Empowering Nurses for the Future - nursingALD.com
Empowering Nurses for the Future - nursingALD.com
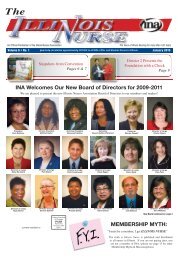
Empowering Nurses for the Future - nursingALD.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
An Official Publication of <strong>the</strong> Illinois <strong>Nurses</strong> Association The Voice of Illinois Nursing <strong>for</strong> more than 100 Years<br />
Volume 5 • No. 4 October 2009<br />
2009 INA Bylaws Proposed<br />
Pages 7, 10<br />
INA Convention<br />
October 14-17, 2009<br />
Yorktown Hilton<br />
Lombard Illinois<br />
<strong>Empowering</strong> <strong>Nurses</strong> <strong>for</strong> <strong>the</strong> <strong>Future</strong><br />
Please join us <strong>for</strong> <strong>the</strong> Illinois <strong>Nurses</strong>’ 80th Biennial<br />
Convention <strong>Empowering</strong> <strong>Nurses</strong> <strong>for</strong> <strong>the</strong> <strong>Future</strong>. Held<br />
at <strong>the</strong> Yorktown Hilton in Lombard Illinois, INA’s 2009<br />
convention is a must attend event <strong>for</strong> anyone interested in<br />
nursing and <strong>the</strong> healthcare industry.<br />
With more than 27 CE course options, this year’s<br />
convention, <strong>Empowering</strong> <strong>Nurses</strong> <strong>for</strong> <strong>the</strong> <strong>Future</strong>, is<br />
designed to embrace and empower nurses in fields across<br />
<strong>the</strong> spectrum of nursing.<br />
Through its educational programs, <strong>the</strong> INA offers<br />
opportunities <strong>for</strong> more than 6,000 members and o<strong>the</strong>r<br />
healthcare professionals to develop expertise, <strong>for</strong>m<br />
professional relationships and exercise leadership, while<br />
contributing to <strong>the</strong> future of nursing.<br />
This two-day convention is jam-packed with activities<br />
including exhibits, receptions and <strong>the</strong> INA Awards<br />
Banquet. Conference attendees will help chart <strong>the</strong> future<br />
of <strong>the</strong> organization while networking with peers and<br />
gaining insight into <strong>the</strong> nursing profession. Take advantage<br />
of this exciting opportunity to interact with hundreds of<br />
professional nurses!<br />
Please visit INA’s website to view <strong>the</strong> current sessions<br />
offered at <strong>the</strong> convention. Exact descriptions should<br />
be listed on <strong>the</strong> website by Sept. 15. Also, look <strong>for</strong> <strong>the</strong><br />
unveiling of <strong>the</strong> new cover of INA’s Chart publication!<br />
Don’t <strong>for</strong>get that one lucky registrant will win a new HP<br />
Mini Netbook<br />
INA Convention Pull-Out<br />
Pages 7-10<br />
current resident or<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
Continuing Education<br />
Lateral Violence and Bullying in <strong>the</strong> Workplace<br />
Pages 11-13<br />
Registration Fees Member Non-Member Retiree Student<br />
One Day Registration<br />
(attendance at continuing<br />
education sessions only)<br />
$125.00 $150.00 $125.00<br />
Full Registration<br />
(includes award banquet)<br />
$250.00 $275.00 $175.00<br />
Late Registration $300.00 $350.00 $225.00<br />
Individual Awards<br />
Banquet Tickets<br />
(included in full registration)<br />
$50.00 $50.00 $50.00<br />
PAC Fundraising Event<br />
(price is separate from full Registration)<br />
$100.00 $100.00 $100.00<br />
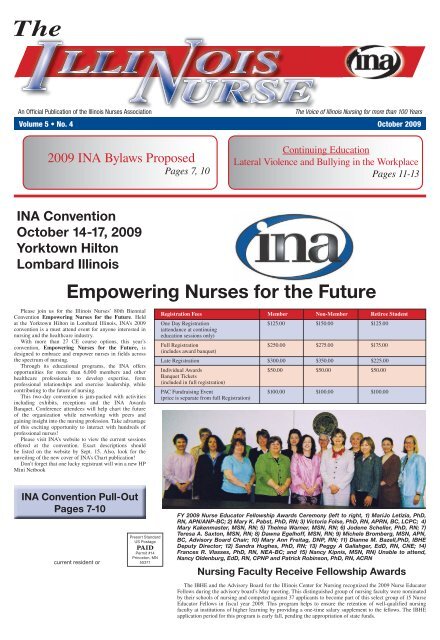
FY 2009 Nurse Educator Fellowship Awards Ceremony (left to right, 1) MariJo Letizia, PhD,<br />
RN, APN/ANP-BC; 2) Mary K. Pabst, PhD, RN; 3) Victoria Folse, PhD, RN, APRN, BC, LCPC; 4)<br />
Mary Kakenmaster, MSN, RN; 5) Thelma Warner, MSN, RN; 6) Jodene Scheller, PhD, RN; 7)<br />
Teresa A. Saxton, MSN, RN; 8) Dawna Egelhoff, MSN, RN; 9) Michele Bromberg, MSN, APN,<br />
BC, Advisory Board Chair; 10) Mary Ann Freitag, DNP, RN; 11) Dianne M. Bazell,PhD, IBHE<br />
Deputy Director; 12) Sandra Hughes, PhD, RN; 13) Peggy A Gallahger, EdD, RN, CNE; 14)<br />
Frances R. Vlasses, PhD, RN, NEA-BC; and 15) Nancy Kipnis, MSN, RN) Unable to attend,<br />
Nancy Oldenburg, EdD, RN, CPNP and Patrick Robinson, PhD, RN, ACRN<br />
Nursing Faculty Receive Fellowship Awards<br />
The IBHE and <strong>the</strong> Advisory Board <strong>for</strong> <strong>the</strong> Illinois Center <strong>for</strong> Nursing recognized <strong>the</strong> 2009 Nurse Educator<br />
Fellows during <strong>the</strong> advisory board’s May meeting. This distinguished group of nursing faculty were nominated<br />
by <strong>the</strong>ir schools of nursing and <strong>com</strong>peted against 37 applicants to be<strong>com</strong>e part of this select group of 15 Nurse<br />
Educator Fellows in fiscal year 2009. This program helps to ensure <strong>the</strong> retention of well-qualified nursing<br />
faculty at institutions of higher learning by providing a one-time salary supplement to <strong>the</strong> fellows. The IBHE<br />
application period <strong>for</strong> this program is early fall, pending <strong>the</strong> appropriation of state funds.
Page 2 October 2009 The Illinois Nurse<br />
President’s Message<br />
Pam Robbins BSN, RN<br />
President Illinois <strong>Nurses</strong> Association<br />
The acknowledgement that<br />
quality patient care is linked<br />
to <strong>the</strong> educated skilled nursing<br />
professional is finally reaching<br />
<strong>the</strong> ears of <strong>the</strong> healthcare industry<br />
and <strong>the</strong> public. The federal<br />
government’s move to identify<br />
preventable <strong>com</strong>plications<br />
occurring in hospitals and<br />
restricting Medicare payment<br />
<strong>for</strong> such “preventable hospital<br />
acquired conditions” was<br />
initiated last year. The HHS.<br />
gov web page of Centers Pam Robbins<br />
<strong>for</strong> Medicare and Medicaid<br />
Services (CMS) has a fact sheet,<br />
“Medicare Takes New Steps to Help Make Your Hospital<br />
Stay Safer” that outlines reasonably preventable conditions.<br />
The federal government cited several selected conditions <strong>the</strong>y<br />
believe are “reasonably preventable” by following evidencedbased<br />
guidelines. Conditions identified as costly or <strong>com</strong>mon<br />
hospital acquired conditions range from retained <strong>for</strong>eign<br />
objects post-surgical procedures to severe pressure ulcers.<br />
Documentation of conditions not present on admission will<br />
be on a “no pay list” <strong>for</strong> reimbursement. Finally, <strong>the</strong>y are<br />
listening to what nurses have been saying <strong>for</strong> years. Payment<br />
of continued identifiable poor out<strong>com</strong>es costs more to <strong>the</strong><br />
federal government system and it is unacceptable! Reasonable<br />
oversight to reducing such hospital acquired conditions seen<br />
as avoidable was based on evidence based research. In this<br />
equation, qualified skilled professional nursing care begets<br />
better patient out<strong>com</strong>es and leads to <strong>the</strong> reduction of mortality<br />
and morbidity rates, evidence any nurse already knows! So<br />
how does <strong>the</strong> nurse find a foothold validating quality nursing<br />
care in <strong>the</strong>ir individual work place?<br />
Let’s return to <strong>the</strong> backbone of nursing education,<br />
Evidenced-Based (E-B) research. “Nursing research<br />
provides a specialized base of scientific knowledge that<br />
helps <strong>the</strong> nursing profession to anticipate and successfully<br />
meet <strong>the</strong> constantly changing challenges of healthcare<br />
provision and gives us leverage to maintain and justify our<br />
importance and relevance in current and future societies”<br />
(Nellett, 2009, p. 1). Nursing standards of any specialty<br />
rely on sound nursing research when determining what<br />
<strong>the</strong> standards of practice should be. Nursing professionals<br />
whe<strong>the</strong>r at <strong>the</strong> bedside, supervisory or master’s prepared<br />
nursing researcher, are all consumers of nursing research<br />
and all can assist in improving patient out<strong>com</strong>es if<br />
<strong>com</strong>mon goals are embraced. Simply said, “a consumer of<br />
nursing research is one who reads, reviews and critiques<br />
nursing research findings and who attempts to use and<br />
apply <strong>the</strong> findings in practice. … Nursing research links<br />
<strong>the</strong>ory, practice and education” (Nellett, 2009, p. 2). How<br />
does <strong>the</strong> bedside professional nurse responsible <strong>for</strong> direct<br />
care ac<strong>com</strong>plish such? Here are some key guides <strong>for</strong> safe<br />
care and activation of E-B research.<br />
<strong>Nurses</strong> must know <strong>the</strong> regulatory law and rules<br />
(policies) of <strong>the</strong>ir institution. You must be knowledgeable<br />
in your own specialty practice as to what are <strong>the</strong><br />
standards of care in that particular specialty. If you are<br />
practicing outside of any of <strong>the</strong>se, you must address<br />
<strong>the</strong>m immediately! Document your care clearly in <strong>the</strong><br />
medical record. If gaps are seen in nursing care, report<br />
<strong>the</strong>m, investigate and discover, through E-B research,<br />
improvements to delivery safer care. It is paramount that<br />
buy-in happens from <strong>the</strong> bedside nurses to administration<br />
when embracing a <strong>com</strong>mitment to improved healthcare<br />
delivery. Sound nursing research and existing specialty<br />
nursing standards can improve changes in delivery of care.<br />
Better healthcare delivery systems decrease patient injury<br />
and it is up to nursing to define what is best <strong>for</strong> patients<br />
and <strong>the</strong> profession.<br />
Nursing research is <strong>the</strong> road to improving care.<br />
The idea that work environments are driven by cost<br />
containment only validates <strong>the</strong> need to push <strong>for</strong> nurses to<br />
advocate <strong>for</strong> nursing care that is based on sound nursing<br />
research. E-Based Practice is gaining momentum even<br />
though it has been around since <strong>the</strong> day of Florence<br />
Nightingale, whose concepts are congruent with <strong>the</strong><br />
present priorities of nursing research…promotion of health,<br />
prevention of disease. (Lo-Biondo-Wood & Haber, 2006).<br />
All nurses are consumers of nursing research. To<br />
modify your work environment, use evidenced based<br />
data! This is a great start to defining staffing requirements<br />
<strong>for</strong> specific patient populations. The care of <strong>the</strong> patients<br />
is directly related to <strong>the</strong>ir aggregate needs AND <strong>the</strong><br />
educational background and skills of <strong>the</strong> registered nurses<br />
caring <strong>for</strong> <strong>the</strong>m. The bedside nurse can search databases to<br />
find research to update <strong>the</strong>ir nursing practices and improve<br />
patient out<strong>com</strong>es. Access is available though hospital<br />
libraries, and educational institutions. Every hospital<br />
with a healthcare curriculum most certainly has database<br />
access. You want nursing research articles that may be<br />
downloaded in full-text and include such databases as<br />
CINAHL Plus, Cochrane Collection, Cochrane Database of<br />
Systematic Reviews, and Database of Abstracts of Reviews<br />
of Effectiveness (DARE). Also useful are <strong>the</strong> following<br />
databases, but <strong>the</strong>re may not be full text, articles: Medline<br />
(First Search) and Medline Plus. Identify improvements<br />
and share with administration and colleagues. Your E-B<br />
research is <strong>the</strong> bedrock of your presentation!<br />
How does an Illinois nurse <strong>the</strong>n activate what he/<br />
President’s Message continued on page 3<br />
Il l I n o I s nu r s e s As s o c I A t I o n<br />
President<br />
Pamela Robbins, BSN, RN: pamrobbins@urban<strong>com</strong>.net<br />
First Vice President<br />
Mildred Taylor, BSN, RN: m.taylor.rn@<strong>com</strong>cast.net<br />
Second Vice President<br />
Roosevelt Gallion, M.Ed, BSN, RN: RG2194@aol.<strong>com</strong><br />
Secretary<br />
Lori Anderson, CRNA, RN: react911@aol.<strong>com</strong><br />
Treasurer<br />
Sharon Zandell, RN: sharon.zandel@med.va.gov<br />
Board of Directors:<br />
Rebecca O. Armea, RN: rarmearn@sbcglobal.net<br />
Sandra Fischer, RN: fish23w@yahoo.<strong>com</strong><br />
Queen Gallien-Patterson, RN: qpatterson@aol.<strong>com</strong><br />
P. Joan Larsen, RN: pjscrapbook@frontiernet.net<br />
Terri L. Williams RN: sewpro9370@aol.<strong>com</strong><br />
Joyce Bailey RN: jabrn_51@webtv.net<br />
Barbara M. Gaffke, PhD, MSN, CS: gaffke5@ameritech.net<br />
Mary Bortolotti, RN: mandkbort@aol.<strong>com</strong><br />
Karen Kelly, EdD, RN, CNE-BC: kkellys@aol.<strong>com</strong><br />
Pamela J. Para RN, MPH, CPHRM, ARM, FASHRM:<br />
pjpara2001@yahoo.<strong>com</strong><br />
Ruby P. Reese RN PhD<br />
Susan Draine: susan.draine@<strong>com</strong>cast.net<br />
District Presidents<br />
1 Roosevelt Gallion: RG2194@aol.<strong>com</strong><br />
2 Mary Bortolotti: mandkbort@aol.<strong>com</strong><br />
3 Sharon Peterson: speterson@crusaderclinic.org<br />
5 Royanne Shultz: royanneschultz@hotmail.<strong>com</strong><br />
8 Ann O’Sullivan: aosullivan@blessinghospital.<strong>com</strong><br />
9 Terri Williams: sewpro9370@aol.<strong>com</strong><br />
10 Jane Bruker: jkbru@aol.<strong>com</strong><br />
13 Janet Lynch: lynch.janet08@gmail.<strong>com</strong><br />
14 Martha McDonald: Martha.mcdonald@sih.net<br />
15 Vacant<br />
17 Ann Smith: nevann@<strong>com</strong>cast.net<br />
18 Vacant<br />
19 Margaret Kraft: margaret.kraft@att.net<br />
20 Cheryl Anema: tccnurse@aol.<strong>com</strong><br />
21 Sandra Webb Booker: ste<strong>the</strong>s@yahoo.<strong>com</strong><br />
E & GW Commission<br />
Sandra D. Robinson, Chair: nursemoney06@yahoo.<strong>com</strong><br />
Linda Briggs: lindasbriggs@yahoo.<strong>com</strong><br />
LaGretta Green: ltg1106@aol.<strong>com</strong><br />
Rosemary Kelly: ranajarkelly@yahoo.<strong>com</strong><br />
Virginia Rockett: momynator@yahoo.<strong>com</strong><br />
Judith K. Hopkins: Sicu40@aol.<strong>com</strong><br />
