />
routine. Mouth care really does matter for our<br />
patients and we should all be helping them to<br />
have healthy mouths.”<br />
Since the project started, visitors have<br />
commented on the improvement of their<br />
loved ones mouth condition.<br />
One family member (a dentist) explained how<br />
his mother had a stark contrast of attitude<br />
towards mouth care while she had been in<br />
hospital on two different occasions. He said,<br />
“My mother was admitted to a different<br />
hospital a few years ago. A few days after she<br />
was admitted, I noticed that her teeth had not<br />
been cleaned and the condition of her mouth<br />
had deteriorated significantly. Despite raising<br />
these concerns with staff, I had to buy several<br />
oral products and come into the hospital<br />
twice a day to clean her teeth and mouth.<br />
“I was shocked that mouth care was not<br />
automatic and didn’t form part of a daily<br />
general hygiene routine. Mouth care is<br />
important because if my mum has poor oral<br />
care then she won’t be able to eat well and<br />
then can’t get well.<br />
“The first thing I noticed when mum was<br />
admitted to Priory 4 was the mouth care<br />
posters promoting the use of the products<br />
with an appropriate care plan. I felt confident<br />
that my mum would receive a good level of<br />
care as a result.”<br />
The results from HAP and other data will be<br />
analysed during April and recommendations<br />
and learnings will be shared with the<br />
executive team. The plan is to roll out the<br />
programme across the organisation.<br />
Six weeks into the trial rates of HAP<br />
remained lower than the mean rate and all<br />
the pilot wards have at least halved their<br />
incidence of HAP. Average length of stay<br />
has reduced from 18 to 11 days.<br />
Sarah Peyton: Over 33 years of success<br />
Sarah Peyton, Acute Medicine Nurse<br />
Practitioner will be retiring from the<br />
Trust after dedicating over three<br />
decades to the Trust and hospital care.<br />
Sarah first began her journey at our Trust<br />
in 1987. Over years she gradually built up<br />
her career to become a ward sister which<br />
was shortly followed by her promotion to<br />
an acute medicine nurse practitioner in<br />
July 2007.<br />
Sarah has played an instrumental role<br />
alongside Dr Sarb Clare, Consultant<br />
Physician in Acute Medicine in setting<br />
up a GP area which then changed to<br />
the AMAA (acute medicine ambulatory<br />
assessment) in 2014. As a result, Sarah,<br />
Sarb and the rest of the team went on be<br />
awarded the International Award from the<br />
Society of Acute Medicine for their work<br />
in AMAA.<br />
Sarah Peyton celebrates her three decade<br />
career at the Trust<br />
Reflecting on her career, she remarked,<br />
“What I’m most proud of is my day-to-day<br />
work on the medical wards and working in<br />
AMAA. The job has changed over time, but I<br />
feel I have adapted to the changes whilst still<br />
being able to offer the best quality of care to<br />
our patients.”<br />
Sarb believes Sarah has played a vital<br />
role at the Trust and in particular AMAA.<br />
She said, “Sarah has left a legacy for the<br />
organisation from developing and leading<br />
on nurse-led weekend discharges to<br />
being pivotal in developing and making<br />
ambulatory care a success. Her work has<br />
been invaluable and endless for both<br />
patients and colleagues.<br />
“She is well-known by generations of both<br />
nurses and doctors and has supported<br />
many young doctors over the years. Sarah<br />
is loved by everyone.”<br />
Upon retirement Sarah is planning to visit<br />
Africa as well as a Caribbean cruise with<br />
her family. She also hopes to visit Nepal<br />
again as she sponsors a little girl to go to<br />
school there.<br />
Thank you for your hard work at the<br />
Trust Sarah – happy retirement!<br />
22
Poo is no longer a taboo thanks<br />
to service<br />
It’s normally a taboo subject saved<br />
for discussions with your doctor or<br />
your most trusted friend or even<br />
keeping it entirely to yourself<br />
for fear of embarrassment. Not<br />
any more - the FINCH (Faecal<br />
INcontinence and Constipation<br />
Healthcare) team are bringing the<br />
embarrassing subject of poo into<br />
the open – highlighting the issue on<br />
national airwaves.<br />
Lead Clinical Nurse Specialist, Kelly<br />
Stackhouse and her team were the<br />
focus of the Radio 4 programme Inside<br />
Health interviewed by Trust Me I’m a<br />
Doctor presenter, Dr Saleyha Ahsan.<br />
The programme is known for discussing<br />
health issues which people struggle to<br />
understand and faecal incontinence<br />
(also known as bowel function) is<br />
certainly one of those topics.<br />
The service is for patients who have<br />
functional bowel disorders, which<br />
means the organ doesn’t work<br />
properly, leading to problems such<br />
as constipation, needing to rush to<br />
the toilet, losing control of the bowel<br />
following surgery in that area.<br />
Kelly explained, “The FINCH service<br />
wants to break the taboo around poo.<br />
Receiving this national coverage is very<br />
important as it will alert people to this<br />
vital service and raise awareness that<br />
there are different treatments available.<br />
We are here to help those who are<br />
experiencing real problems. Some of<br />
them will refuse or be unable to leave the<br />
house because it has gotten so bad. Many<br />
of our patients have told us how it really has<br />
changed their lives for the better being under<br />
the care of our service.”<br />
Set up a little over 10 years ago, the team<br />
initially comprised of just Kelly and one<br />
consultant Miss Kathryn Gill. Kelly had<br />
worked as a colorectal nurse at the Trust.<br />
She explained, “Miss Gill wanted to set up a<br />
service, so we did this together, with one of<br />
the main focuses being on anterior resection<br />
syndrome.<br />
Fast forward to <strong>2020</strong>, and the service has<br />
won a number of accolades. It comprises of<br />
three extra nursing team members and two<br />
more colorectal consultants. In 2019 it had<br />
500 referrals, compared to just 170 in its first<br />
year.<br />
“We hold clinics every day and patients from<br />
all over the country visit us,” Kelly added.<br />
One such patient is Lara Simms. The 21-yearold<br />
student started suffering from terrible<br />
constipation two years ago and was only able<br />
to pass a stool once every three weeks.<br />
Lara’s story was featured on the Radio 4<br />
