Dezembro de 2009 - Vol 16 numero 3 - Sociedade Portuguesa de ...
Dezembro de 2009 - Vol 16 numero 3 - Sociedade Portuguesa de ...
Dezembro de 2009 - Vol 16 numero 3 - Sociedade Portuguesa de ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Rev Port Med Int <strong>2009</strong>; <strong>Vol</strong> <strong>16</strong>(3)<br />
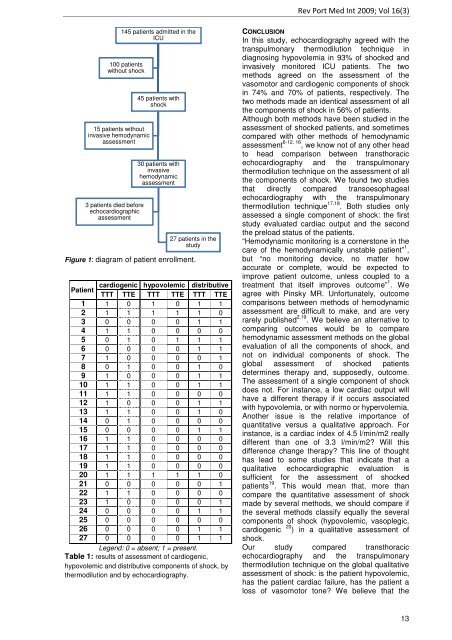
145 patients admitted in the<br />
ICU<br />
100 patients<br />
without shock<br />
15 patients without<br />
invasive hemodynamic<br />
assessment<br />
3 patients died before<br />
echocardiographic<br />
assessment<br />
45 patients with<br />
shock<br />
30 patients with<br />
invasive<br />
hemodynamic<br />
assessment<br />
27 patients in the<br />
study<br />
Figure 1: diagram of patient enrollment.<br />
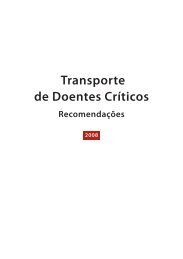
cardiogenic hypovolemic distributive<br />
Patient<br />
TTT TTE TTT TTE TTT TTE<br />
1 1 0 1 0 1 1<br />
2 1 1 1 1 1 0<br />
3 0 0 0 0 1 1<br />
4 1 1 0 0 0 0<br />
5 0 1 0 1 1 1<br />
6 0 0 0 0 1 1<br />
7 1 0 0 0 0 1<br />
8 0 1 0 0 1 0<br />
9 1 0 0 0 1 1<br />
10 1 1 0 0 1 1<br />
11 1 1 0 0 0 0<br />
12 1 0 0 0 1 1<br />
13 1 1 0 0 1 0<br />
14 0 1 0 0 0 0<br />
15 0 0 0 0 1 1<br />
<strong>16</strong> 1 1 0 0 0 0<br />
17 1 1 0 0 0 0<br />
18 1 1 0 0 0 0<br />
19 1 1 0 0 0 0<br />
20 1 1 1 1 1 0<br />
21 0 0 0 0 0 1<br />
22 1 1 0 0 0 0<br />
23 1 0 0 0 0 1<br />
24 0 0 0 0 1 1<br />
25 0 0 0 0 0 0<br />
26 0 0 0 0 1 1<br />
27 0 0 0 0 1 1<br />
Legend: 0 = absent; 1 = present.<br />
Table 1: results of assessment of cardiogenic,<br />
hypovolemic and distributive components of shock, by<br />
thermodilution and by echocardiography.<br />
CONCLUSION<br />
In this study, echocardiography agreed with the<br />
transpulmonary thermodilution technique in<br />
diagnosing hypovolemia in 93% of shocked and<br />
invasively monitored ICU patients. The two<br />
methods agreed on the assessment of the<br />
vasomotor and cardiogenic components of shock<br />
in 74% and 70% of patients, respectively. The<br />
two methods ma<strong>de</strong> an i<strong>de</strong>ntical assessment of all<br />
the components of shock in 56% of patients.<br />
Although both methods have been studied in the<br />
assessment of shocked patients, and sometimes<br />
compared with other methods of hemodynamic<br />
assessment 6-12, <strong>16</strong> , we know not of any other head<br />
to head comparison between transthoracic<br />
echocardiography and the transpulmonary<br />
thermodilution technique on the assessment of all<br />
the components of shock. We found two studies<br />
that directly compared transoesophageal<br />
echocardiography with the transpulmonary<br />
thermodilution technique 17,18 . Both studies only<br />
assessed a single component of shock: the first<br />
study evaluated cardiac output and the second<br />
the preload status of the patients.<br />
“Hemodynamic monitoring is a cornerstone in the<br />
care of the hemodynamically unstable patient” 1 ,<br />
but “no monitoring <strong>de</strong>vice, no matter how<br />
accurate or complete, would be expected to<br />
improve patient outcome, unless coupled to a<br />
treatment that itself improves outcome” 1 . We<br />
agree with Pinsky MR. Unfortunately, outcome<br />
comparisons between methods of hemodynamic<br />
assessment are difficult to make, and are very<br />
rarely published 2,19 . We believe an alternative to<br />
comparing outcomes would be to compare<br />
hemodynamic assessment methods on the global<br />
evaluation of all the components of shock, and<br />
not on individual components of shock. The<br />
global assessment of shocked patients<br />
<strong>de</strong>termines therapy and, supposedly, outcome.<br />
The assessment of a single component of shock<br />
does not. For instance, a low cardiac output will<br />
have a different therapy if it occurs associated<br />
with hypovolemia, or with normo or hypervolemia.<br />
Another issue is the relative importance of<br />
quantitative versus a qualitative approach. For<br />
instance, is a cardiac in<strong>de</strong>x of 4.5 l/min/m2 really<br />
different than one of 3.3 l/min/m2? Will this<br />
difference change therapy? This line of thought<br />
has lead to some studies that indicate that a<br />
qualitative echocardiographic evaluation is<br />
sufficient for the assessment of shocked<br />
patients 19 . This would mean that, more than<br />
compare the quantitative assessment of shock<br />
ma<strong>de</strong> by several methods, we should compare if<br />
the several methods classify equally the several<br />
components of shock (hypovolemic, vasoplegic,<br />
cardiogenic 20 ) in a qualitative assessment of<br />
shock.<br />
Our study compared transthoracic<br />
echocardiography and the transpulmonary<br />
thermodilution technique on the global qualitative<br />
assessment of shock: is the patient hypovolemic,<br />
has the patient cardiac failure, has the patient a<br />
loss of vasomotor tone? We believe that the<br />
13