Thomas Magana: ndirish01@sbcglobal.net<br />
Christine H. Szkarlat: Christine.Szkarlat@va.gov<br />
Joseph Williams: Sangamojoe@aol.<strong>com</strong><br />
Local Unit Chairpersons/Co-Chairs<br />
City of Chicago: Timothy Hudson<br />
RC-23 State of Illinois: Lee Goehl<br />
Co-Chair Bill Schubert<br />
St. Joseph: Marlene Murphy and Chris Daly<br />
Union Health Services: Sophie Heldak<br />
University of Chicago: Karen Keller and Tom Magana<br />
University of Illinois: Marcia Hymon (D20), Leo Sherman<br />
VA Hines: Gail Robinson<br />
Christine Szkarlat (D9)<br />
VA North Chicago: Thelma Fuentes<br />
VA Westside: Murrie Davis (D01)
The Illinois Nurse October 2009 Page 3<br />
Il l I n o I s nu r s e s As s o c I A t I o n<br />
Illinois <strong>Nurses</strong> Association/<br />
Illinois <strong>Nurses</strong> Foundation<br />
105 W. Adams, Suite 2101 911 S. Second Street<br />
Chicago, IL 60603 Springfield, IL 62704<br />
312/419-2900 217/523-0783<br />
Fax: 312/419-2920 Fax: 217/523-0838<br />
www.illinoisnurses.<strong>com</strong><br />
Executive Director:<br />
Susan Swart, MS, RN: Ext. 229, sswart@illinoisnurses.<strong>com</strong><br />
Chief Financial Officer:<br />
Rick Roche: Ext. 230, rroche@illinoisnurses.<strong>com</strong><br />
Program Director, EGW:<br />
Elwood R. Thompson: Ext. 228, ethompson@illinoisnurses.<strong>com</strong><br />
Deputy Executive Director:<br />
Sharon Canariato, MSN, MBA, RN, Ext. 235<br />
scanariato@illinoisnurses.<strong>com</strong><br />
Director of Marketing and Member Services:<br />
Joseland Nixon, MS: Ext. 232 jnixon@illinoisnurses.<strong>com</strong><br />
Associate Director, Continuing Education:<br />
Kemi Ani, Ext. 240 kani@illinoisnurses.<strong>com</strong><br />
E&GW Staff Attorney:<br />
Alice Johnson, Ext. 239, ajohnson@illinoisnurses.<strong>com</strong><br />
E&GW Staff Specialists:<br />
Rick Lezu, 217-523-0783 rlezu@illinoisnurses.<strong>com</strong><br />
Remzi Jaos, Ext. 245 rjaos@illinoisnurses.<strong>com</strong><br />
Pam Brunton, Ext. 224 pbrunton@illinoisnurses.<strong>com</strong><br />
Abass Wane, Ext. 249 awane@illinoisnurses.<strong>com</strong><br />
E&GW Coordinator:<br />
Rhonda Perkins, Ext. 223 rperkins@illinoisnurses.<strong>com</strong><br />
Coordinator, Springfield<br />
Staci Moore, 217-523-0783 staci@illinoisnurses.<strong>com</strong><br />
Staff Accountant:<br />
Toni Fox, Ext. 243 tfox@illinoisnurses.<strong>com</strong><br />
Administrative Assistant:<br />
Brenda Richardson, Ext. 248 brichardson@illinoisnurses.<strong>com</strong><br />
Melinda Sweeney, Ext. 222 msweeney@illinoisnurses.<strong>com</strong><br />
Editorial Committee<br />
Theresa Adelman, RN<br />
Alma Labunski, EdD, MS, RN, Chair<br />
Margaret Kraft, RN, PhD<br />
Linda Olson, PhD, RN<br />
Lisa Anderson Shaw DPH, MA, MSN<br />
Mary Shoemaker, PhD, BS, MS, RN<br />
The Illinois Nurse is published quarterly (4 issues yearly) by <strong>the</strong><br />
Illinois <strong>Nurses</strong> Association, 105 W. Adams, Suite 2101, Chicago,<br />
IL 60603.<br />
Advertising Rates Contact—Arthur L. Davis Publishing Agency,<br />
Inc., 517 Washington St., P.O. Box 216, Cedar Falls, Iowa 50613,<br />
(800) 626-4081, sales@aldpub.<strong>com</strong>. INA and <strong>the</strong> Arthur L.<br />
Davis Publishing Agency, Inc. reserve <strong>the</strong> right to reject any<br />
advertisement. Responsibility <strong>for</strong> errors in advertising is limited to<br />
corrections in <strong>the</strong> next issue or refund of price of advertisement.<br />
Acceptance of advertising does not imply endorsement or approval<br />
by <strong>the</strong> Illinois <strong>Nurses</strong> Association of products advertised, <strong>the</strong><br />
advertisers, or <strong>the</strong> claims made. Rejection of an advertisement<br />
does not imply a product offered <strong>for</strong> advertising is without merit,<br />
or that <strong>the</strong> manufacturer lacks integrity, or that this association<br />
disapproves of <strong>the</strong> product or its use. INA and <strong>the</strong> Arthur L. Davis<br />
Publishing Agency shall not be held liable <strong>for</strong> any consequences<br />
resulting from purchase or use of an advertiser’s product. Articles<br />
appearing in this publication express <strong>the</strong> opinions of <strong>the</strong> authors;<br />
<strong>the</strong>y do not necessarily reflect views of <strong>the</strong> staff, board, or<br />
membership of INA or those of <strong>the</strong> national or local associations.<br />
President’s Message continued from page 2 professional nursing services are delivered. Building safer<br />
she needs to do in <strong>the</strong> work environment? Using nursing<br />
research is simple. After you have found <strong>the</strong> research that<br />
helps you validate your concerns, working with a Clinical<br />
Nurse Specialists whose expertise is educating nursing<br />
staff will be key to implementing any hospital’s quality<br />
improvement plan. Institutions should have qualified<br />
Masters and Doctorate prepared nurses to assist in <strong>the</strong><br />
needs of improving healthcare delivery systems to produce<br />
better patient out<strong>com</strong>es, and education <strong>for</strong> bedside nurses<br />
to engage in improving nursing care <strong>for</strong> <strong>the</strong>ir patient<br />
populations. All nurses are consumers of nursing<br />
research. <strong>Nurses</strong>, who are organized in nursing unions,<br />
have Nursing Care <strong>com</strong>mittees <strong>for</strong> improving practice/<br />
working conditions. Yes, work conditions <strong>for</strong> nurses are<br />
inseparable from nursing practice issues! Share <strong>the</strong> gaps of<br />
your current work situation and develop a plan to improve.<br />
Use E-B data as a resource when working with <strong>the</strong> Nursing<br />
Committee to determine staffing plans. The <strong>for</strong>mation of<br />
this type of <strong>com</strong>mittee is mandated at every hospital by<br />
<strong>the</strong> Illinois law Nurse Staffing by Patient Acuity (PA 95-<br />
0401).<br />
INA has educational CE’s to assist professional<br />
nurses in learning how to be<strong>com</strong>e a consumer of nursing<br />
research and building your nursing advocacy skills.<br />
Join your professional nursing association, <strong>the</strong> Illinois<br />
<strong>Nurses</strong> Association, to advance your advocacy skills and<br />
advance your nursing practice. Safe care emanates from<br />
adequate nurse staffing based on patient aggregate needs<br />
and <strong>the</strong> skills and abilities of <strong>the</strong> registered nurse, when<br />
healthcare delivery systems is <strong>the</strong> re<strong>com</strong>mendation of <strong>the</strong><br />
Institute of Medicine’s federal study. All levels of nursing<br />
are to be engaged using Nursing Research as road map to<br />
improve patient care. I truly believe it is time to activate<br />
<strong>the</strong> process and have nursing define <strong>the</strong> improvements<br />
needed in today’s healthcare system. Nursing research has<br />
<strong>com</strong>municated <strong>for</strong> decades that <strong>the</strong> value of quality nursing<br />
care is priceless.<br />
www.cms.hhs.gov/apps/media/fact_sheets.asp August<br />
4, 2008 “Medicare Takes New Steps to Help Make Your<br />
Hospital Stay Safer”<br />
Lo-Biondo-Wood & Haber. (2006). Nursing Research<br />
Methods and Critical Appraisal <strong>for</strong> Evidence-Based<br />
Practice. St. Louis: Mosby Elsevier.<br />
Nellett, G. H. (2009). Lecture 1 Notes from Nursing<br />
Research, Summer 2009,<br />
Staffing by Patient Acuity—Public Act (PA) 95-0401<br />
www.ilgov The Illinois General Assembly Homepage
Page 4 October 2009 The Illinois Nurse<br />
INA Convention Benefits Anyone involved in <strong>the</strong> Nursing Industry<br />
Participation at <strong>the</strong> INA Convention gives you more<br />
one-on-one exposure to more healthcare professionals you<br />
could ever hope to meet in <strong>the</strong> nursing industry during<br />
one event. You also get <strong>the</strong> chance to learn <strong>the</strong> latest in<br />
healthcare technology, well be<strong>for</strong>e it hits <strong>the</strong> market. By<br />
exhibiting at <strong>the</strong> INA Convention, you’ll get a chance to<br />
meet <strong>the</strong> top leaders in <strong>the</strong> nursing industry. INA supports<br />
your exhibit investment in a variety of ways:<br />
• Innovative programming will draw more than 500<br />
INA attendees.<br />
• More than 80% exclusive exhibit hours are scheduled<br />
to give you maximum visibility and exposure to this<br />
target market.<br />
• A grand opening reception, sponsored by INA, will<br />
showcase your products and services during kick off<br />
of <strong>the</strong> convention in <strong>the</strong> exhibit hall.<br />
• Each exhibitor will receive a list of all attendees<br />
<strong>for</strong> follow-up and future sale and promotional<br />
opportunities<br />
To request an Exhibitor Prospectus and take advantage<br />
of this opportunity to reach your target market effectively<br />
and efficiently, contact Joseland Nixon at 312-419-2900,<br />
x232.<br />
Exhibitor In<strong>for</strong>mation<br />
Exhibit Fees<br />
Premium Exhibit space . . . . . . . . . . . . . . . . . . . . $1,000<br />
Includes premium location in exhibit hall and ½ page<br />
ad in both program booklets<br />
Standard Exhibit space . . . . . . . . . . . . . . . . . . . . . . $750<br />
Includes standard 8x10 exhibit space and ¼ page ad in<br />
both program booklets<br />
Budget Exhibit space . . . . . . . . . . . . . . . . . . . . . . . . $500<br />
Includes standard 8x10 exhibit space<br />
Set-Up<br />
Thursday, October 15th after 1 p.m.<br />
Exhibit Schedule<br />
Thursday, October 15th<br />
4:45 p.m. – 6:15 p.m. Reception in Exhibit Hall<br />
Friday, October 16th<br />
Continuing Education scheduled throughout <strong>the</strong> day.<br />
Friday’s Exhibitor events include: Breakfast at 7:30 a.m.<br />
(Exhibitors only); Exhibit Hall Open at 8 a.m. - Breakfast<br />
<strong>for</strong> attendees in exhibit area; Lunch in exhibit hall at 11:30<br />
a.m. (Exhibitors only); Exhibit Hall Open <strong>for</strong> Lunch at<br />
noon.<br />
Breakfast and lunch <strong>for</strong> two exhibitors per booth is<br />
included in your exhibit cost. Additional meals can be<br />
purchased in advance of <strong>the</strong> event <strong>for</strong> a nominal charge.<br />
Tear Down<br />
Friday, October 16th<br />
4:00 p.m. – Exhibit Hall will close at 4:30 p.m.<br />
How Well Is Your Workplace Staffed?<br />
by: Sharon V. Canariato, MSN, MBA, RN<br />
Insufficient nurse staffing<br />
is among <strong>the</strong> top concerns <strong>for</strong><br />
nurses today. Recent studies<br />
have demonstrated what most<br />
nurses already know: nursing<br />
care and patient safety are<br />
absolutely linked. Research<br />
has shown that improved<br />
RN staffing has a beneficial<br />
effect on patient out<strong>com</strong>es and<br />
mortality. <strong>Nurses</strong>, <strong>the</strong>re<strong>for</strong>e,<br />
play a critical role in patient<br />
safety and quality of care. Safe<br />
nurse staffing is at <strong>the</strong> top of<br />
<strong>the</strong> Illinois <strong>Nurses</strong> Association<br />
agenda.<br />
Sharon Canariato<br />
An American <strong>Nurses</strong> Association poll of registered<br />
nurses nationwide reveals <strong>the</strong>ir significant concerns<br />
over how nurse staffing affects <strong>the</strong> quality of care, and<br />
contributes to <strong>the</strong> growing nursing shortage. The results<br />
highlight <strong>the</strong> need <strong>for</strong> adequate nurse staffing critical to<br />
<strong>the</strong> delivery of quality patient care.<br />
The ANA poll of 14,933 nurses was <strong>com</strong>pleted on <strong>the</strong><br />
website safestaffingsaveslives.org from March 31, 2008 to<br />
June 5, 2009. These were <strong>the</strong> findings:<br />
• What is your role?<br />
Staff <strong>Nurses</strong> = 74%<br />
O<strong>the</strong>r = 18%<br />
Nurse Managers 8%<br />
• How often do you engage in non-nursing roles?<br />
Examples: Delivering meal trays, transfer<br />
patients, draw labs, go to pharmacy<br />
Always (Every Day) = 65.7%<br />
Frequently (Once a Week) = 18.2%<br />
Sometimes (Once a Month) = 5.8%<br />
No Response = 4.1%<br />
Rarely (Less than Monthly) = 4.0%<br />
Never = 2.2%<br />
• How often are you able to take your full meal<br />
break?<br />
Sometimes (Once a Month) = 24.7%<br />
Rarely (Less than Monthly) = 24.1%<br />
Frequently (Once a Week) = 23.1%<br />
Always (Every Day) = 12.4%<br />
Never = 11.7%<br />
No Response = 4.0%<br />
• Would You Feel Confident Having Someone close<br />
to you Receive Care in <strong>the</strong> Facility in Which You<br />
Work?<br />
No = 49.5%<br />
Yes = 45.9%<br />
No Response = 2.3%<br />
• Do You Believe <strong>the</strong> Staffing on Your Unit and<br />
Shift is Sufficient?<br />
No = 71.9%<br />
Yes = 23.5%<br />
No Response = 4.6%<br />
• Are You Currently Considering Leaving Your<br />
Position?<br />
Yes = 52.7%<br />
No = 45.0%<br />
No Response = 2.3%<br />
• If You Are Considering Leaving Your Current<br />
Position, Is <strong>the</strong> Reason Associated with<br />
Inadequate Staffing?<br />
Yes = 42.2%<br />
Not Applicable = 30.6%<br />
No Response = 15.9%<br />
No = 11.3%<br />
INA believes that providing nurses with <strong>the</strong> authority<br />
to establish nurse staffing plans, as evidenced by Illinois’<br />
new Nurse Staffing by Acuity law, ensures that patients’<br />
needs would be met and <strong>the</strong> working environment of that<br />
nurse would be improved. Some factors to be considered<br />
in developing a safe staffing plan includes <strong>the</strong> acuity level<br />
of <strong>the</strong> patients, staff experience and skill mix, <strong>the</strong> need <strong>for</strong><br />
nurses to have adequate opportunity and time to exercise<br />
professional judgment with respect to patient care and<br />
an acknowledgement that patient needs can change from<br />
moment to moment.<br />
If you would be interested in attending a working<br />
seminar to develop a staffing plan <strong>for</strong> your hospital and/<br />
or unit, please contact Illinois <strong>Nurses</strong> Association at 312-<br />
419-2900.