programme. She told the presenter: “It<br />
transpired that I had ‘slow bowel’ and it<br />
had come on all of a sudden. I found myself<br />
suffering from terrible stomach pain and I<br />
was constantly in and out of the hospital in<br />
Brighton where I'm a student. Doctors were<br />
baffled as to what was wrong with me.”<br />
Eventually, she received a diagnosis but<br />
medics unfamiliar with the condition were<br />
unable to treat the problem effectively. “I was<br />
SURGICAL SERVICES<br />
on 15 to 20 laxatives a day and looked<br />
so bloated. I couldn’t go out because I<br />
knew I would need to use the toilet so<br />
much,” she said. Lara visited her family<br />
home frequently and on one occasion<br />
she was admitted to Sandwell Hospital<br />
and referred to the FINCH team.<br />
Kelly discussed Lara's condition with<br />
her colleagues at the multi-disciplinary<br />
team meeting. She was told about the<br />
antegrade continence enema (ACE)<br />
procedure – an operation designed to<br />
help with emptying the bowel. It allows<br />
the patient to self-administer enemas<br />
into the large bowel after a hole is<br />
made in the appendix. Lara became<br />
the first patient at our Trust to have<br />
this procedure, performed by Mr Raj<br />
Peravali.<br />
Lara added: “Since having this<br />
operation my life has changed<br />
drastically for the better. I am able to<br />
carry on with my studies, go out and<br />
see my friends, go shopping without<br />
having to worry about where the<br />
nearest toilet it. I have the FINCH team<br />
to thank for this.”<br />
To contact the FINCH team email<br />
swb-tr.SWBH-GM-FINCH@nhs.net.<br />
To listen to the full interview on<br />
Radio 4 go to https://www.bbc.<br />
co.uk/programmes/m000gbft<br />
Trust Me I’m a Doctor presenter Dr Saleyha Ahsan (far right) with Raj Peravali, Colorectal Consultant Surgeon, and nurses from the FINCH team Liz<br />
Clarson (second left) and Kelly Stackhouse (third left). The team were interviewed for the Radio 4 programme Inside Health which was aired on 10 <strong>March</strong>.<br />
23
National campaign to bust myth<br />
around eye drops<br />
SURGICAL SERVICES<br />
Some of our clinicians have featured<br />
in a hard-hitting campaign to<br />
highlight the importance of glaucoma<br />
patients taking eye drops during<br />
Ramadan.<br />
This campaign organised by the International<br />
Glaucoma Association (IGA) created a mythbusting<br />
video that features a number of<br />
clinicians from the Birmingham and Midland<br />
Eye Centre (BMEC). It highlights how<br />
Muslims using eye drops during Ramadan<br />
will not break their fast as the medication<br />
does not count as food or drink.<br />
Glaucoma is a group of eye conditions in<br />
which the main nerve to the eye (the optic<br />
nerve) is damaged where it leaves the back<br />
of the eye. As it becomes damaged, vision is<br />
lost, usually starting around the edge of the<br />
field of vision known as peripheral vision.<br />
There are no early symptoms of glaucoma,<br />
so up to 40 per cent of the peripheral vision<br />
can be lost without an individual noticing.<br />
Abdul-Jabbar Ghauri, Consultant<br />
Ophthalmologist with Head of Patient Support<br />
Services, International Glaucoma Association<br />
The most common treatment for glaucoma is to<br />
take eye drops. Depending on the type of eye<br />
drops, these may need to be taken every day and<br />
sometimes two or three times a day.<br />
Mr Abdul-Jabbar Ghauri, Consultant<br />
Ophthalmologist, said, “Eye drops should be taken<br />
throughout the month. According to most legal<br />
schools, the medication is not considered to break<br />
the fast, even if traces of taste or colour reach the<br />
back of the throat. For those people who aren’t<br />
convinced and can still taste the drop, they can<br />
try punctal occlusion. Most scholars would agree<br />
that eye drops do not count as food or drink. Islam<br />
forbids any act which is harmful to an individual.<br />
All Muslims should take care of their bodies,<br />
entrusted to them by God.<br />
“It is really important that we get the message<br />
out there that taking eye drops, or any<br />
medication for long-term illnesses is vital. Eye<br />
drops need to be taken every day in a range<br />
of eye conditions, including glaucoma and<br />
inflammatory eye disease. Even stopping the<br />
drops for a short time can cause permanent<br />
damage to a person’s vision and they may not<br />
notice any damage until their next check-up and<br />
field test.<br />
“We know Ramadan can be a busy time, so we<br />
recommend that patients leave their drops in a<br />
prominent place, such as by their toothbrush.<br />
Putting a reminder on a phone is also a good<br />
way to remember to take them.”<br />
As well as Mr Ghauri, other BMEC colleagues<br />
in the video include Emadur Khan, Specialist<br />
Optometrist, Andrew Castle, Specialist<br />
Orthoptist, Stephen Khaw, Senior Pharmacist<br />
and Iyad Ibrahim, Nurse Practitioner.<br />
Birmingham Central Mosque’s Imam,<br />
Mohammad Asad, and Joanna Bradley, Head of<br />
Patient Support Services for IGA also feature.<br />
New group to support myeloma<br />
patients<br />
Not so uncommon, but often diagnosed<br />
late, myeloma is an incurable but<br />
treatable form of blood cancer found in<br />
the bone marrow. It impacts thousands<br />
of people across the UK and accounts<br />
for 15 per cent of all blood cancers.<br />
A newly formed support group will soon be<br />
launching to support myeloma patients. The<br />
Midland Metropolitan Myeloma Support<br />
Group (MMMSG) officially launches on 22<br />
April. It will provide a broad array of support<br />
ranging from patient and carer information,<br />
living with myeloma and treatment options<br />
to name but a few things.<br />
The inaugural meeting will take place at<br />
the education centre at Sandwell Hospital.<br />
Patron, Dr Farooq Wandroo, Haematology<br />
Consultant commented, “MMMSG is a new<br />
myeloma patient support group established<br />
with the help of registered charity Myeloma<br />
UK. Over the years, we have been feeling<br />
an unmet need to have something in place<br />
to support myeloma patients and their<br />
carers when they are newly diagnosed or<br />
post-chemotherapy.<br />
“It’s essential that there is support available<br />
to share information, experiences and<br />
Members of the Midland Metropolitan<br />
Myeloma Support Group committee<br />
expert advice. Information plays a vital role<br />
in helping individuals come to terms with<br />
