annual report 2011 - Office for Research - Northwestern University
annual report 2011 - Office for Research - Northwestern University
annual report 2011 - Office for Research - Northwestern University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Bernard Black<br />
School of Law and Kellogg School of Management<br />
Does Hospital Infection Reporting Affect<br />
Actual Infection Rates?<br />
Health-care associated infections (HAIs), often acquired in<br />
hospitals, kill about 100,000 people <strong>annual</strong>ly. Many of these<br />
infections are preventable. In response to the epidemic of<br />
HAIs, many states have adopted laws requiring hospitals<br />
to publicly <strong>report</strong> their infection rates. But whether public<br />
<strong>report</strong>ing affects hospital behavior, and thus affects actual<br />
infection rates, and by how much, is unknown.<br />
Bernard Black, law instruction and finance, and coauthors<br />
Hyun Kim and Myungho Paik of the <strong>University</strong> of Texas at<br />
Austin have studied the first state (Pennsylvania) to require<br />
detailed public <strong>report</strong>ing and one important type of highly<br />
serious and often fatal infection, central-line-associated<br />
bloodstream infections (known as CLABSI). Using a strong<br />
difference-in-differences research design, they find that<br />
a measure of CLABSI rates, based on hospital billing<br />
records, drops by 23 percent in Pennsylvania relative to<br />
states without public <strong>report</strong>ing. The drop in CLABSI rates<br />
is concentrated in hospitals with high <strong>report</strong>ed rates. This<br />
suggests that public <strong>report</strong>ing in fact changes the behavior<br />
of hospitals with high infection rates.<br />
They also compare their non<strong>report</strong>ed measure with the<br />
CLABSI rates that hospitals publicly <strong>report</strong>. The publicly<br />
<strong>report</strong>ed rates drop far faster, by 40 percent over 2005–07;<br />
more than twice the 17 percent drop in inpatient rates<br />
during this period. This suggests that hospitals are “gaming”<br />
the publicly <strong>report</strong>ed rates. That is, some of the decline<br />
in <strong>report</strong>ed rates appears to be real, but some appears to<br />
reflect hospitals changing how they <strong>report</strong> infections.<br />
30 Annual Report <strong>2011</strong> | Excellence in <strong>Research</strong><br />
Black and his coauthors recently received a $450,000 grant<br />
from the Robert Wood Johnson Foundation to extend this<br />
Courtesy of B. Black<br />
research to other states and other types of HAIs.<br />
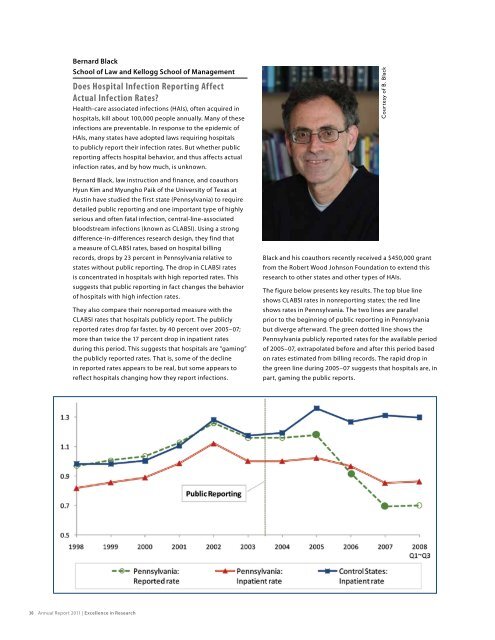
The figure below presents key results. The top blue line<br />
shows CLABSI rates in non<strong>report</strong>ing states; the red line<br />
shows rates in Pennsylvania. The two lines are parallel<br />
prior to the beginning of public <strong>report</strong>ing in Pennsylvania<br />
but diverge afterward. The green dotted line shows the<br />
Pennsylvania publicly <strong>report</strong>ed rates <strong>for</strong> the available period<br />
of 2005–07, extrapolated be<strong>for</strong>e and after this period based<br />
on rates estimated from billing records. The rapid drop in<br />
the green line during 2005–07 suggests that hospitals are, in<br />
part, gaming the public <strong>report</strong>s.