The Illinois Nurse October 2009 Page 5<br />
APN Journey to Remove Barriers to Practice<br />
by Bridget A. Cahill, APN/CNP<br />
Chairperson, ISAPN Government Relations<br />
Committee<br />
The Illinois Society of Advanced Practice Nursing<br />
(ISAPN), Illinois <strong>Nurses</strong> Association (INA) and <strong>the</strong><br />
Illinois Association <strong>for</strong> Nurse Anes<strong>the</strong>tists (IANA) are<br />
working toge<strong>the</strong>r to advance legislation that will remove<br />
<strong>the</strong> restrictive language regarding <strong>the</strong> mandated written<br />
collaborative agreement with a physician. It will likely be<br />
a long journey, but as nurses and advanced practice nurses,<br />
we are used to challenges.<br />
A recap of 2009 events surrounding our journey: SB<br />
1600 was introduced to remove all references to <strong>the</strong> written<br />
collaborative agreement (WCA) in all statutes. As a united<br />
front ISAPN, INA, and IANA co-hosted a legislative<br />
reception to educate legislators on our issue. The bill was<br />
released from <strong>the</strong> Senate Committee on Assignments and<br />
a hearing was held. All APN specialties were represented<br />
and presented <strong>com</strong>pelling testimony. The bill did not pass,<br />
but we made great strides in our first curve of our journey.<br />
One thing we learned is that not all nurses understand<br />
<strong>the</strong> WCA, its implications, and how it can be a method to<br />
‘control’ <strong>the</strong> scope of practice of APNs.<br />
The specific language regarding <strong>the</strong> WCA can be<br />
found in Section 65-35 of <strong>the</strong> Nurse Practice Act. (Log<br />
onto www.idfpr.<strong>com</strong>, click Department of Professional<br />
Regulation, and select ‘nursing.’ That will take you directly<br />
to <strong>the</strong> Nurse Practice Act and <strong>the</strong> language in question.<br />
What is a written collaborative agreement? Does it<br />
protect or hinder APN practice?<br />
A Written Collaborative Agreement:<br />
• Is an agreement, that must be signed by both <strong>the</strong><br />
APN and physician describing <strong>the</strong> APN scope of<br />
practice and articulating specifics to <strong>the</strong> working<br />
relationship. It is NOT a work contract! Nor does it<br />
provide such security.<br />
• It is not liability protection. The APN is accountable<br />
<strong>for</strong> his/her own judgment and decisions.<br />
• Guidelines must be developed between <strong>the</strong> APN and<br />
physician, and followed by <strong>the</strong> APN and physician.<br />
• The APN and physician MUST meet in person once<br />
a month. (CRNA readers, check <strong>the</strong> specific Act<br />
language <strong>for</strong> your requirements.)<br />
• If an APN wishes to collaborate with more than one<br />
physician, that is permissive as long as <strong>the</strong> APN<br />
provides a copy of all agreements to a physician,<br />
should he/she request <strong>the</strong> written collaborative<br />
agreement.<br />
Eliminating <strong>the</strong> written collaborative agreement does<br />
not and will not remove <strong>the</strong> requirement to collaborate<br />
with our physician colleagues and any o<strong>the</strong>r member of<br />
<strong>the</strong> healthcare team. APNs know and respect <strong>the</strong> work<br />
of our colleagues and recognize physician specialists are<br />
needed to provide <strong>the</strong> best care possible to our patients.<br />
And APNs know <strong>the</strong> limits of <strong>the</strong>ir scope of practice based<br />
on <strong>the</strong>ir individual education and experience. We know<br />
when to ask <strong>for</strong> collaboration and consultation. A WCA, as<br />
currently required, is simply not needed <strong>for</strong> collaboration<br />
and cooperation to exist. Recall that prior to <strong>the</strong> statutory<br />
licensure, APNs did practice, and practiced safely, without<br />
a WCA! The challenge is in front of us. We know it will<br />
be a tough, multi-year process. And, we know we need <strong>the</strong><br />
understanding and support of every nurse in <strong>the</strong> state.<br />
Educate ourselves first and <strong>the</strong>n <strong>the</strong> legislators will<br />
enable us to take <strong>the</strong> next step! We need your help!!<br />
Please volunteer to be<strong>com</strong>e grassroots activist. Contact me<br />
(bacgovrel@<strong>com</strong>cast.net) if you desire to get involved and I<br />
will connect you with <strong>the</strong> GR Chairs of each organization<br />
working toge<strong>the</strong>r to make this a reality. Nursing has a<br />
long and powerful history of affecting change in Illinois<br />
healthcare when we stand toge<strong>the</strong>r and make our voices<br />
heard. I invite you to join us.
Page 6 October 2009 The Illinois Nurse<br />
Illinois <strong>Nurses</strong> Foundation<br />
Foundation Seeks to Aid<br />
<strong>Nurses</strong> in Need<br />
The Illinois <strong>Nurses</strong> Foundation understands times are hard, but <strong>the</strong>y are even harder<br />
<strong>for</strong> those less <strong>for</strong>tunate. In this tough economic environment, we have seen many people<br />
suffering without food, clothing or shelter. Among those in need are nurses. The Illinois<br />
<strong>Nurses</strong> Foundation has created a Caring Garden to grow a special fund to provide this<br />
much needed assistance. Through your ef<strong>for</strong>ts to grow this fund, you will be tending to<br />
<strong>the</strong> future hopes of <strong>the</strong>se nurses.<br />
<strong>Nurses</strong> who are facing financial hardship due to illness, natural disaster, personal or<br />
family crisis often have no place to turn. INF wants to give <strong>the</strong>m hope, one more way to<br />
fur<strong>the</strong>r our mission to support <strong>the</strong> nurses of Illinois. The donation <strong>for</strong>m located here is<br />
also on our website at www.illinoisnurses.<strong>com</strong>. Please support <strong>the</strong>se nurses today. This<br />
special fund is <strong>the</strong> only one of its kind in Illinois; help us give <strong>the</strong> nurses in crisis a ray of<br />
hope. Donate today!<br />
Name:<br />
Address:<br />
City, State Zip:<br />
Donation amount:<br />
Check Check Number:<br />
Credit Card<br />
Visa MasterCard<br />
Card Number :<br />
Expiration Date:<br />
Name on Card:<br />
Verification Code (On back of card):<br />
Mail donations to:<br />
Illinois <strong>Nurses</strong> Foundation- <strong>Nurses</strong> in Need<br />
105 W. Adams St.,<br />
Suite 2101<br />
Chicago, IL 60603
The Illinois Nurse October 2009 Page 7<br />
2009 INA Bylaws Proposed<br />
CURRENT BYLAW<br />
Article V Members<br />
Section 5.02 Membership Privileges<br />
In addition, each member, who is eligible to be organized <strong>for</strong> purposes of<br />
collective bargaining, shall have <strong>the</strong> right to:<br />
(8)exercise freedoms of speech and assembly, as protected by <strong>the</strong> United States<br />
Constitution and federal and state statutes; and to, <strong>for</strong>m, join, and assist any<br />
labor organization which is not in direct <strong>com</strong>petition with <strong>the</strong> INA, o<strong>the</strong>r<br />
constituent member associations (CMAs) and ANA. The exercise of <strong>the</strong>se<br />
rights, in and of <strong>the</strong>mselves does not constitute grounds <strong>for</strong> disciplinary action<br />
by ANA.<br />
PROPOSED BYLAW AMENDMENT<br />
Article V Members<br />
Add new (7) and (8) to Article V Members Section 5.02 (a) Membership<br />
Privileges and renumber current (7) to (9).<br />
(7) INA only members do not receive benefits from ANA at <strong>the</strong> national<br />
level; and,<br />
(8) RNs working or living in Illinois may join at <strong>the</strong> state level only, at<br />
any time and <strong>for</strong> such periods of time that INA state only membership is<br />
sanctioned by a written agreement with <strong>the</strong> ANA;<br />
In addition, each member, who is eligible to be organized <strong>for</strong> purposes of<br />
collective bargaining, shall have <strong>the</strong> right to:<br />
(9) exercise freedoms of speech and assembly, as protected by <strong>the</strong> United<br />
States Constitution and federal and state statutes; and to, <strong>for</strong>m, join, and assist<br />
any labor organization which is not in direct <strong>com</strong>petition with <strong>the</strong> INA, o<strong>the</strong>r<br />
constituent member associations (CMAs) and ANA. The exercise of <strong>the</strong>se<br />
rights, in and of <strong>the</strong>mselves does not constitute grounds <strong>for</strong> disciplinary action<br />
by ANA.<br />
Con<strong>for</strong>mity with ANA Bylaws.<br />
RATIONALE<br />
CURRENT BYLAW<br />
Section 5.04 Transfer - State<br />
Transfer of membership from INA to ano<strong>the</strong>r Constituent Member Association<br />
and from ano<strong>the</strong>r ANA Constituent Member Association to INA shall be in<br />
accordance with ANA bylaws.<br />
PROPOSED BYLAW AMENDMENT<br />
Add new language to Section 5.04 Transfer - State<br />
Transfer of membership from INA to ano<strong>the</strong>r Constituent Member Association<br />
and from ano<strong>the</strong>r ANA Constituent Member Association to INA shall be in<br />
accordance with ANA bylaws, without payment of additional dues. The<br />
transferring constituent is not required to refund to <strong>the</strong> individual<br />
member nor to <strong>the</strong> receiving constituent dues already paid.<br />
Con<strong>for</strong>mity with ANA Bylaws.<br />
Article VII Dues<br />
Section 7.04 Dues to ANA<br />
RATIONALE<br />
CURRENT BYLAW<br />
The INA shall be bound by <strong>the</strong> obligation to pay dues to <strong>the</strong> ANA pursuant to<br />
<strong>the</strong> ANA bylaws and <strong>the</strong> House of Delegates policy and until such time that<br />
INA members vote to disaffiliate from ANA by 2/3 of <strong>the</strong> vote cast by a ballot<br />
distributed to <strong>the</strong> entire INA membership. This vote may occur by mail or<br />
electronic ballot, with appropriate notice and procedures to protect <strong>the</strong> integrity<br />
and validity of <strong>the</strong> vote.<br />
Article VII Dues<br />
Section 7.04 Dues to ANA<br />
PROPOSED BYLAW AMENDMENT<br />
INA shall remit a portion of dues to <strong>the</strong> ANA that is equal to that which<br />
INA remits to ANA <strong>for</strong> direct members in accordance with <strong>the</strong> ANA<br />
dues policy and <strong>the</strong> written agreement between <strong>the</strong> INA and ANA. The<br />
INA shall be bound by <strong>the</strong> obligation to pay dues to <strong>the</strong> ANA pursuant to <strong>the</strong><br />
ANA bylaws and <strong>the</strong> House of Delegates policy and until such time that INA/<br />
ANA members vote to disaffiliate from ANA by 2/3 vote of <strong>the</strong> entire INA/<br />
ANA membership. This vote may occur by mail or electronic ballot, with<br />
appropriate notice and procedures to protect <strong>the</strong> integrity and validity of <strong>the</strong><br />
vote.<br />
Con<strong>for</strong>mity to ANA Bylaws.<br />
RATIONALE<br />
It is noted that INA and ANA have no written agreement.<br />
CURRENT BYLAW<br />
Article XI Officers and Directors<br />
Section 11.02 Directors<br />
There shall be 14 directors, 4 of whom shall be staff nurses. Directors are<br />
elected each biennium in <strong>the</strong> manner provided in Article XXI.<br />
PROPOSED BYLAW AMENDMENT<br />
Article XI Officers and Directors<br />
Section 11.02 Directors<br />
There shall be 10 directors. Directors are elected each biennium in <strong>the</strong> manner<br />
provided in Article XXI.<br />
RATIONALE<br />
This director number change is prudent, from a fiscal standpoint, and because<br />
INA has significantly fewer members than when this number of directors<br />
was chosen. Designating staff nurse seats on <strong>the</strong> INA BOD was done at a<br />
time when <strong>the</strong>re were very few staff nurses serving on <strong>the</strong> INA Board. The<br />
intent was to designate, <strong>for</strong> a temporary period of time, seats <strong>for</strong> staff nurses<br />
to aspire to. For <strong>the</strong> last many elections, a significant portion of <strong>the</strong> INA BOD<br />
are nurses in direct care. The term staff nurse, be<strong>com</strong>ing less used, no longer<br />
strictly defines <strong>the</strong> direct care nurse. With <strong>the</strong> broad range of titles and job<br />
descriptions, clinical designation is almost impossible to gauge.<br />
CURRENT BYLAW<br />
Article XII Board of Directors<br />
Section 12.01 Composition<br />
The Board of Directors shall consist of <strong>the</strong> following:<br />
a) five officers of INA;<br />
b) fourteen directors, four of whom shall be staff nurses<br />
PROPOSED BYLAW AMENDMENT<br />
Article XII Board of Directors<br />
Section 12.01 Composition<br />
The Board of Directors shall consist of <strong>the</strong> following:<br />
a) five officers of INA;<br />
b) ten directors<br />
RATIONALE<br />
This director number change is prudent, from a fiscal standpoint, and because<br />
INA has significantly fewer members than when this number of directors<br />
was chosen. Designating staff nurse seats on <strong>the</strong> INA BOD was done at a<br />
time when <strong>the</strong>re were very few staff nurses serving on <strong>the</strong> INA Board. The<br />
intent was to designate, <strong>for</strong> a temporary period of time, seats <strong>for</strong> staff nurses<br />
to aspire to. For <strong>the</strong> last many elections, a significant portion of <strong>the</strong> INA BOD<br />
are nurses in direct care. The term staff nurse, be<strong>com</strong>ing less used, no longer<br />
strictly defines <strong>the</strong> direct care nurse. With <strong>the</strong> broad range of titles and job<br />
descriptions, clinical designation is almost impossible to gauge.<br />
CURRENT BYLAW<br />
Article XVIII Commissions<br />
Section 18.03 Composition<br />
The Commissions on Continuing Education and Economic and General<br />
Welfare shall consist of nine members. The Commission on Work<strong>for</strong>ce<br />
Advocacy shall consist of five members.<br />
PROPOSED BYLAW AMENDMENT<br />
Article XVIII Commissions<br />
Section 18.03 Composition<br />
The Commissions on Continuing Education, Work<strong>for</strong>ce Advocacy and<br />
Economic and General Welfare shall consist of nine members.<br />
RATIONALE<br />
Consistency of membership across all <strong>com</strong>missions. The Commission on<br />
Work<strong>for</strong>ce Advocacy needs additional members due to <strong>the</strong> current projects.<br />