a myeloma diagnosis and understanding<br />
treatment options. Over 17, 000 people<br />
in the UK have myeloma and, though the<br />
disease remains incurable, the majority of<br />
patients now live a pronged life with current<br />
treatments.<br />
“This group consists of several patients<br />
and carers who are very enthusiastic about<br />
meeting and supporting each other. Doctors<br />
and nurses will support the group by<br />
providing advice on treatments available,<br />
management of pain, toxicities and<br />
measures to help myeloma patients live<br />
life to the fullest. The group will also<br />
help spread awareness about myeloma<br />
and promote early diagnosis to help<br />
prevent complications. It will also be<br />
working closely the Trust’s cancer<br />
services team.”<br />
Jane Ogleby, Macmillan Haematology<br />
CNS said: “We’re looking forward to<br />
the launch of the MMMSG; it will offer<br />
a great way for patients and family<br />
members to meet in an informal and<br />
welcoming setting. It will provide<br />
those living with myeloma lots of<br />
useful resources and access to trained<br />
professionals. It will also offer specialist<br />
support to help individuals deal with<br />
everything from their diagnosis through<br />
to more practical tips on how to<br />
navigate life with myeloma. As well as<br />
this individuals will benefit from support<br />
from each other as well as carers.”<br />
If you’d like to find out any<br />
more information, please email<br />
jane.ogleby@nhs.net.<br />
24
Inside the mortuary – taking care of<br />
our patients right to the end<br />
Jessica Arnold, Mortuary Service Manager is one of five colleagues who perform post-mortems at<br />
our Trust<br />
When many of us think of a mortuary<br />
we are filled with dread and fear often<br />
imagining what it must be like to be<br />
surrounded by death. However, when<br />
you meet our colleagues who work<br />
in the mortuary at City and Sandwell<br />
it is somewhat reassuring to see that<br />
the mortuary is a calm, even homely<br />
looking place aimed at making loved<br />
ones feel at ease during the most<br />
difficult time of their lives.<br />
<strong>Heartbeat</strong> caught up with our Mortuary<br />
Service Manager, Jessica Arnold who told<br />
us more. “People often have<br />
misconceptions about the mortuary and<br />
what we do – our aim is simple – patient<br />
care. We look after patients who have<br />
passed away and ensure they are taken care<br />
of until they leave for a burial or cremation.<br />
We can deal with very emotive cases<br />
but the team are here because they are<br />
compassionate and caring.”<br />
We asked Jessica to explain the flow of a<br />
patient leaving the ward and going into the<br />
care of the mortuary.<br />
She said: “When our patients are brought<br />
down by portering colleagues, part of our<br />
role is to check their paperwork is in order.<br />
We check that the patient has the correct<br />
ID and that all their personal belongings are<br />
accounted for. Patients are also measured as<br />
part of the requirement for the undertakers<br />
who require the measurements in order<br />
to prepare the coffins. There is a beautiful<br />
handwritten register where we write the<br />
patient’s name, date of death and the name<br />
of the undertaker. The information is also<br />
recorded electronically.”<br />
Five technicians make up the team in the<br />
mortuary who all take part in undertaking<br />
post mortems. Jessica explained that not all<br />
patients have a post mortem and it depends<br />
on whether the cause of death is known.<br />
“Post mortems are usually carried out if a<br />
patient dies unexpectedly,” said Jessica. “The<br />
process is meant to piece the puzzle of how<br />
someone died. Our coroner’s jurisdiction has<br />
access to a digital autopsy which is situated<br />
at Sandwell crematorium; it is a scanner that<br />
helps to ascertain the cause of death limiting<br />
the need for invasive procedures. In some<br />
cases the scan can be inconclusive so we have<br />
to carry out a full invasive post mortem.<br />
“As technicians we remove all the organs in<br />
preparation of dissection and examination by<br />
the pathologist. This can sometimes result in<br />
further examination where blood and urine is<br />
collected for further testing in the lab. Once<br />
it is clear how a patient has died, the coroner<br />
can issue the necessary paperwork for a<br />
funeral to take place.”<br />
It’s hard to imagine what it must be like<br />
having to deal with patients who have lost<br />
their lives and their families.<br />
Kulwinder Johal, Clinical Directorate Lead has<br />
recently taken on the overall management of<br />
the mortuary. She said: “Dealing with people<br />
in a bereaved status is very challenging. I am<br />
in awe of how the team take care of our<br />
patients as well as manage the expectations<br />
of loved ones.<br />
PRIMARY CARE, COMMUNITIES<br />
AND THERAPIES<br />
“They often have to have sensitive<br />
conversations with families to prepare<br />
them about what to expect when they<br />
see their loved one.”<br />
Jessica added: “We are not a funeral<br />
home so we are limited as to what we<br />
can do to prepare patients for viewing.<br />
But we do ensure that hair is brushed<br />
or combed and that the eyes and<br />
mouth are shut. The aim is to give the<br />
impression that the patient is sleeping<br />
so we lay them on a viewing trolley that<br />
looks like a bed.”<br />
Kulwinder aims to raise awareness of<br />
the mortuary service and the amazing<br />
work they do. “I don’t think colleagues<br />
around the organisation fully understand<br />
the work and skill that goes into caring<br />
for deceased patients,” she said. “We<br />
have just gone through a Human Tissues<br />
Authority (HTA) inspection and there<br />
is a lot of structure and accountability<br />
required to run a mortuary service.<br />
“We have worked together with our<br />
colleagues including clinical nurse<br />
practitioners, bereavement support<br />
midwives and ward managers as part<br />
of a stakeholder group involved with<br />
the deceased to achieve the standards<br />
of the HTA and deliver a coordinated<br />
approach to the way we care for<br />
deceased patients.<br />
“Together we work to ensure patients<br />
are laid to rest quicker and we also<br />
provide training particularly for the rapid<br />
release process. The rapid release process<br />
ensures that a death certificate is signed<br />
on the ward at the time of death (if<br />
