20 - World Journal of Gastroenterology
20 - World Journal of Gastroenterology
20 - World Journal of Gastroenterology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
A B<br />
C<br />
Vespasiani Gentilucci U et al . Non-cirrhotic portal hypertension: A diagnostic challenge<br />
trabeculae were compressed and atrophic. The interface<br />
between nodules was not defined by fibrous septa. There<br />
was only minimal inflammation and no evidence <strong>of</strong> degenerative<br />
changes <strong>of</strong> hepatocytes. Histologically, the diagnosis<br />
was NRH. Clinically, the diagnosis was NCPH, in the form<br />
<strong>of</strong> NRH associated with large regenerative nodules.<br />
As NCPH has been described in association with blood<br />
coagulation disorders, myeloproliferative diseases, immunological<br />
alterations, systemic or intra-abdominal infections<br />
and exposure to toxic substances or to drugs, all these<br />
WJG|www.wjgnet.com<br />
D<br />
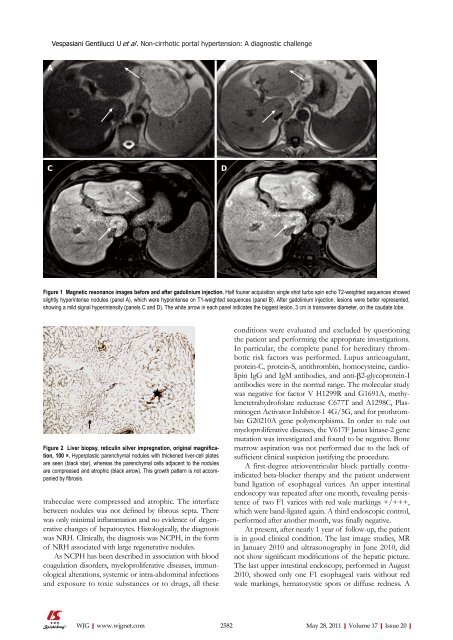
Figure 1 Magnetic resonance images before and after gadolinium injection. Half fourier acquisition single shot turbo spin echo T2-weighted sequences showed<br />
slightly hyperintense nodules (panel A), which were hypointense on T1-weighted sequences (panel B). After gadolinium injection, lesions were better represented,<br />
showing a mild signal hyperintensity (panels C and D). The white arrow in each panel indicates the biggest lesion, 3 cm in transverse diameter, on the caudate lobe.<br />
Figure 2 Liver biopsy, reticulin silver impregnation, original magnification,<br />
100 ×. Hyperplastic parenchymal nodules with thickened liver-cell plates<br />
are seen (black star), whereas the parenchymal cells adjacent to the nodules<br />
are compressed and atrophic (black arrow). This growth pattern is not accompanied<br />
by fibrosis.<br />
conditions were evaluated and excluded by questioning<br />
the patient and performing the appropriate investigations.<br />
In particular, the complete panel for hereditary thrombotic<br />
risk factors was performed. Lupus anticoagulant,<br />
protein-C, protein-S, antithrombin, homocysteine, cardiolipin<br />
IgG and IgM antibodies, and anti-β2-glycoprotein-I<br />
antibodies were in the normal range. The molecular study<br />
was negative for factor V H1299R and G1691A, methylenetetrahydr<strong>of</strong>olate<br />
reductase C677T and A1298C, Plasminogen<br />
Activator Inhibitor-1 4G/5G, and for prothrombin<br />
G<strong>20</strong>210A gene polymorphisms. In order to rule out<br />
myeloproliferative diseases, the V617F Janus kinase-2 gene<br />
mutation was investigated and found to be negative. Bone<br />
marrow aspiration was not performed due to the lack <strong>of</strong><br />
sufficient clinical suspicion justifying the procedure.<br />
A first-degree atrioventricular block partially contraindicated<br />
beta-blocker therapy and the patient underwent<br />
band ligation <strong>of</strong> esophageal varices. An upper intestinal<br />
endoscopy was repeated after one month, revealing persistence<br />
<strong>of</strong> two F1 varices with red wale markings +/+++,<br />
which were band-ligated again. A third endoscopic control,<br />
performed after another month, was finally negative.<br />
At present, after nearly 1 year <strong>of</strong> follow-up, the patient<br />
is in good clinical condition. The last image studies, MR<br />
in January <strong>20</strong>10 and ultrasonography in June <strong>20</strong>10, did<br />
not show significant modifications <strong>of</strong> the hepatic picture.<br />
The last upper intestinal endoscopy, performed in August<br />
<strong>20</strong>10, showed only one F1 esophageal varix without red<br />
wale markings, hematocystic spots or diffuse redness. A<br />
2582 May 28, <strong>20</strong>11|Volume 17|Issue <strong>20</strong>|