Section 18.06 Terms<br />
(See Proviso)<br />
Section 18.06 Terms<br />
(See Proviso)<br />
CURRENT BYLAW<br />
PROPOSED BYLAW AMENDMENT<br />
RATIONALE<br />
Note Proviso: As approved at 2008 HOD.<br />
Three (3) Commission on Work<strong>for</strong>ce Advocacy (CWFA) Commissioners shall<br />
be elected <strong>for</strong> <strong>the</strong> 2011-2015 term. Two (2) CWFA Commissioners will remain<br />
in <strong>the</strong>ir positions from 2007-2013. This will ensure future staggered terms.<br />
The CWFA will decide <strong>the</strong> slots by lot or by attrition.<br />
Bylaws Proposed Amendments continued on page 10<br />
2009 INA Convention
Page 8 October 2009 The Illinois Nurse<br />
INA Convention Schedule<br />
Thursday, October 15, 2009 Schedule<br />
4:00pm-7pm Registration<br />
4:45pm-6:15pm<br />
6:15pm-8pm<br />
Exhibitor Wel<strong>com</strong>e Reception<br />
PAC Reception<br />
Thursday, October 15, 2009<br />
Registration: 4:00 pm – 7:00 pm<br />
Exhibitor Wel<strong>com</strong>e Reception: 4:45 pm – 6:15 pm<br />
PAC Event: 6:15 pm – 8:00 pm<br />
2009 INA Convention<br />
Friday, October 16, 2009<br />
7:00am-3pm Registration<br />
7:00am-4pm Exhibit Hall<br />
7:00am-9am Breakfast with Exhibitors<br />
Concurrent Sessions<br />
9:00am-10 am Psycho-Neuro Immunology and Allostasis:<br />
Translating Research into Practice—Rebecca<br />
West, APN/CNP<br />
Interventional Options <strong>for</strong> <strong>the</strong> Treatment of<br />
Emphysema—Theresa Boley, APN/CNP<br />
Demystifying Grassroots Lobbying (repeated<br />
session)<br />
Changes to <strong>the</strong> ANCC Continuing Education<br />
Criteria— Jean Roberson, MS, RN<br />
Lateral Violence and Bullying in <strong>the</strong><br />
Workplace—Ann O’Sullivan, MSN, RN, CAN<br />
Newborn Hearing Screening: Why We Do It<br />
and Why It Matters—Gail Tanner, AuD<br />
9:00am-2pm Onsite voting/INA office<br />
Concurrent Sessions<br />
10:15am-11:15am Reimbursement Issues—<br />
Marie Lindsey, APN/CNP, PhD<br />
A Case-Based Approach to Improving<br />
Out<strong>com</strong>es in HIV/AIDS—<br />
Ann Williams, EdD, ANP<br />
Patient Evaluation after Bariatric Surgery —<br />
Ed Schafer, RN, DNP<br />
Presenting Educational Opportunities <strong>for</strong><br />
Nursing—<br />
Alexia Hieber Johnson, APN/CNS, CCRN<br />
Retaining <strong>Nurses</strong>: What Will It Take? —Patti<br />
Ludwig-Beymer, PhD, RN, CTN<br />
Telemedicine: The <strong>Future</strong> is Now — Pamela<br />
J. Para, RN, MPH<br />
Write is Might: Running from Risk— Linda J.<br />
Hay, JD and<br />
Susan A. Wagener, RN, JD<br />
11:15am-12:30pm General Session-How to Stay Energized in a<br />
Changing World—Greg Risberg, MSA, CSP<br />
12:30pm-2:00pm Lunch with Exhibitors<br />
Concurrent Sessions<br />
2:00pm-3:00pm CXR Basics <strong>for</strong> APNs—<br />
Maria Connolly, APN/CNS, PhD<br />
What Do We Tell <strong>the</strong> Kids? Practical Tips <strong>for</strong><br />
Discussing Death and Dying with Children—<br />
Megan Styx, APN/CNP<br />
NP Malpractice and Remedies—<br />
Ellen Wodika and Nancy Lagorio<br />
Preceptor Model Proposal—<br />
Susan Draine, MSN, RN<br />
Employee Free Choice Act—Al Martin<br />
Leading Change in Creating a Blueprint <strong>for</strong><br />
Cultural Competency, Part I—<br />
Growing <strong>the</strong> Nursing Work<strong>for</strong>ce in Illinois<br />
—Linda B. Roberts, MSN, RN<br />
Concurrent Sessions<br />
3:15pm-4:15pm Suturing Workshop—Ed Schaefer, RN, DNP<br />
Nursing Research: How to Get Started—<br />
Donna Plonczynski, APN/CNP<br />
Enhancing Ethics with Movies—<br />
Laura McAnally, BNS, RN, MA, MJ<br />
Staffing by Acuity Law—<br />
Debra L. Weiderman, BSN, RN<br />
Leading Change in Creating a Blueprint <strong>for</strong><br />
Cultural Competency Part II—<br />
The History of Collective Bargaining at<br />
INA—Linda B. Roberts, MSN, RN<br />
5:00pm-6:00pm Illinois <strong>Nurses</strong> Foundation (INF) Reception<br />
6:30pm-9:30pm Awards Banquet<br />
Saturday, October 17, 2009<br />
7:00am-8:00am Breakfast<br />
7:30am-8:30am Registration/Credentialing<br />
8:30am-12:00pm House of Delegates<br />
12:00pm-1:30pm Lunch on your own<br />
12:00pm-1:30pm New Board Meeting/Lunch<br />
1:30pm-4:00pm House of Delegates<br />
Friday, October 16, 2009<br />
Registration: 7:00 am – 3:00 pm<br />
Breakfast with Exhibitors: 7:00 am – 9:00 am<br />
Onsite Voting 9:00 am – 2:00 pm<br />
CONCURRENT SESSIONS: 9:00 AM – 10:00 AM<br />
• Psycho-Neuro Immunology and Allostasis: Translating Research into<br />
Practice, Rebecca West, APN/CNP<br />
○ Explains <strong>the</strong> conceptual framework of psycho-neuro immunology and<br />
how it relates to allostasis, allostatic load, nursing research and practice.<br />
Discusses key findings from current related research<br />
• Interventional Options <strong>for</strong> <strong>the</strong> Treatment of Emphysema, Theresa Boley,<br />
APN/CNP<br />
○ Discusses types of emphysema, causes and <strong>the</strong>rapies. Defines process<br />
<strong>for</strong> patient selection in <strong>com</strong>mon emphysema treatments<br />
• Demystifying Grassroots Lobbying<br />
○ Identifies <strong>com</strong>ponents of grassroots lobbying in order to facilitate change<br />
in <strong>the</strong> workplace and legislature. Discusses strategies to implement a<br />
successful grassroots program<br />
• Changes to <strong>the</strong> ANCC Continuing Education Criteria, Jean Roberson, MS, RN<br />
○ This program will explain current guidelines <strong>for</strong> creating a nursing<br />
CE program, and how <strong>the</strong>se guidelines will be affected by up<strong>com</strong>ing<br />
changes to <strong>the</strong> ANCC criteria<br />
• Lateral Violence and Bullying in <strong>the</strong> Workplace, Ann O’Sullivan, MSN, RN, CAN<br />
○ Don’t be bullied in <strong>the</strong> workplace! This program highlights <strong>the</strong> signs and<br />
characteristics of nurse workplace abuse and harassment. See how you can<br />
protect yourself and improve <strong>the</strong> workplace to protect o<strong>the</strong>r nurses.<br />
• Newborn Hearing Screening: Why We Do It and Why It Matters, Gail<br />
Tanner, AuD<br />
○ Newborn hearing screening in Illinois became mandatory in 2002.<br />
While screenings are per<strong>for</strong>med in all nurseries in Illinois birthing<br />
hospitals, nurses per<strong>for</strong>ming <strong>the</strong> screenings rarely understand <strong>the</strong><br />
electro-physiological methodology <strong>the</strong>y employ. The goal is to develop<br />
an understanding of <strong>the</strong> “bigger picture” of newborn hearing screening<br />
CONCURRENT SESSIONS: 10:15 AM – 11:15 AM<br />
• Reimbursement Issues, Marie Lindsey, APN/CNP, PhD<br />
○ Reimbursement concepts are critical to APN practice. Underlying issues<br />
related to Medicaid, Medicare and private insurance will be discussed.<br />
• A Case-Based Approach to Improving Out<strong>com</strong>es in HIV/AIDS, Ann<br />
Williams, EdD, ANP<br />
○ Be able to identify patients at risk <strong>for</strong> HIV and utilizing routine<br />
testing. Initiating HAART through a case-based approach. Implement<br />
strategies <strong>for</strong> <strong>the</strong> management of side effects, overall management and<br />
unique diagnostic challenges<br />
• Patient Evaluation after Bariatric Surgery, Ed Schaefer, RN, DNP<br />
○ Discusses anatomical changes that occur from different bariatric<br />
surgical procedures. Reviews typical and atypical presentation of<br />
abdominal <strong>com</strong>plaints associated with bariatric surgery. Discusses<br />
workup and disposition of pathology<br />
• Presenting Educational Opportunities <strong>for</strong> Nursing, Alexia Hieber Johnson,<br />
APN/CNS, CCRN<br />
○ This program describes <strong>the</strong> process of developing CNE <strong>for</strong> <strong>the</strong><br />
beginning educator, staff nurses and advanced practice nurses. This<br />
program will empower nurses to share knowledge through CNE<br />
programs at <strong>the</strong> unit level and beyond. The program starts with<br />
concepts of adult learning <strong>the</strong>ory.<br />
• Retaining <strong>Nurses</strong>: What Will it Take? Patti Ludwig-Beymer, PhD, RN, CTN<br />
○ This course will look at <strong>the</strong> self perceptions of knowledge and expertise<br />
in older and younger nurses. Factors that influence willingness to<br />
remain in <strong>the</strong> work<strong>for</strong>ce will be addressed. Discussion will also center<br />
on modifications to support older nurse retention.<br />
• Telemedicine: The <strong>Future</strong> is Now, Pamela J. Para, RN, MPH<br />
○ This presentation will illustrate what nurses should know about<br />
telemedicine from historical, legislative and patient safety perspectives.<br />
The presentation will explore nurses’ involvement in this emerging<br />
field, as well as broader concepts related to telemedicine as a strategy/<br />
tool <strong>for</strong> health care re<strong>for</strong>m.<br />
• Write is Might: Running From Risk, Linda J. Hay, JD and Susan A. Wagener,<br />
RN, JD<br />
○ The goal of this presentation is to provide nurses with a brief overview<br />
of <strong>the</strong> legal process, to better understand what is required by <strong>the</strong> law to<br />
prove and defend a nursing malpractice case. This seminar will provide<br />
some basic risk management concepts that apply to nurses, including<br />
<strong>the</strong> need <strong>for</strong> good documentation, <strong>the</strong> critical importance of <strong>the</strong> medical<br />
record, and what <strong>the</strong> <strong>com</strong>plete medical record entails. The seminar<br />
will discuss <strong>the</strong> use of electronic medical records in this context<br />
including emails, laptop <strong>com</strong>puters and related technologies in <strong>the</strong> risk<br />
management context. Finally, <strong>the</strong> seminar will address some <strong>com</strong>mon<br />
bases <strong>for</strong> nursing liability such as <strong>com</strong>munication with o<strong>the</strong>r health<br />
care providers, admission and discharge issues, chain of <strong>com</strong>mand, and<br />
policies and procedures<br />
KEYNOTE SESSION: 11:15 AM – 12:30 PM<br />
• How to Stay Energized in a Changing World, Greg Risberg, MSA, CSP<br />
○ Discusses elements of genuine <strong>com</strong>munication and obstacles in its<br />
achievement. Demonstrates ways of <strong>com</strong>municating which are more honest,<br />
yet appropriate, to <strong>the</strong> situation. Assists you in recognizing stress indicators<br />
and applying methods of stress reduction in your own life
The Illinois Nurse October 2009 Page 9<br />
of Events Join Us <strong>for</strong> <strong>the</strong>se Special Events<br />
Thursday, October 15<br />
4:45pm-6:15pm Exhibitor Reception<br />
Lunch with Exhibitors: 12:30 pm – 2:00 pm<br />
Kick off INA’s 80th Biennial Convention with this<br />
annual wel<strong>com</strong>ing event. Join us in thanking this year’s<br />
CONCURRENT SESSIONS: 2:00 PM – 3:00 PM<br />
exhibitors <strong>for</strong> <strong>the</strong>ir support of INA and <strong>the</strong> nursing<br />
profession during <strong>the</strong> past year as you network with old<br />
friends and establish new contacts.<br />
• CXR Basics <strong>for</strong> APNs, Maria Connolly, APN/CNS, PhD<br />
○ Reviews basic radiographic lung densities. Describes an approach to<br />
ensure thorough interpretation and characteristics found in <strong>the</strong> primary<br />
and acute care settings<br />
• What Do We Tell <strong>the</strong> Kids? Practical Tips <strong>for</strong> Discussing Death and Dying<br />
with Children, Megan Styx, APN/CNP<br />
○ Describes <strong>the</strong> central elements in a child’s concept of death and <strong>the</strong> normal<br />
grief responses. Identifies age-appropriate strategies to explain death to a<br />
child with <strong>com</strong>passion and to support a child through grief and bereavement.<br />
Identifies warning signs of ineffective coping in a grieving child<br />
• NP Malpractice and Remedies, Ellen Wodika and Nancy Lagorio<br />
○ Increases awareness of professional liability risks to APNs in <strong>the</strong>ir<br />
practice. Utilizes data that APNs can use to benchmark <strong>the</strong>ir own<br />
out<strong>com</strong>es. Provides re<strong>com</strong>mendations to support APNs in managing<br />
<strong>the</strong>ir own professional liability risks<br />
• Preceptor Model Proposal, Susan Draine, MSN, RN<br />
○ This proposal addresses <strong>the</strong> current nursing shortage on all levels, by<br />
discussing a new preceptor proposal. In this model, students enrolled in<br />
traditional BS RN clinical courses would be assigned to a unit to work<br />
with an RN who is a preceptor and be supervised by an agency based<br />
MSN faculty member. In exchange <strong>for</strong> acting as preceptor, <strong>the</strong> RN would<br />
receive credit hours of free tuition towards his/her BSN or MSN<br />
• Employee Free Choice Act, Al Martin<br />
○ Learn about <strong>the</strong> Employee Free Choice Act (EFCA). This act, which is<br />
pending in Congress, can greatly expand a group’s ability to organize and<br />
unionize. It would amend <strong>the</strong> NLRA to establish an easier system during<br />
organizing ef<strong>for</strong>ts, and <strong>for</strong> o<strong>the</strong>r purposes<br />
• Leading Change in Creating a Blueprint <strong>for</strong> Cultural Competency, Part I<br />
○ Be<strong>com</strong>e a symbol of change in <strong>the</strong> corporate environment, while<br />
integrating cultural <strong>com</strong>petence in practice and education. You will<br />
review principles <strong>for</strong> cultural <strong>com</strong>petence which are based on out<strong>com</strong>es<br />
from developing a blueprint<br />
• Growing <strong>the</strong> Nursing Work<strong>for</strong>ce in Illinois, Linda B. Roberts, MSN, RN<br />
○ Learn <strong>the</strong> history of <strong>the</strong> Illinois Center <strong>for</strong> Nursing as well as <strong>the</strong>ir<br />
successful projects in solving <strong>the</strong> states nursing shortage<br />
CONCURRENT SESSIONS: 3:15 PM – 4:15 PM<br />
• Suturing Workshop, Ed Schaefer, RN, DNP<br />
○ Learn principles of wound cleansing, examination, proper tissue handling<br />
and post care instructions. Discusses equipment needed along with<br />
techniques <strong>for</strong> wound closure and dressing. Various wound closure<br />
techniques discussed.<br />
• Nursing Research: How to Get Started, Donna Plonczynski, APN/CNP<br />
○ Discusses <strong>the</strong> value of nursing research. The process <strong>for</strong> developing a<br />
research question into a study is demonstrated. The procedure in ethical<br />
and responsible manners will be identified<br />