cause is known). A signed form is issued<br />
to the family who will give authority for<br />
the body to be released. The patient is<br />
then escorted to the mortuary by a ward<br />
colleague and handed over straight to<br />
the undertaker. When done right, rapid<br />
release can take up to four hours and is<br />
a great comfort for families as they can<br />
lay their loved ones to rest.”<br />
Jessica commented: “Part of the work of<br />
the stakeholder group is also to ensure<br />
families are supported throughout the<br />
process and where necessary direct<br />
them to services that provide financial<br />
support.”<br />
If you would like further information<br />
or training please contact Jessica on<br />
jessica.arnold3@nhs.net<br />
25
Gynaecology celebrates first birthday!<br />
WOMEN AND CHILD HEALTH<br />
Our Sandwell based gynaecology<br />
team celebrated their first birthday in<br />
February.<br />
The celebration represented a year since<br />
the department moved from Alpha Suite<br />
to clinic 6A which is a part of the main<br />
outpatients’ area at Sandwell Hospital. The<br />
gynaecology unit specialise is addressing,<br />
correcting and easing any gynaecological<br />
issues our female patients experience.<br />
For some of our patient's gynaecological<br />
issues can have a catastrophic effect on<br />
their daily life. With this in mind, the team<br />
help patients to rectify these complex<br />
issues.<br />
“Thanks to the move we have been<br />
able to increase our capacity. It is an<br />
exciting time for further growth. We<br />
are working hard to modernise one<br />
service, in particular, to offer a one-stop<br />
clinical experience for women with postmenopausal<br />
bleeding,” said Tiffany Jones,<br />
Sister.<br />
In addition, the gynaecology team have<br />
also been able to commit to achieving<br />
faster treatment times for women that<br />
receive an endometrial (womb lining)<br />
cancer diagnosis.<br />
Charlotte Gordan, HCA in gynaecology kindly<br />
made the first birthday cake<br />
The special birthday event was attended by<br />
colleagues who work within gynaecology,<br />
including Dr Abha Sinha, Consultant<br />
Gynaecologist and Obstetrician, CD. Dr Sinha<br />
believes the success of the move has been<br />
down to all the colleagues who work within<br />
the team. Tiffany has proven instrumental to<br />
the department, as have her core team made<br />
up of Vanessa Wright, Sara Greenaway, Jean<br />
Whitehouse, Tracey Law, Jenny Oliver, Charlotte<br />
Gordon, Donna Francis, Julie Hill and Cynthia<br />
Daly.<br />
The team also benefits from being supported<br />
in times of pressure by Paula Bryan and her<br />
team from gynaecology outpatients’ in the<br />
Birmingham Treatment Centre. She said, “I<br />
have to express my huge admiration for Tiffany<br />
for her leadership skills, as well as her clinical<br />
and interpersonal skills in leading an amazing<br />
team. She has worked incredibly hard over<br />
the past 12 months to get the unit staffed<br />
with the best HCA team. She’s also trained<br />
and supported them to develop into band 3-4<br />
roles.”<br />
Raffaela Goodby, Director of People and<br />
Organisation Development has been a patient<br />
and has participated in multiple board visits<br />
to the department. A real advocate of the<br />
team and the work they do, she said, “Not<br />
many patients can say that their gynaecology<br />
visits are like visiting a spa. I can say that my<br />
experience as a patient and as a colleague has<br />
been zen from start to finish!<br />
“Tiffany and the team calmly and simply<br />
explain very intimate procedures and give you<br />
assurance and honesty at a very worrying<br />
time. When I had treatment last year to<br />
have pre-cancerous cells removed, the team<br />
explained what was happening and I didn’t<br />
feel embarrassed or ill at ease once. That’s an<br />
achievement considering the intimacy of the<br />
situation."<br />
She added, “I want to offer my thanks to<br />
the team for all they do for patients, and for<br />
having that person-centred approach I know<br />
they offer to each patient. Thank you for<br />
being so open about women’s reproductive<br />
health, for openly talking about the<br />
importance of smear tests, and for looking<br />
after the gynaecological health of Sandwell<br />
and West Birmingham with such composure.”<br />
Baby Gibson first to benefit from<br />
patient generosity<br />
Two-day-old, Kade Gibson was<br />
keen to show off his latest knitwear<br />
thanks to the kindness of former<br />
patient, Julita Dirsaite.<br />
Julita was in our maternity department<br />
two and a half years ago and after the<br />
fantastic care she received whilst at the<br />
Trust, she made the decision she wanted<br />
to give back to the nurses and midwives<br />
at the hospital.<br />
Being an enthusiastic knitter and the<br />
drive to help others, Julita decided she<br />
wanted to knit clothes for one of our<br />
most vulnerable group of patients and<br />
those just starting out in life, premature<br />
babies. Items included tiny knitted<br />
converse boots, ballerina shoes, flower<br />
blankets and bonnets. As well as knitting<br />
for the little babies, she also knitted<br />
a few accessories for our midwives<br />
including pen pots to store stationary as<br />
Baby Kady Gibson shows off his new knitted<br />
gear<br />
gifts for their continued hard work in the<br />
department.<br />
Claire Cushing, M2 Ward Manager is one of<br />
many colleagues to get a gift from Julita and<br />
believes the donations from her will really<br />
help our patients.<br />
She said: “We were overwhelmed with<br />
the donations from Julita and very much<br />
appreciate them all in our department. All<br />
the clothes, booties and blankets that have<br />
been knitted will really benefit the babies in<br />
maternity and their parents.”<br />
Amanda Winwood, Fundraising Manager at<br />
Your Trust Charity facilitated the knitwear for<br />
maternity and echoes Claire’s views.<br />
She said: “Unfortunately we have many<br />
mums who struggle to get hold of clothing<br />
for their premature babies, but by having<br />
our community support us in making such<br />
beautiful gifts and giving their time allows<br />
us to support our patients in the very early<br />
days. Julita’s gifts tie in perfectly with it being<br />
Year of the Nurse and Midwife <strong>2020</strong>, and<br />
showing how appreciated they are.”<br />
Angela Jane Gibson, mum of Kade Gibson<br />
was thankful for the donation and said, “It<br />
was really kind of the charity and hospital<br />
