Download the entire issue - American Association for Clinical ...
Download the entire issue - American Association for Clinical ...
Download the entire issue - American Association for Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
What are <strong>the</strong> three most important<br />
elements of safe process design?<br />
The first is accounting <strong>for</strong> human factors.<br />
It is important to recognize that processes<br />
which rely on perfect human per<strong>for</strong>mance<br />
are incapable of high reliability. The second<br />
is standardization with limited discretionary<br />
variability (See “Examples,” below).<br />
Fur<strong>the</strong>rmore, reasons <strong>for</strong> appropriate variation<br />
should be captured and fed into <strong>the</strong><br />
process design. The third is organizational<br />
culture. It is essential to have a positive reporting<br />
culture that exposes misses and<br />
near misses, because no process or procedure<br />
is failure-proof. Successful reporting<br />
cultures also identify key vulnerabilities.<br />
How do attitudes about safety in <strong>the</strong><br />
laboratory affect process design?<br />
All processes that rely on vigilance and hard<br />
work are incapable of per<strong>for</strong>ming at a high<br />
level of reliability. If leadership and/or <strong>the</strong><br />
front line worker do not understand <strong>the</strong><br />
limitations of human per<strong>for</strong>mance, <strong>the</strong>n<br />
high levels of reliability will not be possible.<br />
Also, a positive reporting culture is essential.<br />
Punishment <strong>for</strong> human error will impede<br />
process improvement and make <strong>the</strong><br />
organization less safe and less reliable.<br />
14 CliniCal laboratory news July 2011<br />
PATIENT SAFETY FOCUS<br />
TAkING AIM AT REDuCING LAB ERRORS<br />
Designing Processes <strong>for</strong> Patient Safety<br />
The Key is Finding <strong>the</strong> Vulnerabilities and Fixing Them<br />
richard gitomer, Md, Mba, is chief quality<br />
officer <strong>for</strong> emory university Hospital<br />
Midtown and is a general internist by<br />
training. He has led numerous improvement<br />
projects related to access, efficiency,<br />
and innovation in <strong>the</strong> ambulatory setting<br />
and care of patients with chronic conditions.<br />
dr. gitomer is a recognized leader<br />
in process improvement through his collaborations<br />
with <strong>the</strong> institute <strong>for</strong> Healthcare<br />
improvement and <strong>the</strong> association of<br />
american Medical Colleges.<br />
this inteRview was ConDuCteD By CoRinne Fantz, phD.<br />
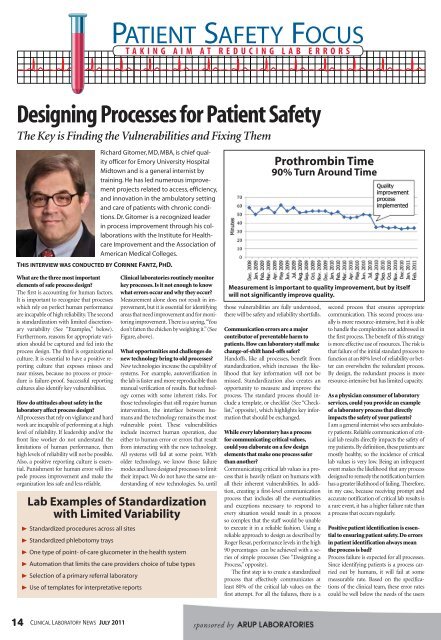
<strong>Clinical</strong> laboratories routinely monitor<br />
key processes. Is it not enough to know<br />
what errors occur and why <strong>the</strong>y occur?<br />
Measurement alone does not result in improvement,<br />
but it is essential <strong>for</strong> identifying<br />
areas that need improvement and <strong>for</strong> monitoring<br />
improvement. There is a saying, “You<br />
don’t fatten <strong>the</strong> chicken by weighing it.” (See<br />
Figure, above).<br />
What opportunities and challenges do<br />
new technology bring to old processes?<br />
New technologies increase <strong>the</strong> capability of<br />
systems. For example, autoverification in<br />
<strong>the</strong> lab is faster and more reproducible than<br />
manual verification of results. But technology<br />
comes with some inherent risks. For<br />
those technologies that still require human<br />
intervention, <strong>the</strong> interface between humans<br />
and <strong>the</strong> technology remains <strong>the</strong> most<br />
vulnerable point. These vulnerabilities<br />
include incorrect human operation, due<br />
ei<strong>the</strong>r to human error or errors that result<br />
from interacting with <strong>the</strong> new technology.<br />
All systems will fail at some point. With<br />
older technology, we know those failure<br />
modes and have designed processes to limit<br />
<strong>the</strong>ir impact. We do not have <strong>the</strong> same understanding<br />
of new technologies. So, until<br />
lab examples of standardization<br />
with limited variability<br />
® standardized procedures across all sites<br />
® standardized phlebotomy trays<br />
® one type of point- of-care glucometer in <strong>the</strong> health system<br />