• APN Media Training, Julie Adkins, APN/CNP<br />
○ Discusses <strong>the</strong> type of in<strong>for</strong>mation journalist use <strong>for</strong> television, newspaper<br />
and radio. You will learn how to talk to journalists of all media types as<br />
well as how to interpret body language cues during an interview<br />
• Enhancing Ethics with Movies, Laura, McAnally, BNS, RN, MA, MJ<br />
○ Observing ethical situations in films can give members a better<br />
understanding of how <strong>com</strong>plex patient care is and of <strong>the</strong> ethical issues<br />
that often arise<br />
• Staffing by Acuity Law, Debra L. Weiderman, BSN, RN<br />
○ The Nurse Staffing by Patient Acuity law provides <strong>for</strong> nurses to be<strong>com</strong>e<br />
actively involved in <strong>the</strong>ir practice and have a voice in <strong>the</strong> staffing decisions<br />
made at <strong>the</strong>ir hospital. One of <strong>the</strong> many requirements includes that every<br />
hospital implement a staffing plan re<strong>com</strong>mended by a <strong>com</strong>mittee of nurses,<br />
<strong>com</strong>prised of 50% direct-care staff<br />
• Leading Change in Creating a Blueprint <strong>for</strong> Cultural Competency, Part II,<br />
○ Continued from above description<br />
• The History of Collective Bargaining at INA, Linda B. Roberts, MSN, RN<br />
○ Learn about <strong>the</strong> development of <strong>the</strong> national and state Economic Security and<br />
General Welfare Program. Hear about Illinois initiatives and <strong>the</strong> strengths of<br />
INA’s program<br />
INF Reception: 5:00 pm – 6:00 pm<br />
INF Silent Auction: 5:30 pm – 6:00 pm<br />
Awards Banquet: 6:30 pm – 9:30 pm<br />
Saturday, October 17, 2009<br />
Registration/Credentialing: 7:30 am – 8:30 am<br />
Breakfast: 7:00 am – 8:00 am<br />
House of Delegates: 8:30 am – 12:00 pm<br />
Lunch: 12:00 – 1:30 (on your own)<br />
New Board Meeting with lunch: 12:00 – 1:30<br />
House of Delegates, continued: 1:30 – 4:00<br />
6:15pm-8:00pm INA PAC Reception<br />
Want to have fun while you help <strong>the</strong> INA Political<br />
Action Committee? Join us <strong>for</strong> night of fun and festivities!<br />
We have a night of networking and fun, including a new wild and wacky<br />
game show hosted by Comedy Capers. This event will pull four members<br />
from <strong>the</strong> audience, place <strong>the</strong>m at podiums equipped with microphones and<br />
have <strong>the</strong>m participate in a real live game show! The PAC Reception will<br />
last from 6:15 pm to 8:00 pm. Tickets are $100*. You can get tickets from<br />
<strong>the</strong> INA staff at <strong>the</strong> registration desk and at <strong>the</strong> door. You can also call<br />
(217) 523-0783 <strong>for</strong> in<strong>for</strong>mation or tickets.<br />
* Any INA member who purchases a ticket will automatically be entered<br />
into a drawing <strong>for</strong> a bed and breakfast trip at <strong>the</strong> Heartland Lodge in<br />
Nebo, Illinois.<br />
Friday, October 16<br />
5:00pm-6:00pm Illinois <strong>Nurses</strong><br />
Foundation Gala Reception<br />
Join us as we recognize past and present donors of <strong>the</strong><br />
Illinois <strong>Nurses</strong> Foundation. The gala will also announce <strong>the</strong> 2009 Anne<br />
Zimmerman Fellowship to one deserving member<br />
who has demonstrated outstanding leadership within INA.<br />
Also, don’t <strong>for</strong>get to stop by <strong>the</strong> silent auction.<br />
6:30pm-9:30pm INA Awards Dinner<br />
Come celebrate ano<strong>the</strong>r great Biennium of<br />
achievement. We will honor and acknowledge those<br />
individuals who have made significant contributions to<br />
INA and/or <strong>the</strong> nursing profession during <strong>the</strong> past<br />
Biennium. Full registrants will receive one ticket with <strong>the</strong><br />
cost of registration fees. Attendees who register only <strong>for</strong><br />
Friday will need to purchase a ticket if <strong>the</strong>y wish to<br />
attend this event. Tickets must be purchased in advance<br />
and will not be sold onsite.<br />
Virtual Forums Schedule<br />
CONVENTION FORUMS TO BE DONE VIA GoToMeeting and<br />
CONFERENCE CALL<br />
Members can choose to participate via <strong>the</strong>ir <strong>com</strong>puter and phone and<br />
view in<strong>for</strong>mation as it is discussed or download <strong>the</strong> in<strong>for</strong>mation from <strong>the</strong><br />
INA website and participate via conference call only. The choice is yours.<br />
To participate via GoToMeeting an email address is necessary so as to<br />
send <strong>the</strong> member <strong>the</strong> appropriate link.<br />
Call in to 866-951-1151 conference room #1340574<br />
Please RSVP to Susan Swart 312-419-2900 x229 or sswart@<br />
illinoisnurses.<strong>com</strong> <strong>for</strong> <strong>the</strong> <strong>for</strong>um and session you will be attending.<br />
DON’T FORGET TO INCLUDE YOUR EMAIL ADDRESS.<br />
Bylaws <strong>for</strong>um Finance <strong>for</strong>um<br />
Sept 22 5:30 pm Oct 1 5:30 pm<br />
Oct 1 10:00 am Oct 5 10:00 am<br />
Oct 5 6:30 pm Oct 7 6:30 pm<br />
Candidate <strong>for</strong>um<br />
Candidates and members are invited to participate in a question and<br />
answer session. Candidate in<strong>for</strong>mation will be located on Votenet<br />
accessible from <strong>the</strong> INA convention page. All candidates should/will be<br />
advised to submit a bio <strong>for</strong> <strong>the</strong> website. This will provide in<strong>for</strong>mation to<br />
members on who <strong>the</strong> candidates are and what <strong>the</strong>ir goals will be.<br />
Voting begins Oct 1st and ends Oct 16th at 2pm<br />
Sept 21 5:00 pm<br />
Sept 23 6:00 pm<br />
Legislative Plat<strong>for</strong>m Strategic Plan Forum<br />
Sept 28 10:00 am Sept 30 6:00 pm<br />
Oct 6 5:30 pm<br />
2009 INA Convention
Page 10 October 2009 The Illinois Nurse<br />
2009 INA Convention<br />
CURRENT BYLAW<br />
18.04 Vacancies<br />
Vacancies on <strong>the</strong> Commission on <strong>the</strong> Continuing Education shall by filled by<br />
<strong>the</strong> Board. Vacancies on <strong>the</strong> Commission on Economic and General Welfare<br />
shall be filled by that <strong>com</strong>mission. Except <strong>for</strong> un<strong>for</strong>eseen circumstances,<br />
failure to attend two consecutive meetings of a <strong>com</strong>mission shall constitute a<br />
resignation, and <strong>the</strong> vacancy shall be filled as provided above.<br />
PROPOSED BYLAW AMENDMENT<br />
18.04 Vacancies<br />
Vacancies on <strong>the</strong> Commission on Continuing Education shall by filled by<br />
<strong>the</strong> Board. Vacancies on <strong>the</strong> Commission on Economic and General Welfare<br />
and Commission on Work<strong>for</strong>ce Advocacy shall be filled by that <strong>com</strong>mission.<br />
Except <strong>for</strong> un<strong>for</strong>eseen circumstances, failure to attend two consecutive<br />
meetings of a <strong>com</strong>mission shall constitute a resignation, and <strong>the</strong> vacancy shall<br />
be filled as provided above.<br />
RATIONALE<br />
Clarification of <strong>the</strong> CWFA’s authority to fill vacancies on that <strong>com</strong>mission.<br />
CURRENT BYLAW<br />
Article XXI Elections<br />
Section 21.01 Election by Secret Ballot<br />
(a) Each biennium, 5 INA officers, 14 directors, 4 members of <strong>the</strong> Congress on<br />
Health Policy and Practice, 2 or 3 members of <strong>the</strong> Commission on Continuing<br />
Education, 4 members of <strong>the</strong> Commission on Economic and General Welfare<br />
and 2 or 3 members of <strong>the</strong> Commission on Work<strong>for</strong>ce Advocacy shall be<br />
elected by <strong>the</strong> membership by secret ballot. Each member shall vote <strong>for</strong> 5<br />
INA officers, 14 directors, 4 members of <strong>the</strong> Congress on Health Policy and<br />
Practice, 2 or 3 members of <strong>the</strong> Commission on Continuing Education, and<br />
4 members of <strong>the</strong> Commission on Economic and General Welfare. Only<br />
non-collective bargaining members, who are also members of <strong>the</strong> Center <strong>for</strong><br />
American Nursing, may vote <strong>for</strong> members of <strong>the</strong> Commission on Work<strong>for</strong>ce<br />
Advocacy. Only INA members who are in collective bargaining may vote <strong>for</strong><br />
members of <strong>the</strong> Commission on Economic and General Welfare.<br />
(b) Delegates and alternate delegates to <strong>the</strong> ANA House of Delegates shall be<br />
elected each biennium by <strong>the</strong> Membership by secret ballot.<br />
PROPOSED BYLAW AMENDMENT<br />
Article XXI Elections<br />
Section 21.01 Election by Secret Ballot<br />
(a) Each biennium, 5 INA officers, 10 directors, 4 members of <strong>the</strong> Congress<br />
on Health Policy and Practice, 4 members of <strong>the</strong> Commission on Continuing<br />
Education, 4 members of <strong>the</strong> Commission on Economic and General Welfare<br />
and 4 members of <strong>the</strong> Commission on Work<strong>for</strong>ce Advocacy shall be elected by<br />
<strong>the</strong> membership by secret ballot. Each member shall vote <strong>for</strong> 5 INA officers,<br />
10 directors, 4 members of <strong>the</strong> Congress on Health Policy and Practice, and 4<br />
members of <strong>the</strong> Commission on Continuing Education. Only non-collective<br />
bargaining members, who are also members of <strong>the</strong> Center <strong>for</strong> American<br />
Nursing, may vote <strong>for</strong> members of <strong>the</strong> Commission on Work<strong>for</strong>ce Advocacy.<br />
Only INA members who are in collective bargaining may vote <strong>for</strong> members of<br />
<strong>the</strong> Commission on Economic and General Welfare.<br />
(b) Delegates and alternate delegates to <strong>the</strong> ANA House of Delegates shall be<br />
elected each biennium by <strong>the</strong> INA/ANA Membership by a separate secret<br />
ballot.<br />
RATIONALE<br />
Consistency of <strong>com</strong>missioner elections across all <strong>com</strong>missions. Clarification<br />
of member voting eligibility <strong>for</strong> <strong>the</strong> Commission on Work<strong>for</strong>ce Advocacy.<br />
Con<strong>for</strong>mity with <strong>the</strong> ANA Bylaws.<br />
Article V Members<br />
Section 5.02 Membership Privileges<br />
CURRENT BYLAW<br />
PROPOSED BYLAW AMENDMENT<br />
Add new language to Article V Members<br />
Section 5.02 Membership Privileges<br />
2009 INA Bylaws Proposed . . .<br />
(c) Individual Affiliate members in good standing shall have membership<br />
privileges as follows: An Individual Affiliate is a health care worker,<br />
who is not a registered nurse, but is represented by <strong>the</strong> Illinois <strong>Nurses</strong><br />
Association <strong>for</strong> <strong>the</strong> purpose of collective bargaining and pays dues per<br />
INA/EGW policy.<br />
1) Individual Affiliate privileges are limited to <strong>the</strong> Economic & General<br />
Welfare Commission. Privileges include <strong>the</strong> ability to be appointed to <strong>the</strong><br />
Commission per INA bylaws and <strong>the</strong> ability to vote only <strong>for</strong> <strong>the</strong> members<br />
of <strong>the</strong> Commission on Economic and General Welfare.<br />
2) Individual Affiliate members do not receive benefits from ANA at <strong>the</strong><br />
national level.<br />
continued from page 7<br />
RATIONALE<br />
Currently INA represents health care workers, who are not registered nurses,<br />
in our bargaining units. They are allowed only fair share representation. This<br />
change would allow <strong>for</strong> proper adherence to labor law and ANA bylaws.<br />
Article II Purposes and Functions<br />
Article II Purposes and Functions<br />
Add new Section 2.03 Insulation<br />
CURRENT BYLAW<br />
PROPOSED BYLAW AMENDMENT<br />
Section 2.03 Insulation<br />
It is <strong>the</strong> policy of INA that collective bargaining and subjects related to<br />
collective bargaining shall <strong>com</strong>pletely exclude participation by a supervisor<br />
or managerial employee (within <strong>the</strong> meaning of relevant labor law).<br />
E&GW Commission members must be members of an INA bargaining<br />
unit.<br />
Con<strong>for</strong>mity with labor law.<br />
RATIONALE<br />
CURRENT BYLAW<br />
Article XVIII Commissions<br />
Section 18.10 Commission on<br />
Economic and General Welfare<br />
(a) Composition<br />
(1) All members shall be persons (a) whose functions in nursing are not<br />
primarily managerial in nature and (b) who are eligible <strong>for</strong> collective bargaining<br />
representation under federal and state labor relations laws, decisions, rulings,<br />
and orders including but not limited to <strong>the</strong> Labor Management Relations Act,<br />
Civil Service Re<strong>for</strong>m Act and State Public Employee Relations Act.<br />
PROPOSED BYLAW AMENDMENT<br />
Add new language to Article XVIII Commissions<br />
Section 18.10 Commission on<br />
Economic and General Welfare<br />
This Commission is insulated in accordance with Article II Purposes and<br />
Functions, Section 2.03 Insulation, and relevant federal and state labor<br />
law. Reports to <strong>the</strong> Board of Directors and/or House of Delegates on<br />
confidential subjects related to collective bargaining shall only be given in<br />
insulated session.<br />
(a) Composition<br />
(1) Membership in <strong>the</strong> Commission shall consist of two (2) categories:<br />
1) INA members (a) whose functions in nursing are not primarily<br />
managerial in nature; and, (b) who are eligible <strong>for</strong> collective bargaining<br />
representation under federal and state labor relations laws, decisions, rulings,<br />
and orders, including but not limited to <strong>the</strong> Labor Management Relations Act,<br />
Civil Service Re<strong>for</strong>m Act and State Public Employee Relations Act and are<br />
represented by <strong>the</strong> Illinois <strong>Nurses</strong> Association in a collective bargaining<br />
agreement; and,<br />
2) Individual Affiliates (a) whose functions are not primarily<br />
managerial in nature; and, (b) who are eligible <strong>for</strong> collective bargaining<br />
representation under federal and state labor relations laws, decisions,<br />
rulings, and orders, including but not limited to <strong>the</strong> Labor Management<br />
Relations Act, Civil Service Re<strong>for</strong>m Act and State Public Employee<br />
Relations Act and who pay dues per INA/EGW policy. These Individual<br />
Affiliates will be allowed to participate in discussions that relate to<br />