to provide Kade with a set of knitwear and<br />
booties when he was born.”<br />
She added: “I must say a massive thank you<br />
to both as well as a special thanks to Julita<br />
for knitting them.”<br />
26
Safer Sleep Week to help prevent<br />
unexpected deaths of little ones<br />
Early <strong>March</strong> marked Safer Sleep Week<br />
an annual campaign spearheaded by<br />
The Lullaby Trust, whose vision is to<br />
reduce and prevent where possible the<br />
unexpected deaths of babies and young<br />
children.<br />
The Lullaby Trust actively fund research into<br />
both the causes and prevention of sudden<br />
infant death syndrome (SIDS). They also<br />
provide support to parents and engage with<br />
medical professionals to help promote child<br />
health.<br />
With approximately 700,000 babies born<br />
every year in the UK, the focus of this year’s<br />
campaign was to provide practical tips to<br />
help new parents survive sleep deprivation.<br />
The Safer Sleep Week campaign was<br />
enthusiastically embraced by our<br />
community maternity team. The team<br />
shared tips to equip parents with the<br />
knowledge to establish safe sleep routines.<br />
This included having a Moses basket set<br />
up to demonstrate both the correct and<br />
incorrect way to put a baby to sleep. The<br />
team were also on hand to answer any<br />
Michelle Defreitas from the community midwives<br />
team held sessions with new parents during<br />
Safer Sleep Week<br />
questions and, they had a display of posters<br />
and leaflets available too.<br />
Speaking to <strong>Heartbeat</strong>, Dionne Mullings,<br />
Community Team Manager said, “We’re<br />
passionate supporters of Safer Sleep Week.<br />
We aimed to reach all of our new parents<br />
with some key messages to help to reduce the<br />
risk of SIDS occurring. Sleep deprivation can<br />
WOMEN AND CHILD HEALTH<br />
be hard for new parents to adjust to, but<br />
we’re here to help. We have a vast array<br />
of experience on the team and, between<br />
us we wanted to reinforce the message<br />
that it’s important to establish safer sleep<br />
routines early on.”<br />
Safer sleeping – things you can do<br />
• Always place your baby on their<br />
back to sleep<br />
• Keep your baby smoke free during<br />
pregnancy and after birth<br />
• Breastfeed your baby<br />
• Place your baby to sleep in a<br />
separate cot or Moses basket in<br />
the same room as you for the first<br />
six months<br />
• Use a firm, flat, waterproof mattress<br />
in good condition.<br />
Did you know that you can download<br />
treatment-specific patient information<br />
leaflets from the EIDO Healthcare<br />
website for FREE?<br />
EIDO has hundreds of patient leaflets for different procedures that<br />
are being carried out across the Trust.<br />
They are available in an easy-to-read format and<br />
in different languages.<br />
Patient information for hundreds of procedures carried out across<br />
the Trust can be downloaded for free and passed on to patients<br />
to help them better understand the procedure they may be<br />
undergoing. Many of these are available in different languages and<br />
formats and help patients to give informed consent.<br />
Visit Connect Clinical Systems EIDO PT Leaflets.<br />
For more information, please contact Communications Team on<br />
ext.5303 or email swbh.comms@nhs.net<br />
27
Is it a bird? Is it a plane?<br />
No, it’s a CT scanner<br />
IMAGING<br />
This month the imaging team at<br />
City Hospital played host to an army<br />
of high-vis clad engineers from<br />
Siemens Healthineers who delivered<br />
the newest addition to the imaging<br />
department at the Birmingham<br />
Treatment Centre (BTC), the new<br />
computerised tomography (CT)<br />
scanner.<br />
Amongst the beeping fanfare of a crane,<br />
engineers carefully peeled away the side<br />
wall of the BTC, constructed a reinforced<br />
platform and gently lifted, manoeuvred<br />
and landed the huge scanner onto the<br />
first floor to then be delicately pushed to<br />
its new home in the imaging department.<br />
CT scanners are innovative scanners<br />
that create cross sectional images of the<br />
body by rotating an x-ray machine round<br />
the body and then use a computer to<br />
reconstruct the multiple images into a<br />
single three-dimensional image that lets<br />
doctors look inside the body. Commonly,<br />
CT scanners diagnose infections, fractures<br />
and muscle disorders, as well as helping<br />
to pinpoint masses and tumours. They<br />
are sometimes even used to help guide<br />
surgical procedures and biopsies.<br />
To find out more about the scanner,<br />
<strong>Heartbeat</strong> caught up with Phil Spencer,<br />
Superintendent Radiographer and CT<br />
Lead at our Trust. He said, “The newest<br />
scanner we have had delivered is now the<br />
fifth CT scanner we have at our disposal.<br />
We have two at Sandwell and three at<br />
City. This gives us plenty of resources offer<br />
imaging support at short notice, as well<br />
as resilience, should one of the scanners<br />
need to be repaired.”<br />
The newest addition to the imaging team’s<br />
arsenal<br />
Trust bowel-ed over by national<br />
cancer audit results<br />
The National Bowel Cancer Audit<br />
publishes results about the care<br />
and outcomes of patients with<br />
bowel cancer in England and Wales.<br />
Commissioned by the Healthcare<br />
Quality Improvement Partnership as<br />
part of the National Clinical Audit<br />
and Patient Outcomes Programme,<br />
this quality improvement programme<br />
has been running for several years.<br />
It is delivered jointly by the Clinical<br />
Effectiveness Unit at the Royal College<br />
of Surgeons of England, NHS Digital,<br />
and the Association of Coloproctology<br />
of Great Britain and Ireland.<br />
Each year, a report is produced for trusts<br />
in England and multidisciplinary teams in<br />
Wales. Our most recent results published<br />
for 2017-2018 show that we included<br />
more patients than expected and we<br />
performed positively in several areas.<br />
Mr Torrance, Colorectal Consultant<br />
remarked, “Our data collection is<br />
significantly better than it has been in<br />
the past and that has allowed us to share<br />
that we are performing above average<br />
compared to our local peers and nationally<br />
in most measures. We stood out in the rate<br />
of major surgery performed in potentially<br />
curative patients. Whilst the national score<br />
was 86 per cent, we scored 92 per cent<br />
– 6 per cent above the national average.<br />
