Refractive Lens Surgery
Refractive Lens Surgery
Refractive Lens Surgery
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
94 S.J. Dell<br />
Fig. 10.8. Small capsulorrhexis helps ensure correct<br />
posterior vaulting of the Crystalens. A capsulorrhexis<br />
that is too large can allow anterior vaulting<br />
of the lens, while one that is too small<br />
complicates cortical removal and lens implantation,<br />
and tends to provoke an intense fibrotic reaction<br />
of the capsule<br />
ens are posteriorly vaulted in the correct position<br />
(Fig. 10.8). A capsulorrhexis that is too<br />
large can allow anterior vaulting of the lens,<br />
while one that is too small can lead to an overly<br />
aggressive fibrotic response of the posterior<br />
capsule as many more anterior lens epithelial<br />
cells are left in place. Very small<br />
capsulorrhexes have the added disadvantages<br />
of complicating cortical removal and delivery<br />
of the trailing plate into the capsular bag. Additionally,<br />
a very small capsulorrhexis may<br />
dampen accommodative movement of the<br />
optic by trapping the Crystalens in a fibrotic<br />
cocoon formed by fusion of the anterior and<br />
posterior leaves of the capsule. Surprisingly,<br />
proper capsulorrhexis sizing has been one of<br />
the more challenging aspects of the first few<br />
cases of surgeons transitioning to this lens.<br />
In general, the Crystalens provides excellent<br />
centration as a result of the polyimide<br />
loops at the termination of the plate haptics.<br />
Fixation of the polyimide loops occurs relatively<br />
early in the postoperative period and<br />
exchanging or repositioning the Crystalens<br />
can be difficult after approximately 4 weeks.<br />
The Crystalens cannot be dialed or rotated in<br />
a traditional fashion, as the four polyimide<br />
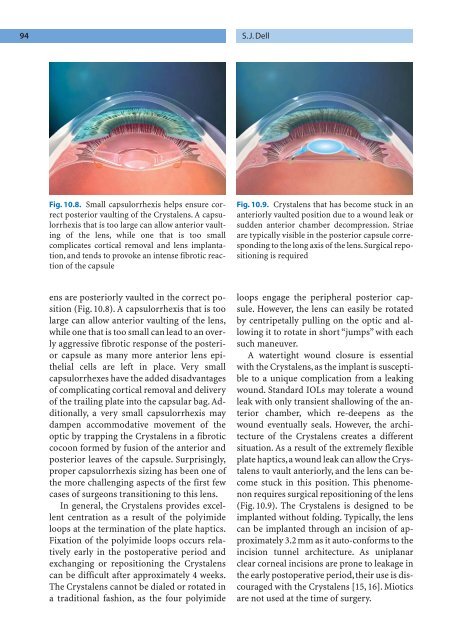
Fig. 10.9. Crystalens that has become stuck in an<br />
anteriorly vaulted position due to a wound leak or<br />
sudden anterior chamber decompression. Striae<br />
are typically visible in the posterior capsule corresponding<br />
to the long axis of the lens. Surgical repositioning<br />
is required<br />
loops engage the peripheral posterior capsule.<br />
However, the lens can easily be rotated<br />
by centripetally pulling on the optic and allowing<br />
it to rotate in short “jumps” with each<br />
such maneuver.<br />
A watertight wound closure is essential<br />
with the Crystalens, as the implant is susceptible<br />
to a unique complication from a leaking<br />
wound. Standard IOLs may tolerate a wound<br />
leak with only transient shallowing of the anterior<br />
chamber, which re-deepens as the<br />
wound eventually seals. However, the architecture<br />
of the Crystalens creates a different<br />
situation. As a result of the extremely flexible<br />
plate haptics,a wound leak can allow the Crystalens<br />
to vault anteriorly, and the lens can become<br />
stuck in this position. This phenomenon<br />
requires surgical repositioning of the lens<br />
(Fig. 10.9). The Crystalens is designed to be<br />
implanted without folding. Typically, the lens<br />
can be implanted through an incision of approximately<br />
3.2 mm as it auto-conforms to the<br />
incision tunnel architecture. As uniplanar<br />
clear corneal incisions are prone to leakage in<br />
the early postoperative period, their use is discouraged<br />
with the Crystalens [15, 16]. Miotics<br />
are not used at the time of surgery.