collective bargaining only.<br />
Con<strong>for</strong>mity with labor law.<br />
RATIONALE
The Illinois Nurse October 2009 Page 11<br />
Continuing Education Offering<br />
Lateral Violence And Bullying In The Workplace<br />
by: Ann O’Sullivan, RN, MSN, CNE, NE-BC<br />
Assistant Dean, Associate Professor<br />
Blessing-Rieman College of Nursing<br />
Chair, Commission on Work<strong>for</strong>ce Advocacy<br />
Illinois <strong>Nurses</strong> Association<br />
Janet Lynch, RN, MSN<br />
Dean of Health Professions<br />
Sauk Valley Community College<br />
Vice-Chair, Commission on Work<strong>for</strong>ce Advocacy<br />
Illinois <strong>Nurses</strong> Association<br />
CE OFFERING<br />
1.5 CONTACT HOURS<br />
---------------------------<br />
This offering expires in 2 years:<br />
March, 2011<br />
----------------------------------<br />
The goal of this continuing education offering is to<br />
provide in<strong>for</strong>mation on violence and bullying in <strong>the</strong><br />
workplace and its implications<br />
The objectives of this article are:<br />
1. Describe Joint Commission concerns and<br />
requirements<br />
2. Define workplace abuse and disruptive behavior<br />
3. List strategies to reduce workplace violence and<br />
bullying<br />
4. Identify what nurses can do<br />
The Illinois <strong>Nurses</strong> Association created <strong>the</strong> Commission<br />
on Work<strong>for</strong>ce Advocacy in 2007. All nurses who are<br />
INA members who are not members through collective<br />
bargaining are represented by this Commission. The core<br />
purpose of <strong>the</strong> WFA program is to articulate, advocate,<br />
and provide work<strong>for</strong>ce advocacy solutions to equip nurses<br />
in shaping <strong>the</strong>ir work environment. Work<strong>for</strong>ce advocacy<br />
is an enabling process whereby nurses are supported by<br />
a variety of programs, services, tools, and resources with<br />
which to influence <strong>the</strong>ir work at <strong>the</strong> Center <strong>for</strong> American<br />
<strong>Nurses</strong>. The mission of <strong>the</strong> Center is to create healthy work<br />
environments through advocacy, education, and research.<br />
If you are interested in having <strong>the</strong> topic “Lateral<br />
Violence and Bullying in <strong>the</strong> Workplace” presented at<br />
your facility, please call <strong>the</strong> INA office.<br />
Since its <strong>for</strong>mation, one of <strong>the</strong> priorities of <strong>the</strong><br />
Commission has been to educate nurses on <strong>the</strong> issues<br />
surrounding workplace violence and bullying. To this end,<br />
we have developed a position paper which is available on<br />
<strong>the</strong> INA website, offered a continuing education program<br />
in March 2009, and now we offer this continuing education<br />
article <strong>for</strong> all nurses in <strong>the</strong> state.<br />
Lateral violence and bullying has been extensively<br />
reported and documented among healthcare professionals,<br />
with serious negative out<strong>com</strong>es <strong>for</strong> registered nurses, <strong>the</strong>ir<br />
patients and health care employers. There may be many<br />
different titles (conflict, horizontal or lateral violence,<br />
incivility, disruptive behavior)—but <strong>the</strong> result is <strong>the</strong><br />
same—behaviors that are toxic to <strong>the</strong> nursing profession<br />
and have a negative impact on retention of quality staff.<br />
It is <strong>the</strong> position of <strong>the</strong> Illinois <strong>Nurses</strong> Association<br />
(INA) that <strong>the</strong>re is no place in a professional practice<br />
environment <strong>for</strong> lateral violence and bullying among<br />
nurses or between healthcare professionals. All healthcare<br />
organizations should implement a zero tolerance policy<br />
related to disruptive behavior, including a professional code<br />
of conduct and educational and behavioral interventions to<br />
assist nurses in addressing disruptive behavior. (Position<br />
paper adapted from <strong>the</strong> Center <strong>for</strong> American <strong>Nurses</strong><br />
position paper, 2008)<br />
Background<br />
The culture of <strong>the</strong> healthcare setting has been<br />
historically populated by images of <strong>the</strong> nurse as a<br />
“handmaiden” in a patriarchal environment (Kelly, 2006,<br />
p.23). The balance of power has not been in <strong>the</strong> nurse’s<br />
favor. Organizations fashioned to be hierarchical have not<br />
fostered a culture of professional collegiality, nor have<br />
<strong>the</strong>y advanced <strong>the</strong> role of nursing. Too often, nurses have<br />
acquiesced to a victim mentality that only facilitates a<br />
sense of powerlessness. <strong>Nurses</strong> have reported concern<br />
about <strong>the</strong> lack of action taken by supervisors in addressing<br />
horizontal violence in <strong>the</strong> workplace (Farrell, 1997; Stanley<br />
et al., 2007).<br />
While not directly addressing bullying or horizontal<br />
violence, Kramer (1974) described <strong>the</strong> “reality shock”<br />
occurring <strong>for</strong> new graduates when <strong>the</strong>y encountered<br />
differences in <strong>the</strong>ir perception of what nursing could be<br />
and <strong>the</strong> actual reality of <strong>the</strong> workplace. Kramer suggested<br />
that “reality shock” can manifest as hopelessness and<br />
dissatisfaction, which is a prelude to conflict in <strong>the</strong><br />
workplace (p. 9). Today, bullying is an international<br />
phenomenon not limited to <strong>the</strong> healthcare arena, and abuse<br />
can also occur between professions. The phrase “nurses<br />
eat <strong>the</strong>ir young,” has been used to describe <strong>the</strong> negative<br />
behaviors directed toward new nurses (Rowe & Sherlock,<br />
2005). Griffin (2004) described <strong>the</strong> vulnerability of newly<br />
licensed nurses as <strong>the</strong>y are socialized into <strong>the</strong> nursing<br />
work<strong>for</strong>ce; lateral violence affected <strong>the</strong>ir perception of<br />
whe<strong>the</strong>r to remain in <strong>the</strong>ir current position.<br />
Sofield and Salmond (2003) found that primarily<br />
physicians, <strong>the</strong>n patients, and patients’ families were<br />
responsible <strong>for</strong> most of <strong>the</strong> verbal abuse towards nurses.<br />
One-third of respondents expressed <strong>the</strong>y would consider<br />
resignation in response to verbal abuse; it was concluded<br />
that nurses lacked <strong>the</strong> skills to deal with <strong>the</strong> verbal<br />
abuse and perceived <strong>the</strong>mselves as powerless to change<br />
organizational response (Sofield & Salmond, 2003).<br />
Cox found <strong>the</strong> most frequent source of verbal abuse was<br />
physicians, and in descending order patients, families and<br />
peers, supervisors and subordinates (1991). The turnover<br />
attributed to verbal abuse was 24 percent <strong>for</strong> staff nurses<br />
and 25 percent <strong>for</strong> nurse managers (Cox, 1991b). Cook,<br />
Green and Topp (2001) found that perioperative nurses<br />
encountered verbal abuse by physicians. However, Rowe<br />
and Sherlock (2005) reported that nurses in particular were<br />
<strong>the</strong> most frequent source of verbal abuse towards o<strong>the</strong>r<br />
nurses. Patients’ families were <strong>the</strong> second most frequent<br />
source, followed by physicians and <strong>the</strong>n patients (Rowe &<br />
Sherlock, 2005).<br />
In a hostile environment, <strong>com</strong>munication is hindered<br />
and this can affect quality of care and patient safety<br />
(Joint Commission on Accreditation of Health care<br />
Organizations, 2002). Healthcare providers report<br />
intimidation does alter <strong>com</strong>munication and negatively<br />
impacts patient care and safety (Institute <strong>for</strong> Safe<br />
Medication Practices, 2004). Healthcare professionals<br />
facing intimidation may sometimes choose to abdicate<br />
<strong>the</strong>ir advocacy role to avoid intimidating behaviors,<br />
impacting patient safety. The Institute <strong>for</strong> Safe Medication<br />
Practices survey (2004) revealed that more experienced<br />
nurses were more likely to encounter intimidating<br />
behaviors; differences in intimidating encounters were<br />
not appreciably different in terms of gender, but females<br />
were more likely to ask ano<strong>the</strong>r colleague to talk with <strong>the</strong><br />
intimidator <strong>for</strong> <strong>the</strong>m. The organization’s effectiveness in<br />
handling intimidation was viewed less favorably by those<br />
nurses and pharmacists with more years of practice in that<br />
facility (Institute <strong>for</strong> Safe Medication Practices, 2004a).<br />
Conflict in <strong>the</strong> workplace results in serious negative<br />
out<strong>com</strong>es <strong>for</strong> registered nurses and o<strong>the</strong>r healthcare<br />
professionals, organizations, and patients. The Joint<br />
Commission (2007) acknowledges that unresolved conflict<br />
and disruptive behavior can adversely affect safety and<br />
quality of care. Additionally, healthcare organizations are<br />
grappling with a continuing nursing shortage today and<br />
it is projected to grow worse as nurses retire (American<br />
Association of Colleges of <strong>Nurses</strong>, 2007). Bullying and<br />
lateral violence have a negative impact on <strong>the</strong> ability of<br />
<strong>the</strong> nursing profession to retain both new and long-term<br />
colleagues.<br />
Intimidation and disruptive behaviors can foster<br />
medical errors, contribute to poor patient satisfaction and<br />
to preventable adverse out<strong>com</strong>es, increase <strong>the</strong> cost of care,<br />
and cause qualified clinicians, administrators and managers<br />
to seek new positions in more professional environments.<br />
Safety and quality of patient care is dependent on<br />
teamwork, <strong>com</strong>munication and a collaborative work<br />
environment. To ensure quality and promote a culture of<br />
safety, healthcare organizations must address <strong>the</strong> problem<br />
of behaviors that threaten <strong>the</strong> per<strong>for</strong>mance of <strong>the</strong> health<br />
care team. (Joint Commission, 2008).<br />
Effective January 1, 2009, <strong>the</strong> Joint Commission has<br />
a new Leadership standard that addresses disruptive and<br />
inappropriate behaviors: “EP 4: The hospital/organization<br />
has a code of conduct that defines acceptable and<br />
disruptive and inappropriate behaviors; and EP 5: Leaders<br />
create and implement a process <strong>for</strong> managing disruptive<br />
and inappropriate behaviors” (Joint Commission, 2008,<br />
p.2). In addition, standards to <strong>the</strong> medical staff this<br />
chapter has been revised to include interpersonal skills<br />
and professionalism in <strong>the</strong> credentialing process. Joint<br />
Commission also presents several o<strong>the</strong>r suggested actions,<br />
including: educating all team members on appropriate<br />
professional behavior, holding all team members<br />
accountable <strong>for</strong> modeling desirable behaviors, “zero<br />
tolerance” <strong>for</strong> intimidating or disruptive behaviors, develop<br />
policies and processes <strong>for</strong> addressing disruptive behaviors.<br />
(Joint Commission, 2008)<br />
Strategies to Reduce Workplace Violence and Bullying<br />
First, nursing must recognize <strong>the</strong> need <strong>for</strong> cultural<br />
change to eliminate <strong>the</strong> effects of disruptive behavior,<br />
including lateral violence and bullying at <strong>the</strong> personal,<br />
organizational, national and international levels. Suggested<br />
improvements include interdisciplinary collaboration,<br />
<strong>com</strong>munication and opportunities <strong>for</strong> education and<br />
training to address disruptive behavior by physicians<br />
(Rosenstein, 2002). In a cognitive rehearsal strategy<br />
proposed by Griffin (2004), nurses were taught to delay<br />
automatic thoughts, and respond differently through<br />
empowerment strategies to address lateral violence.<br />
Gerardi (2004) described <strong>the</strong> use of mediation techniques<br />
to identify conflict early and develop a plan to resolve it<br />
by listening, reframing <strong>the</strong> concerns raised, identifying<br />
<strong>com</strong>monalities and clearly defining decisions. Developing<br />
a critical mass of diverse professionals trained in conflict<br />
management can not only reduce lateral violence and<br />
bullying, but it can also assist with o<strong>the</strong>r potential conflict<br />
situations, such as, error disclosure issues and process<br />
reviews.<br />
The Institute of Safe Medication Practices (2004b)<br />
suggested organizational strategies: development of<br />
a multidisciplinary group that will survey staff about<br />
behaviors, develop educational opportunities, establish a<br />
standard method <strong>for</strong> collaborative <strong>com</strong>munication and zero<br />
tolerance <strong>for</strong> intimidation, in addition to being models <strong>for</strong><br />
and rewarding positive behaviors.<br />
Scott (2009) re<strong>com</strong>mends 10 actions to deal with<br />
disruptive (bullying behaviors):<br />
1. Know what behaviors can be disruptive—both<br />
overt and passive behaviors can be violent, such<br />
as name-calling, frequent put downs, withholding<br />
in<strong>for</strong>mation, rolling eyes, heavy sighing, verbal<br />
abuse, constant criticism, physical intimidation,<br />
etc.<br />
2. Know when to engage—When <strong>the</strong> conflict is<br />
ongoing or recurring; when it’s creating a potential<br />
threat to o<strong>the</strong>rs; when <strong>the</strong> conflict keeps you awake<br />
at night.<br />
3. Avoid Avoidance—even though you may not know<br />
how to do it well, or you have a fear of retaliation,<br />
or time constraints.<br />
4. Be mindful of you own feelings—BREATHE<br />
and focus on what’s happening inside and out; be<br />
empa<strong>the</strong>tic; think be<strong>for</strong>e saying something.<br />
5. Take immediate interventions when witnessing<br />
disruptive behavior—acknowledge that <strong>the</strong>y are<br />
Lateral Violence & Bullying continued on page 12
Page 12 October 2009 The Illinois Nurse<br />
upset, set limits. Arrange to talk when everyone is<br />
less stressed.<br />
6. Learn to listen—this is <strong>the</strong> most important part of<br />
dealing with conflict; hearing with intent; listen<br />