We also perform significantly more cases<br />
through keyhole surgery compared to<br />
the rest of the country, with 89 per cent<br />
attempted through keyhole surgery<br />
compared to 69 per cent nationally. When<br />
we combined this with our enhanced<br />
recovery programme supported by our<br />
anaesthetic colleagues, ward staff and<br />
clinical nurse specialist team, we have<br />
helped nearly half of patients go home<br />
within 5 days of major surgery compared to<br />
the national average of just over a third of<br />
patients.”<br />
When discussing how we’ve achieved<br />
these results, Dr Torrance commented,<br />
“We have invested in our data and<br />
wanted to show just how well we’re<br />
performing as a Trust. We now have<br />
a dedicated person responsible for<br />
managing our data. Tahira Sani from our<br />
cancer services team has done a great job<br />
at collating all of our data and allowing us<br />
to show just how well we’re performing,<br />
both regionally and nationally.”<br />
Speaking to <strong>Heartbeat</strong>, Tahira<br />
commented, “I have taken on the task of<br />
compiling our clinical data. This involves<br />
collating data from lots of different<br />
sources including systems and meeting<br />
notes. I was pleased to see how well we<br />
performed as a Trust in comparison to<br />
others locally and nationally.”<br />
28
This month we say hello to Liam<br />
Kennedy. As you’ll likely know, Liam<br />
isn’t new to our Trust; however, he has<br />
recently moved from being our deputy<br />
chief operating officer to become our<br />
chief operating officer (COO).<br />
Having started his career as a science<br />
teacher, Liam joined the NHS nine<br />
years ago as part of the NHS graduate<br />
management training scheme. Reflecting<br />
on his decision to join this scheme, Liam<br />
remarked, “This was a defining career<br />
moment for me. I developed the skills<br />
to help me lead different functions and<br />
teams across several trusts. I have worked<br />
in project management, accounting and<br />
transformation positions, as well as a<br />
group manager in medicine, surgery and<br />
community services.”<br />
Liam completed a six-month placement<br />
with Monitor; a regulatory body that<br />
was responsible for ensuring healthcare<br />
provision in NHS England was financially<br />
effective. As well as this, he has completed<br />
a management accounting qualification<br />
via the Chartered Institute of Management<br />
Accountants and a PgCert in healthcare<br />
leadership and management.<br />
Liam Kennedy, Chief Operating Officer<br />
You may be surprised to learn that Liam has<br />
not always worked in healthcare. Before<br />
joining the NHS, Liam had a varied career.<br />
Aside from being a teacher, he also worked<br />
as a celebrity account manager and revealed<br />
that Peter Andre was the most famous<br />
person he ever booked for an event.<br />
Looking to the future as our COO, Liam has<br />
Liam Kennedy<br />
Chief Operating Officer<br />
some key areas of interest he’ll be focusing<br />
on. “Digital implementation into the NHS<br />
is a passion of mine. So far, I’ve worked<br />
across the Unity project and introduced<br />
digital dictation. I’ll be working closely with<br />
teams to ensure we’re giving our clinical<br />
colleagues the tools they need to deliver the<br />
best patient care. Digital transformation will<br />
help us offer a more efficient and patientfocused<br />
service.<br />
“I’ll be looking at improving our urgent care<br />
standards and working with all directorates<br />
to ensure they have the data, skills and<br />
resources to deliver service improvements.<br />
As well as this, I’m keen to look at<br />
preventative measures to ensure we’re<br />
having early interactions with patients. We<br />
have lots of resources available to help them<br />
lead healthier lives.”<br />
Outside of work Liam enjoys keeping fit.<br />
This year he had planned an Ironman<br />
triathlon in Copenhagen that involves<br />
swimming, running and doing a bike ride<br />
all in support of Your Trust Charity. Excited<br />
about taking on the challenge, he said, “It’s<br />
going to be a test of endurance. I’ve started<br />
my training and go swimming before work.<br />
I’m looking forward to doing something<br />
that will directly give back to our Trust.”<br />
Wave goodbye to…<br />
Lis Hesk<br />
Matron – gynaecology and gynae oncology<br />
This month we bid adieu to Lis Hesk,<br />
Matron in gynaecology and gynae<br />
oncology. Having started her career in<br />
1982 in Leicester, Lis has had a long and<br />
varied career in nursing. In 1988, she<br />
completed her midwifery training at<br />
Queen Charlotte’s Hospital in London<br />
and has never looked back.<br />
Speaking to <strong>Heartbeat</strong> about her career,<br />
she said, “I have always been a nurse,<br />
I cannot imagine doing anything else. I<br />
started my training in 1982 before most of<br />
my staff were born! I have always worked<br />
in women’s health – it’s an area I feel<br />
incredibly passionate about.”<br />
Lis joined our Trust in 2012 as matron of<br />
gynaecology and gynae oncology. Over<br />
the years she’s had a number of career<br />
highlights including the implementation of<br />
Unity. Looking back on it she said, “This<br />
was a massive project that affected each<br />
member of the team. We had fantastic<br />
support within gynaecology; the team really<br />
Lis Hesk<br />
embraced the electronic patient record and<br />
it has had such a positive impact on the<br />
care we deliver.”<br />
Danielle Joseph, Deputy Group Director<br />
of Operations commented, “Lis is an<br />
exceptional nurse and leader. I’ve worked<br />
with her for some time now and have a<br />
huge amount of respect for her. Lis is caring<br />
and patient focused - something you need<br />
to be within gynae and gynae oncology.<br />
She is most definitely a team player,<br />
collaborative and always up for a challenge.<br />
Lis has been a pleasure to work with and<br />
we are all going to miss her greatly.”<br />
Looking ahead to the future Lis is planning<br />
on spending time with her family and<br />
friends. “I’ve not taken a day off sick<br />
since 1989 - I’ve never wanted to let my<br />
colleagues down. I will definitely enjoy<br />
some quality time with my loved ones when<br />
I retire.”<br />
Thank you for your hard work and<br />
dedication, Lis.<br />
29
Letters, of less than 200 words please, can be sent to the Communications Department,<br />