® automation that limits <strong>the</strong> care providers choice of tube types<br />
® selection of a primary referral laboratory<br />
® use of templates <strong>for</strong> interpretative reports<br />
Prothrombin Time<br />
90% Turn around Time<br />
measurement is important to quality improvement, but by itself<br />
will not significantly improve quality.<br />
those vulnerabilities are fully understood,<br />
<strong>the</strong>re will be safety and reliability shortfalls.<br />
Communication errors are a major<br />
contributor of preventable harm to<br />
patients. How can laboratory staff make<br />
change-of-shift hand-offs safer?<br />
Handoffs, like all processes, benefit from<br />
standardization, which increases <strong>the</strong> likelihood<br />
that key in<strong>for</strong>mation will not be<br />
missed. Standardization also creates an<br />
opportunity to measure and improve <strong>the</strong><br />
process. The standard process should include<br />
a template, or checklist (See “Checklist,”<br />
opposite), which highlights key in<strong>for</strong>mation<br />
that should be exchanged.<br />
While every laboratory has a process<br />
<strong>for</strong> communicating critical values,<br />
could you elaborate on a few design<br />
elements that make one process safer<br />
than ano<strong>the</strong>r?<br />
Communicating critical lab values is a process<br />
that is heavily reliant on humans with<br />
all <strong>the</strong>ir inherent vulnerabilities. In addition,<br />
creating a first-level communication<br />
process that includes all <strong>the</strong> eventualities<br />
and exceptions necessary to respond to<br />
every situation would result in a process<br />
so complex that <strong>the</strong> staff would be unable<br />
to execute it in a reliable fashion. Using a<br />
reliable approach to design as described by<br />
Roger Resar, per<strong>for</strong>mance levels in <strong>the</strong> high<br />
90 percentages can be achieved with a series<br />
of simple processes (See “Designing a<br />
Process,” opposite).<br />
The first step is to create a standardized<br />
process that effectively communicates at<br />
least 80% of <strong>the</strong> critical lab values on <strong>the</strong><br />
first attempt. For all <strong>the</strong> failures, <strong>the</strong>re is a<br />
second process that ensures appropriate<br />
communication. This second process usually<br />
is more resource-intensive, but it is able<br />
to handle <strong>the</strong> complexities not addressed in<br />
<strong>the</strong> first process. The benefit of this strategy<br />
is more effective use of resources. The risk is<br />
that failure of <strong>the</strong> initial standard process to<br />
function at an 80% level of reliability or better<br />
can overwhelm <strong>the</strong> redundant process.<br />
By design, <strong>the</strong> redundant process is more<br />
resource-intensive but has limited capacity.<br />
As a physician consumer of laboratory<br />
services, could you provide an example<br />
of a laboratory process that directly<br />
impacts <strong>the</strong> safety of your patients?<br />
I am a general internist who sees ambulatory<br />
patients. Reliable communication of critical<br />
lab results directly impacts <strong>the</strong> safety of<br />
my patients. By definition, <strong>the</strong>se patients are<br />
mostly healthy, so <strong>the</strong> incidence of critical<br />
lab values is very low. Being an infrequent<br />
event makes <strong>the</strong> likelihood that any process<br />
designed to remedy <strong>the</strong> notification barriers<br />
has a greater likelihood of failing. There<strong>for</strong>e,<br />
in my case, because receiving prompt and<br />
accurate notification of critical lab results is<br />
a rare event, it has a higher failure rate than<br />
a process that occurs regularly.<br />
Positive patient identification is essential<br />
to ensuring patient safety. Do errors<br />
in patient identification always mean<br />
<strong>the</strong> process is bad?<br />
Process failure is expected <strong>for</strong> all processes.<br />
Since identifying patients is a process carried<br />
out by humans, it will fail at some<br />
measurable rate. Based on <strong>the</strong> specifications<br />
of <strong>the</strong> clinical team, <strong>the</strong>se error rates<br />
could be well below <strong>the</strong> needs of <strong>the</strong> users