with your heart and your gut; takes practice.<br />
7. Collaborate with your boss—ask <strong>for</strong> assistance in<br />
role playing.<br />
8. Behave differently—choose constructive behavior<br />
over avoidance; understand your role in disruptive<br />
behaviors; do not resort to old, ineffective<br />
behaviors.<br />
9. Reflect on <strong>the</strong> experience—reflect on a recent<br />
experience with disruptive behavior—why did it<br />
matter to you? How did you feel? What could you<br />
have done differently?<br />
10. Remember—it’s all about you—not about <strong>the</strong>m!<br />
The INA re<strong>com</strong>mends <strong>the</strong> following strategies to<br />
eliminate disruptive behavior (lateral violence and<br />
bullying):<br />
<strong>Nurses</strong><br />
1. <strong>Nurses</strong> and nurse leaders, managers and<br />
supervisors adopt and model professional ethical<br />
behavior.<br />
2. Recognize and appropriately address bullying<br />
and disruptive behavior in <strong>the</strong> workplace through<br />
enhanced conflict management and conflict<br />
resolution.<br />
3. Reflect on your own behavior and <strong>com</strong>municate<br />
respectfully with each o<strong>the</strong>r. Participate in<br />
collaborative interdisciplinary initiatives to prevent<br />
abuse.<br />
4. Work to ensure <strong>the</strong> mission, vision and values of<br />
<strong>the</strong>ir workplaces that are reflective of <strong>the</strong> Code of<br />
Ethics <strong>for</strong> <strong>Nurses</strong> (American <strong>Nurses</strong> Association,<br />
2001) and standards set by <strong>the</strong> profession, in order<br />
Continuing Education Offering<br />
Lateral Violence & Bullying continued from page 11 to eliminate disruptive behavior (lateral violence behaviors.<br />
and bullying).<br />
2. Build on previous and current studies while<br />
seeking to explore innovative interventions on how<br />
to eliminate manifestations of disruptive behaviors.<br />
3. Evaluate <strong>the</strong> efficacy of promising strategies in<br />
eliminating disruptive behaviors (lateral violence<br />
and bullying) from <strong>the</strong> workplace.<br />
Employers/Healthcare Organizations<br />
1. Implement zero tolerance policies that address<br />
disruptive behaviors (lateral violence and bullying)<br />
and indicate such behaviors will not be tolerated.<br />
The organizations should adopt zero tolerance<br />
policies that include appropriate investigation<br />
and due process necessary to provide adequate<br />
safeguards to nurses and o<strong>the</strong>rs who are accused of<br />
lateral violence or bullying.<br />
2. Promote a Culture of Safety that encourages open<br />
and respectful <strong>com</strong>munication among all healthcare<br />
providers and staff (The Joint Commission, 2007).<br />
3. Provide support to any individual impacted by<br />
lateral violence and/or bullying.<br />
4. Provide education and counseling to victims<br />
and <strong>the</strong> perpetrators of horizontal violence and<br />
bullying.<br />
Nursing Continuing Education and Academic Programs<br />
1. Disseminate in<strong>for</strong>mation to nurses and students<br />
that address conflict and provide in<strong>for</strong>mation<br />
about how to change disruptive behavior in <strong>the</strong><br />
workplace.<br />
2. Implement continuing education programs related<br />
to bullying and lateral violence and interventions<br />
to address such behaviors.<br />
3. Develop educational programs regarding bullying<br />
and strategies on how to recognize and address<br />
such disruptive behavior.<br />
4. Develop and implement curricula that educate<br />
nursing students on <strong>the</strong> incidence of disruptive<br />
behaviors including lateral violence and bullying,<br />
along with steps to take to eradicate this behavior.<br />
Nursing Research<br />
1. Continue to research <strong>the</strong> contributing factors<br />
and <strong>the</strong> process of lateral violence and bullying<br />
INA as a Nursing Policy Maker<br />
1. Support policy, development of legislation,<br />
regulations and standards that promote a culture of<br />
safety <strong>for</strong> patient care and discourage all <strong>for</strong>ms of<br />
disruptive behavior, including lateral violence and<br />
bullying.<br />
2. Continue its work to assure that nurses influence<br />
legislative initiatives, accreditation standards and<br />
policies through active participation in <strong>the</strong> policy<br />
process (International Council of <strong>Nurses</strong>, 2000).<br />
Conclusion<br />
INA recognizes that lateral violence and bullying<br />
in <strong>the</strong> workplace is a serious problem. It is imperative<br />
that <strong>the</strong> profession of nursing addresses this problem to<br />
improve <strong>the</strong> recruitment and retention of nurses. The<br />
ef<strong>for</strong>ts to improve patient care are inextricably linked to<br />
<strong>the</strong> work environment of nurses (Institute of Medicine,<br />
2004). Disruptive behaviors of health care providers<br />
are not conducive to a culture of safety. The evidence is<br />
clear that disruptive behaviors such as lateral violence<br />
and bullying are serious problems that negatively impact<br />
<strong>the</strong> work environment of nurses. This problem is broad<br />
reaching and has clear implications in <strong>the</strong> current and<br />
future projected shortage of nurses, as well as <strong>the</strong> safety<br />
and quality of patient care. It has an impact on <strong>the</strong> ability<br />
of <strong>the</strong> profession to recruit new members and <strong>the</strong> ability<br />
of health care organizations and o<strong>the</strong>r employers to retain<br />
nurses.<br />
Lateral Violence & Bullying continued on page 13
The Illinois Nurse October 2009 Page 13<br />
Lateral Violence & Bullying continued from page 12<br />
HOW TO EARN<br />
CONTINUING EDUCATION CREDIT<br />
This course is 1.5 Contact Hours<br />
1. Read <strong>the</strong> Continuing Education Article<br />
2. Take <strong>the</strong> test on <strong>the</strong> next page.<br />
Complete <strong>the</strong> entire <strong>for</strong>m<br />
DEADLINE<br />
Answer <strong>for</strong>ms must be postmarked by<br />
March 1, 2011<br />
3. Mail or fax <strong>the</strong> <strong>com</strong>pleted answer <strong>for</strong>m.<br />
Include processing fee as follows:<br />
INA members- $7.50<br />
Non members- $15.00<br />
Check or money order payable to INA or credit card<br />
in<strong>for</strong>mation only<br />
MAIL: Illinois <strong>Nurses</strong> Association<br />
Attn: Sharon Canariato<br />
105 W. Adams, Suite 2101<br />
Chicago, IL 60603<br />
FAX: Credit Card Payments Only<br />
312-419-2920<br />
ACHIEVEMENT<br />
• To earn 1.5 contact hours of continuing education,<br />
you must achieve a score of 75%<br />
• If you do not pass <strong>the</strong> test, you may<br />
take it again at no additional charge.<br />
• Certificates indicating successful <strong>com</strong>pletion<br />
of this offering will be emailed to you<br />
ACCREDITATION<br />
Illinois <strong>Nurses</strong> Association is an approved provider of<br />
continuing nursing education<br />
by <strong>the</strong> Georgia <strong>Nurses</strong> Association, an accredited<br />
approver by <strong>the</strong><br />
American <strong>Nurses</strong> Credentialing Center’s<br />
Commission on Accreditation.<br />
Continuing Education Offering<br />
TEST QUESTIONS:<br />
1. Conflict in <strong>the</strong> workplace results in serious negative out<strong>com</strong>es <strong>for</strong> registered nurses and o<strong>the</strong>r healthcare professionals, organizations, and<br />
patients.<br />
True<br />
False<br />
2. Examples of disruptive/bullying behaviors include:<br />
a. name-calling<br />
b. rolling eyes<br />
c. constant criticism<br />
d. blaming<br />
e. all of <strong>the</strong> above<br />
3. The most important part of dealing with conflict is:<br />
a. Know when to engage<br />
b. Avoid avoidance<br />
c. Learn to listen<br />
d. Collaborate with your boss<br />
4. The Joint Commission requires organizations to:<br />
a. Create and implement a process <strong>for</strong> managing disruptive and inappropriate behaviors<br />
b. Education <strong>for</strong> all team members on appropriate professional behaviors<br />
c. Implementing a zero tolerance policy <strong>for</strong> intimidating behaviors<br />
d. Hold all team members accountable <strong>for</strong> modeling desirable behaviors<br />
5. The Illinois <strong>Nurses</strong> Association re<strong>com</strong>mends that health care organizations:<br />
a. Implement zero tolerance policies that address disruptive behaviors (lateral violence and bullying) and indicate such behaviors will<br />
not be tolerated.<br />
b. Promote a Culture of Safety that encourages open and respectful <strong>com</strong>munication among all healthcare providers and staff<br />
c. Provide support to any individual impacted by lateral violence and/or bullying.<br />
d. Provide education and counseling to victims and <strong>the</strong> perpetrators of horizontal violence and bullying.<br />
e. All of <strong>the</strong> above<br />
(Submit entire <strong>for</strong>m below <strong>for</strong> contact hours)<br />
ANSWER FORM<br />
CE #15: Lateral Violence & Bullying in <strong>the</strong> Workplace<br />
Please circle <strong>the</strong> appropriate letter<br />
1. A B<br />
2. A B C<br />
3. A B C<br />
4. A B C D<br />
5. A B<br />
6. A B C D<br />
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -<br />
(Please PRINT clearly)<br />
Name: _______________________________________________________________________________________________________________<br />
Address: _____________________________________________________________________________________________________________<br />
City: ________________________________________________________________ State: _____________ Zip: ____________________<br />
Phone: _________________________________________________ Email Address: _____________________________________________<br />
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -<br />
Evaluation- CE 0309-15<br />
Strongly Agree (5) Strongly Disagree (1)<br />
Learner achievement of objectives:<br />
1. Describe Joint Commission concerns and requirements 5 4 3 2 1<br />
2. Define workplace abuse and disruptive behavior 5 4 3 2 1<br />
3. List strategies to reduce workplace violence and bullying 5 4 3 2 1<br />
4. Identify what nurses can do 5 4 3 2 1<br />
How many minutes did it take you to read and <strong>com</strong>plete this program? ___________________________________________________________<br />
Suggestions <strong>for</strong> improvement? <strong>Future</strong> topics? _______________________________________________________________________________<br />
METHOD OF PAYMENT<br />
❑ INA Member ($7.50) INA ID# ________________________________________________<br />
❑ Non Member ($15.00)<br />
❑ Money Order ❑ Check ❑ VISA ❑ Master Card ❑ American Express<br />
(note: a fee of $25 will be assessed <strong>for</strong> any returned checks)<br />
Card account number: ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____<br />
Credit card expiration date: ____ ____ / ____ ____<br />
Signature __________________________________________________________ Date _______________________<br />
Mail all tests to: INA, Attn: Sharon Canariato, 105 W. Adams, Sute 2101, Chicago, IL 60603References<br />
American Association of Colleges of <strong>Nurses</strong>. (2007). Nursing Shortage. Retrieved December 4, 2007, from http://www.aacn.nche.edu/Media/FactSheets/Nursing/<br />
Shortage.htm<br />
American <strong>Nurses</strong> Association. (2001). Code of ethics <strong>for</strong> nurses with interpretive statements. Silver Spring, MD.: American <strong>Nurses</strong> Association.<br />
Center <strong>for</strong> American <strong>Nurses</strong>. (2007). Bullying in <strong>the</strong> workplace: Reversing a culture. Silver Spring, MD: Center <strong>for</strong> American <strong>Nurses</strong>.<br />
Center <strong>for</strong> American <strong>Nurses</strong>. (2008). Lateral violence and bullying in <strong>the</strong> workplace. Retrieved July 30, 2008, from http://www.center<strong>for</strong>americannurses.org.<br />
Cook, J. K., Green, M., & Topp, R. V. (2001). Exploring <strong>the</strong> impact of physician verbal abuse on perioperative nurses. AORN Journal, 74(3),317-318,320,322-327,329-<br />
330.<br />
Cox, H. (1991a). Verbal abuse nationwide: oppressed group behavior. Part 1. Nursing Management, 22(2), 32-35.<br />
Cox, H. (1991b). Verbal abuse nationwide: impact and modifications. Part 2. Nursing Management, 22(3), 66-69.<br />
Farrell, G. A. (1997). Aggression in clinical settings: nurses’ views. Journal of Advanced Nursing, 25(3); 501-508.<br />
Gerardi, D. (2004). Using mediation techniques to manage conflict and create healthy work environments. AACN Clinical Issues: Advanced Practice in Acute &<br />
Critical Care, 5(2), 182-195.<br />
Griffin, D. (2004). Teaching cognitive rehearsal as a shield <strong>for</strong> lateral violence: an intervention <strong>for</strong> newly licensed nurses. The Journal of Continuing Education in<br />
Nursing, 35(6), 257-263.<br />
Institute <strong>for</strong> Safe Medication Practices. (2004a). Intimidation: Practitioners speak up about this unresolved problem (part I). March 11. Retrieved January 9, 2006,<br />
from<br />
http://www.ismp.org.newsletterslacutecare/articles/2004031l_2.asp<br />
Institute <strong>for</strong> Safe Medication Practices. (2004b). Intimidation: Mapping a Plan <strong>for</strong> Cultural Change in Healthcare (part ll). March 25. Retrieved January 9, 2006, from<br />
http://www.ismp.org newsletters/acutecare/articlesl20040325.asp<br />
Institute of Medicine. (2004). Keeping patients safe: Trans<strong>for</strong>ming <strong>the</strong> work environment of nurses. Washington, DC: The National Academies Press.<br />
International Council of <strong>Nurses</strong> (2000). Participation of nurses in health services decision making and policy development. ICN Position Statement. Retrieved from<br />
July 26, 2007 http://www.icn.ch/pspolicvdevOO.htm<br />
Joint Commission. (2002). Health care at <strong>the</strong> crossroads: Strategies <strong>for</strong> addressing <strong>the</strong> evolving nursing crisis. Retrieved December 4, 2007, from http://www.<br />
joint<strong>com</strong>mission.org/NR/rdonlyres/5C138711-ED76-4D6F-909F- B06E0309F36D/0/health care at <strong>the</strong> crossroads.pdf<br />
Joint Commission. (2007). Leadership Chapter. Retrieved January 7, 2007 from http:/ /www.joint<strong>com</strong>mission.org/Accreditation Programs/Hospitals/Standards/hap_<br />
prepub_stds.htm<br />
Joint Commission. (2008). Sentinel Event Alert. Retrieved October 3, 2008 from http:/ /www.joint<strong>com</strong>mission.org/SentinelEvents/SentinelEventAlert/sea_40.htm<br />