Trust Headquarters, Sandwell Hospital or by email to swb–tr.SWBH–GM–<strong>Heartbeat</strong>@nhs.net<br />
YOUR RIGHT TO BE HEARD<br />
Cleaning concerns at Trinity<br />
House<br />
Dear <strong>Heartbeat</strong>,<br />
Can you tell me why Trinity House<br />
has had there cleaning cut down<br />
to two days a week, Monday and<br />
Friday. It has been months since<br />
the offices have been vacuumed or<br />
floors cleaned, and now we have to<br />
go three days without the toilets or<br />
kitchens being cleaned.<br />
Trinity House as a lot visitors and<br />
would hate to think what they will<br />
think if rubbish is piled high. Come<br />
the summer we will have a smell<br />
from rubbish lying around for days.<br />
All I can say is that you would not<br />
leave your toilet/kitchen at home<br />
without cleaning it every day. I hope<br />
the Trust will take action on this<br />
as I believe that this low level of<br />
cleaning will lead to more people<br />
being of sick because of lack of basic<br />
cleaning.<br />
Regards,<br />
Anon<br />
Dear colleague,<br />
Cleaning arrangements at the<br />
Trust have changed. We are<br />
moving more of our cleaning<br />
time into our patient facing<br />
and clinical areas. And we<br />
are reducing expenditure in<br />
non-clinical areas by just over<br />
£100,000 a year.<br />
The schedules for cleaning have<br />
changed. What does this mean<br />
for you?<br />
• Just like before we need<br />
your help to make sure that<br />
communal areas, kitchens<br />
and toilets are usable and<br />
civilised. In simple terms if you<br />
create some “mess” please clean<br />
it up. If there are a real mess,<br />
maybe because someone has<br />
an accident, then that can be<br />
reported.<br />
• From now on, if your bin only<br />
fills up once a week it will be<br />
emptied by the WSO team. But<br />
if you want it emptied more<br />
regularly, please use one of the<br />
provided bin bags and drop<br />
off your bag into the large<br />
bins outside our entrances on<br />
your way home. Do not pile up<br />
bin bags outside offices or in<br />
communal areas.<br />
There are separate Trust wide<br />
comms on waste and recycling,<br />
and making sure we use the right<br />
bins for the right things, and fold<br />
cardboard into central storage<br />
areas. If you have not had chance to<br />
read through that, take a look on<br />
Connect.<br />
Working together we want to make<br />
working here a great experience.<br />
By moving around the money we<br />
have we are trying to invest in the<br />
right things, like more support for<br />
staff wellbeing, mental health,<br />
and exercise, as well as important<br />
changes for our environment,<br />
improving our gardens and tackling<br />
climate change. We hope you can<br />
support the changes made by doing<br />
your bit. The changes apply Trustwide<br />
in non-clinical areas – and that<br />
does include HQ and the “executive<br />
corridors”!<br />
Kind regards<br />
Toby Lewis<br />
Chief Executive<br />
Why am I being redeployed?<br />
Dear <strong>Heartbeat</strong>,<br />
I am being redeployed. I was told this<br />
in front of a colleague. Why have I<br />
been chosen? Surely there are risks for<br />
patients in moving people around from<br />
clinics to wards. Is it legal to do this and<br />
how can I be sure I won’t lose my PIN<br />
number?<br />
Very worried RGN<br />
Dear colleague,<br />
Thank you for your letter. I<br />
completely understand your<br />
concern at a time of both rumour<br />
and anxiety. We are going to have<br />
to re-deploy lots of colleagues and<br />
even those not moved in the first<br />
phase in April and May may be<br />
needed in the second phase in June.<br />
You will get some training but<br />
should only practice within your<br />
competence. You will get a new line<br />
manager and a buddy. And we will<br />
work with you once you start.<br />
I must apologise you were spoken<br />
to in front of someone else. Our<br />
standard is really clear - private<br />
conversations, an opportunity<br />
to raise concerns and to suggest<br />
reasonable adjustments. We need to<br />
work with you, and remember this<br />
is “a marathon not a sprint”. Get in<br />
touch if you remain concerned.<br />
Kind regards<br />
Paula Gardner, Chief Nurse<br />
30
Toby writes about… management by<br />
walking about<br />
TobyLewis_SWBH<br />
TOBY’S LAST WORD<br />
I have written eight COVID Updates<br />
@SWBHnhs. So far. I suspect there<br />
are more to come.<br />
Each time I am humbled by responses<br />
wishing me well, giving me advice,<br />
asking me questions, and reflecting the<br />
variety of individual experience we have<br />
as we face this pandemic together.<br />
The situation is moving fast. But<br />
it is also moving predictably. All of<br />
us tend to see our own situation as<br />
unique, but in truth Iran, Italy, Wuhan<br />
and Madrid all give us clues to what<br />
is ahead, as do Germany and South<br />
Korea. So, this is a chance to use<br />
evidence and learn lessons. That is true<br />
for governments, hospitals, countries<br />
and individuals. Thank you to those<br />
contributing their time to research trials<br />
and their wisdom to our ethics and<br />
advisory group.<br />
Now, here’s my point: There are plans,<br />
and revised plans, and plans to get<br />
plans - all the usual paraphernalia of<br />
management and large organisational<br />
systems.<br />
So what matters? Well obviously as<br />
many other articles in <strong>Heartbeat</strong> point<br />
out what matters is our patients,<br />
their loved ones, our colleagues and<br />
those we care most about. So the<br />
leadership task is not in truth measured<br />
in command centres, capacity or even<br />
PPE. Each of those things is vital. But<br />
none of those things will succeed<br />
unless we do something else –<br />
communicate better than we ever<br />
have, or ever have had to, before.<br />
I don’t mean send canny emails or<br />
film videos. I mean each person who<br />
leads, which might be someone who<br />
manages someone, or someone who<br />
inspires others as a peer, finding time<br />
with colleagues to make sense of what<br />
is going on. Where do you fit in? You<br />
might feel like a bystander, far from<br />
ED or ITU. You might feel exhausted,<br />
plunged into workforce models across<br />
AMU and our red wards that seemed<br />
impossible days ago. You might have<br />
exhaustion and exhilaration as you rush<br />
from one event to another webex.<br />
In all circumstances the challenge is to<br />
hear other’s confusion gently. To explain<br />
why choices have been made, carefully.<br />
