Refractive Lens Surgery
Refractive Lens Surgery
Refractive Lens Surgery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
22 J.T. Holladay<br />
4.1 Introduction<br />
The indications for intraocular lens (IOL)<br />
implantation following cataract or clear lensectomy<br />
have significantly increased. These<br />
expanded indications result in more complicated<br />
cases such as patients with a scleral<br />
buckle, silicone in the vitreous, previous<br />
refractive surgery, piggyback IOLs in nanophthalmos,<br />
positive and negative secondary<br />
piggyback IOLs and specialty lenses, such as<br />
multifocal and toric IOLs. Techniques for determining<br />
the proper IOL and power are presented.<br />
Several measurements of the eye are helpful<br />
in determining the appropriate IOL power<br />
to achieve a desired refraction. These measurements<br />
include central corneal refractive<br />
power (K-readings), axial length (biometry),<br />
horizontal corneal diameter (horizontal<br />
white to white), anterior chamber depth, lens<br />
thickness, preoperative refraction and age of<br />
the patient. The accuracy of predicting the<br />
necessary power of an IOL is directly related<br />
to the accuracy of these measurements [1, 2].<br />
4.1.1 Theoretical Formulas<br />
Fyodorov first estimated the optical power of<br />
an IOL using vergence formulas in 1967 [3].<br />
Between 1972 and 1975, when accurate ultrasonic<br />
A-scan units became commercially<br />
available, several investigators derived and<br />
published the theoretical vergence formula<br />
[4–9]. All of these formulas were identical<br />
[10], except for the form in which they were<br />
written and the choice of various constants<br />
such as retinal thickness, optical plane of the<br />
cornea, and optical plane of the IOL. These<br />
slightly different constants accounted for less<br />
than 0.50 diopters in the predicted refraction.<br />
The variation in these constants was a result<br />
of differences in lens styles, A-scan units,<br />
keratometers, and surgical techniques among<br />
the investigators.<br />
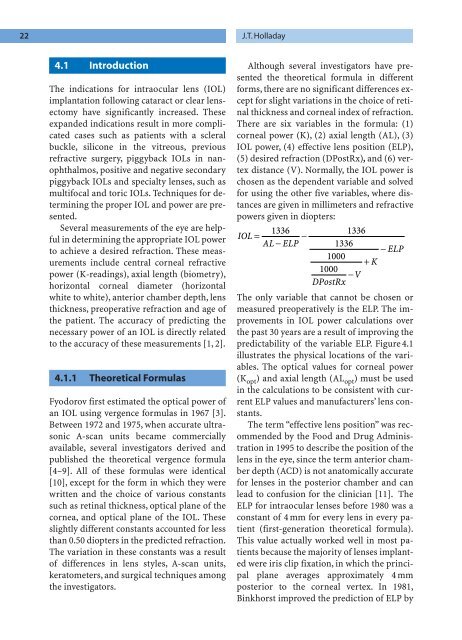
Although several investigators have presented<br />
the theoretical formula in different<br />
forms, there are no significant differences except<br />
for slight variations in the choice of retinal<br />
thickness and corneal index of refraction.<br />
There are six variables in the formula: (1)<br />
corneal power (K), (2) axial length (AL), (3)<br />
IOL power, (4) effective lens position (ELP),<br />
(5) desired refraction (DPostRx), and (6) vertex<br />
distance (V). Normally, the IOL power is<br />
chosen as the dependent variable and solved<br />
for using the other five variables, where distances<br />
are given in millimeters and refractive<br />
powers given in diopters:<br />
IOL<br />
AL ELP<br />
DPostRx V<br />
1336 1336<br />
= −<br />
−<br />
1336<br />
− ELP<br />
1000<br />
+ K<br />
1000<br />
−<br />
The only variable that cannot be chosen or<br />
measured preoperatively is the ELP. The improvements<br />
in IOL power calculations over<br />
the past 30 years are a result of improving the<br />
predictability of the variable ELP. Figure 4.1<br />
illustrates the physical locations of the variables.<br />
The optical values for corneal power<br />
(K opt ) and axial length (AL opt ) must be used<br />
in the calculations to be consistent with current<br />
ELP values and manufacturers’ lens constants.<br />
The term “effective lens position” was recommended<br />
by the Food and Drug Administration<br />
in 1995 to describe the position of the<br />
lens in the eye, since the term anterior chamber<br />
depth (ACD) is not anatomically accurate<br />
for lenses in the posterior chamber and can<br />
lead to confusion for the clinician [11]. The<br />
ELP for intraocular lenses before 1980 was a<br />
constant of 4 mm for every lens in every patient<br />
(first-generation theoretical formula).<br />
This value actually worked well in most patients<br />
because the majority of lenses implanted<br />
were iris clip fixation, in which the principal<br />
plane averages approximately 4 mm<br />
posterior to the corneal vertex. In 1981,<br />
Binkhorst improved the prediction of ELP by