To place our effort in the regional<br />
context, alongside the work of care home<br />
workers, police officers, PHL staff at<br />
Heartlands, and our peers at New Cross<br />
and across the Black Country. At the<br />
same time, the profound challenge must<br />
not cloak poor management practice.<br />
No amount of explaining makes sense<br />
of visor shortages. No amount of best<br />
intentions gives comfort at the death of<br />
someone we were unable to save.<br />
This article is about management by<br />
walking about. Tough when you can’t<br />
go everywhere! And when as a manager<br />
there is much you don’t know. Always<br />
easier to communicate certainty and talk<br />
about stuff you know. But now faced<br />
with a worldwide emergency is exactly<br />
when those people whose job, and career<br />
choice, is to coach other people, need<br />
to be forward about sharing what truths<br />
you know. Explain how the role of our<br />
ward service officers fit in. Explain who<br />
can work from home and why we need<br />
some people to move to hotels. Above all<br />
find a bit of space to hear what has<br />
been understood among the very<br />
many people we work with who<br />
do not access email or log onto the<br />
Connect system. An authentic voice<br />
who has tried to find PPE at 8.15pm<br />
on a Saturday night or has had to<br />
cancel a clinic of patients matters<br />
very much. You are just as much part<br />
of a frontline effort, alongside our<br />
bank office, and our porters.<br />
So if you are not sure how to<br />
contribute, or you are a manager<br />
and are free for a while to wander,<br />
let me ask you to find teams,<br />
explain again what you think<br />
everyone already knows, and<br />
give people some of your time to<br />
hear how folk feel. Our common<br />
purpose is all too obvious. We are<br />
facing a viral pandemic, where your<br />
care and attention for your own<br />
health, directly impacts my chance of<br />
survival. But we are each individuals<br />
and on different days we fear and<br />
face this challenge differently. So<br />
I need everyone who manages<br />
anyone to take just a little more time<br />
to work with our colleagues and<br />
make sure that we really are fighting<br />
this as one team.<br />
QUICK COVID-19 QUIZ – CAN YOU GET ALL 7 RIGHT?<br />
• How many seconds should you wash your hands for each time you do?<br />
• Which GP practices locally are the two local Hot COVID Primary<br />
Care Centres?<br />
• Which two surgical services have relocated from City to Sandwell to help<br />
us cope?<br />
• What is a blue ward?<br />
• Can you get free taxis with your hotel booking, yes or no?<br />
• How far apart should you be when socially distancing?<br />
• What’s the one word that we want to sum up our COVID-19<br />
response as Trust?<br />
There could be a prize. Email your seven to tobylewis@nhs.net and we’ll<br />
let you know.<br />
31
Charity launches fundraising<br />
campaign for Midland Met<br />
YOUR TRUST CHARITY<br />
hospital. It’s not just about caring for our<br />
community - it is about including them.”<br />
@SWBHCharity To donate<br />
to the Your Trust Charity text<br />
“SWBH16 £5” to 70070<br />
Your Trust Charity has officially<br />
launched a £2 million campaign<br />
to raise funds for the Midland<br />
Metropolitan University Hospital<br />
(MMUH).<br />
The campaign, called We Are<br />
Metropolitan, was launched in <strong>March</strong>.<br />
All of the cash raised will have one thing<br />
in common - it will positively impact the<br />
patient experience by funding research<br />
nurses, pharmacists and community<br />
spaces at the new facility.<br />
The state-of-the-art hospital will open<br />
in 2022 and boast the busiest accident<br />
and emergency department in Europe,<br />
serving 700,000 people across Sandwell<br />
and West Birmingham. Richard Samuda,<br />
our Chairman, said, “Besides our drive to<br />
make sure MMUH delivers the best care<br />
Guests received a special We Are Metropolitan<br />
brochure on arrival at the launch event as a<br />
memento.<br />
possible, our charitable appeal for funding<br />
enables the Trust to develop in parallel,<br />
important community outreach activities<br />
and research relevant to our patients'. We<br />
see this as key to making this more than<br />
a hospital build project. For us, it’s about<br />
contributing to the wider improvement in<br />
public health outcomes.<br />
“We want to ensure that those using our<br />
new hospital not only receive the best care<br />
possible, but also that their entire journey<br />
is seamless. We believe that by funding<br />
play areas for our young patients, creating<br />
a beautiful garden where people can sit<br />
and reflect, and hiring research nurses who<br />
will help to find treatment and cures for<br />
illnesses, we can help achieve this.”<br />
Mr Samuda went on to say, “The thinking<br />
behind the We Are Metropolitan campaign<br />
is to reflect that everyone within Sandwell<br />
and West Birmingham is part of this<br />
The local community and businesses<br />
across the region are being encouraged<br />
to support the campaign by donating to<br />
the fund by hosting events. Thrill-seekers<br />
can even take part in a bungee jump onsite<br />
in September.<br />
Paul Faulkner, Chief Executive of the<br />
Greater Birmingham Chamber of<br />
Commerce, is also Co-Chair for the<br />
campaign’s Business Committee. He<br />
said, “I am delighted to support this<br />
worthwhile campaign and would<br />
encourage the business community<br />
to get involved. The scale, ambition<br />
and impact of the hospital will be truly<br />
transformational for our region. We<br />
need the help of our local community to<br />
get to two million pounds by 2022. We<br />
want to make it more than a hospital,<br />
but that can only be achieved if we raise<br />
these vital funds."<br />
To help with the fundraising<br />
campaign contact Your Trust<br />
Charity on extension 5196, or email<br />
midlandmet@nhs.net.<br />
You can also make an online<br />
donation at https://donorbox.org/<br />
your-trust-charity.<br />
Sandwell and West Birmingham<br />
NHS Trust<br />
WE ARE<br />
METROPOLITAN<br />
<strong>March</strong> <strong>2020</strong> staff lottery results<br />
1st £188.75<br />
Lyndsey Hemsley<br />
2nd £113.25<br />
Usha Sund<br />
3rd £75.50<br />
Beverley Manners<br />
Don’t forget that Your Trust Charity lottery costs just £1 a month and anyone<br />
who works for the Trust can join. Payment is deducted from your wages each<br />
month. To take part email amanda.winwood@nhs.net.