Kelly, J. (2006). An overview of conflict. Dimensions of Critical Care Nursing, 25(1), 22-28.<br />
Kramer, M.. (1974). Reality Shock: Why nurses leave nursing (1st Ed.). St. Louis, MO: The CV Mosby Company.<br />
Rosenstein, A. H. (2002). Nurse-physician relationships: impact on nurse satisfaction and retention. American Journal of Nursing, 102(6), 26-34.<br />
Rowe, M. M., & Sherlock, H. (2005). Stress and verbal abuse in nursing: do burned out nurses eat <strong>the</strong>ir young? Journal of Nursing Management, 13(3), 242-248.<br />
Sofield, L., & Salmond, S. W. (2003). Work Place violence: a focus on verbal abuse and intent to leave <strong>the</strong> organization. Orthopaedic Nursing, 22(4), 274-283.<br />
Scott, D. (2009). Ten tips <strong>for</strong> addressing disruptive behavior. Retrieved May 10, 2008 from www.center<strong>for</strong>americannurses.<strong>com</strong>.<br />
Stanley, K. M., Martin, M. M., Michel, Y., Welton, J. M., & Nemeth, L. S. (2007). Examining lateral violence in <strong>the</strong> nursing work<strong>for</strong>ce. Issues in Mental Health<br />
Nursing, 28, 1247-1265.<br />
The Joint Commission. (2007). Pre-publication standards <strong>for</strong> critical access hospitals. Oakbrook Terrace, IL: Author. Retrieved February 15, 2008, from<br />
www.joint<strong>com</strong>mission.org/AccreditationPrograms/ CriticalAccessHospitals/Standards/cah_prepub _stds.htm
Page 14 October 2009 The Illinois Nurse<br />
ILLINOIS HIV CARE<br />
CONNECT<br />
<strong>Nurses</strong>, O<strong>the</strong>r Care Providers Can Refer HIV-Positive<br />
Individuals to Statewide Care Network<br />
<strong>Nurses</strong> and o<strong>the</strong>r health care providers are encouraged to<br />
refer HIV-positive individuals to one of eight regional offices<br />
of Illinois HIV Care Connect—www.hivcareconnect.<strong>com</strong>.<br />
“Illinois HIV Care Connect extends <strong>the</strong> ability of health<br />
care providers and o<strong>the</strong>rs to help people living with HIV find<br />
<strong>the</strong> services <strong>the</strong>y need to achieve optimal health and selfsufficiency,”<br />
said Jim Nelson, executive director of <strong>the</strong> Illinois<br />
Public Health Association.<br />
Once enrolled in Illinois HIV Care Connect, people living<br />
with HIV receive confidential medical case management<br />
services at no charge, regardless of in<strong>com</strong>e. Also, <strong>the</strong>y may<br />
quality <strong>for</strong> a range of o<strong>the</strong>r health care and support services.<br />
In an ef<strong>for</strong>t to curb a still-serious HIV infection epidemic<br />
in Illinois, <strong>the</strong> Illinois Public Health Association recently<br />
introduced Illinois HIV Care Connect to increase awareness<br />
about <strong>the</strong> statewide network of services <strong>for</strong> HIV-positive<br />
individuals.<br />
Funded by <strong>the</strong> Illinois Department of Public Health through<br />
federal Ryan White Part B grants, Illinois HIV Care Connect’s<br />
regional offices are located in Belleville, Champaign, Chicago<br />
(two regional offices), Murphysboro, Peoria, Rock<strong>for</strong>d, and<br />
Springfield. For more in<strong>for</strong>mation on local offices, go to http://<br />
www.hivcareconnect.<strong>com</strong>/connect.html<br />
Increasing awareness of HIV-related services among nurses<br />
and o<strong>the</strong>r health providers is a primary goal of <strong>the</strong> initiative,<br />
Nelson said. “Our new Web site has detailed in<strong>for</strong>mation about<br />
<strong>the</strong> enormous resources provided by <strong>the</strong> statewide network,”<br />
he adds.<br />
People living with HIV who enroll in Illinois HIV Care<br />
Connect may qualify <strong>for</strong> outpatient medical care, mental<br />
health care, oral health care, medical nutritional <strong>the</strong>rapy,<br />
substance abuse prevention and counseling, and o<strong>the</strong>r support<br />
services. “Illinois HIV Care Connect serves as a one-stop shop<br />
<strong>for</strong> all <strong>the</strong>se services,” said Valerie Webb, IPHA president.<br />
Getting HIV-positive individuals to take advantage of <strong>the</strong>se<br />
services helps to curb <strong>the</strong> spread and progression of HIV, Webb<br />
said. “It’s important that HIV-positive individuals receive <strong>the</strong><br />
medical treatments <strong>the</strong>y need to slow <strong>the</strong> progression of HIV.<br />
They also need to know <strong>the</strong> precautions <strong>the</strong>y should take to<br />
prevent <strong>the</strong> spread of <strong>the</strong> infection to o<strong>the</strong>rs.”<br />
In addition to reaching out to health care providers, Illinois<br />
HIV Care Connect also will encourage corrections officials to<br />
refer HIV-positive individuals because HIV infection within<br />
<strong>the</strong> prison population is five times higher than among <strong>the</strong><br />
general public, Nelson said.<br />
HIV infection still a serious problem in Illinois<br />
HIV infection can progress to AIDS and o<strong>the</strong>r diseases.<br />
Illinois has <strong>the</strong> nation’s seventh highest cumulative number of<br />
AIDS cases, according to <strong>the</strong> Illinois Department of Public<br />
Health, with more than 36,000 reported cases and 18,500<br />
deaths since 1981.<br />
About one-quarter—or 10,000—of <strong>the</strong> 40,000 HIVpositive<br />
Illinois residents do not know <strong>the</strong>y are HIV-positive,<br />
<strong>the</strong> department estimates. Unaware of <strong>the</strong>ir HIV infection,<br />
undiagnosed individuals spread HIV to o<strong>the</strong>rs through<br />
unprotected sex, intravenous drug use, or o<strong>the</strong>r ways.<br />
Undiagnosed individuals also do not receive <strong>the</strong> benefit of<br />
medical treatments that can slow <strong>the</strong> progression of HIV<br />
infection into AIDS or o<strong>the</strong>r illnesses.<br />
To stop <strong>the</strong> progression and transmission of HIV-related<br />
disease, <strong>the</strong> U.S. Centers <strong>for</strong> Disease Control and Prevention<br />
(CDC) has re<strong>com</strong>mended that all individuals age 13-64 be<br />
tested <strong>for</strong> HIV infection. Those wishing not to be tested<br />
can choose to decline or “opt-out.” As a result, <strong>the</strong> Illinois<br />
Department of Public Health expects that increased numbers<br />
of individuals will be diagnosed as HIV-positive, making<br />
referrals to HIV Care Connect an important way to contain<br />
<strong>the</strong> progression and spread of HIV infection.<br />
Teaching Evidence-Based Cultural Competence in<br />
Nursing Education: A Case Study<br />
Ann O’Sullivan, MSN, RN, CNE, NE-BC<br />
Assistant Dean, Associate Professor<br />
Blessing-Rieman College of Nursing<br />
Quincy IL<br />
In 2007, during major curriculum revision discussions,<br />
Blessing-Rieman College of Nursing decided to add a<br />
course on Cultural Competency to <strong>the</strong> senior level <strong>for</strong><br />
all nursing students. This was based on an assessment of<br />
our students and <strong>the</strong>ir level of knowledge about cultural<br />
issues and <strong>the</strong>ir patients. The Institute of Medicine (IOM)<br />
(2001) reported on <strong>the</strong> evidence of unequal treatment<br />
of racial and ethnic minorities in health care. The IOM<br />
(2005) and <strong>the</strong> Sullivan Commission (2004) reported that<br />
health disparities were attributed to patient characteristics,<br />
practitioner bias and systematic factors which all point<br />
to <strong>the</strong> need <strong>for</strong> education <strong>for</strong> all health care practitioners.<br />
Faculty who were preparing to teach this new course,<br />
did an extensive literature review, studied and attended<br />
conferences on this topic to be prepared to start teaching a<br />
one hour online course in <strong>the</strong> fall of 2008.<br />
What is Cultural Competence?<br />
The American <strong>Nurses</strong> Association defines cultural<br />
diversity as “Difference between people based on a shared<br />
ideology and valued set of beliefs, norms, customs, and<br />
meanings experienced in a way of life” (ANA, 1991).<br />
The definitions of Cultural Competence that were chosen<br />
<strong>for</strong> <strong>the</strong> course are: 1.) “A process in which <strong>the</strong> health<br />
care provider continuously strives to achieve <strong>the</strong> ability<br />
to effectively work within <strong>the</strong> cultural context of a client/<br />
individual, or family, or <strong>com</strong>munity (Campinha-Bacote,<br />
2002); and 2.) “The ongoing capacity of healthcare<br />
systems, organizations, and professionals to provide <strong>for</strong><br />
diverse populations high quality care that is family- and<br />
patient-centered and equitable” (National Quality Forum,<br />
2008). Leininger (2002) defines culturally <strong>com</strong>petent<br />
care as “Those cognitively based assistive, supportive,<br />
facilitative, or enabling acts or decisions that are tailor<br />
made to fit with <strong>the</strong> individual, group, or institutional<br />
cultural values, beliefs, and lifeways in order to provide or<br />
support meaningful, beneficial, and satisfying health care<br />
or well-being services.” These definitions served as <strong>the</strong><br />
foundation <strong>for</strong> <strong>the</strong> course learning objectives.<br />
National Standards <strong>for</strong> Culturally Competent Care<br />
The U.S. Office of Minority Health (2001) issued<br />
The National Standards <strong>for</strong> Culturally Competent and<br />
Linguistically Appropriate Services (CLAS) in Health<br />
Care, which established standards in 3 specific areas:<br />
Culturally <strong>com</strong>petent care, Language access services, and<br />
organizational supports.<br />
The American <strong>Nurses</strong> Association (1991) states “nurses<br />
need to understand:<br />
• How cultural groups understand life processes;<br />
• How cultural groups define health and illness;<br />
• What cultural groups do to maintain wellness;<br />
• What cultural groups believe to be <strong>the</strong> causes of<br />
illness;<br />
• How healers cure and care <strong>for</strong> members of cultural<br />
groups; and<br />
• How <strong>the</strong> cultural background of <strong>the</strong> nurse influences<br />
<strong>the</strong> way in which care is delivered;”<br />
The American Association of Colleges of Nursing<br />
(AACN) identifies five key <strong>com</strong>petencies considered to be<br />
essential <strong>for</strong> baccalaureate nursing graduates to provide<br />
culturally <strong>com</strong>petent care (2008) which <strong>for</strong>med <strong>the</strong> basics<br />
<strong>for</strong> <strong>the</strong> course:<br />
• Apply knowledge of social and cultural factors<br />
that affect nursing and health care across multiple<br />
contexts<br />
• Use relevant data sources and best evidence in<br />
providing culturally <strong>com</strong>petent care<br />
• Promote achievement of safe and quality out<strong>com</strong>es<br />
<strong>for</strong> diverse populations<br />
• Advocate <strong>for</strong> social justice, including <strong>com</strong>mitment<br />
to <strong>the</strong> health of vulnerable populations and <strong>the</strong><br />
elimination of health disparities<br />
• Participate in continuous cultural <strong>com</strong>petence<br />
development<br />
Curriculum Development<br />
The Health Resources and Service Administration<br />
(HRSA) provides an invaluable resource in <strong>the</strong> document<br />
“Trans<strong>for</strong>ming <strong>the</strong> Face of Health Professions Through<br />
Cultural and Linguistic Competence Education: The<br />
Role of <strong>the</strong> HRSA Centers of Excellence. Key factors <strong>for</strong><br />
curriculum development include: 1.) Developing faculty<br />
<strong>com</strong>mitment to implementing cultural and linguistic<br />
<strong>com</strong>petency education was essential <strong>for</strong> learning to occur.<br />
While we do not have ethnic and racial diversity on our<br />
faculty, <strong>the</strong> course faculty spent much time learning about<br />
cultural <strong>com</strong>petence issues. 2.) The rationale <strong>for</strong> increasing<br />
cultural <strong>com</strong>petence through our curriculum was very<br />
evident to <strong>the</strong> entire faculty, and it was an essential<br />
<strong>com</strong>ponent of <strong>the</strong> first modules of <strong>the</strong> course. 3.) As this<br />
course was taught in <strong>the</strong> senior year, it became increasingly<br />
evident to <strong>the</strong> faculty that a more developmental learning<br />
path was required <strong>for</strong> <strong>the</strong> students to fully engage and<br />
attain <strong>the</strong> required <strong>com</strong>petencies. The HRSA document<br />
supports this: “…multicultural content cannot and should<br />
not be taught in just one course or workshop, but needs to<br />
be rein<strong>for</strong>ced in many different ways over <strong>the</strong> course of <strong>the</strong><br />
students’ education.” After one year of requiring <strong>the</strong> course<br />
<strong>for</strong> seniors, this separate course was dropped, and specific<br />
content was incorporated into each nursing course. This<br />
content includes: a.) attitudes about racism, homophobia,<br />
prejudices and biases of all kinds are openly discussed;<br />
b.) skills in cross-cultural <strong>com</strong>munication. 4.) The faculty<br />
continues to work on integrating cultural and linguistic<br />
topics into existing courses. The toolkit developed by<br />
HRSA has proven invaluable.<br />
A sample curriculum developed by <strong>the</strong> American<br />
Medical Student Association (2006) has also been very<br />
helpful in developing essential content to integrate across<br />
<strong>the</strong> curriculum:<br />
• Definition of Culture and Cultural Competency<br />
• Definition of Diversity and Diverse Population<br />
• Issues in Health Care: The Impact of Diversity<br />
• Cultural Models of Health, Disease and Illness<br />
• Cultural/Traditional Health Care Practices<br />
• Negotiating Cultural Conflicts in <strong>the</strong> Doctor-Patient<br />
Relationship<br />
Teaching strategies that are suggested in this curriculum<br />
include: interviewing and <strong>com</strong>munication, using<br />
interpreters, taking a cultural profile/history, case studies<br />
and videos.<br />
The AACN position paper Cultural Competency in<br />
Baccalaureate Nursing Education (2008) provided <strong>the</strong><br />
most guidance in <strong>the</strong> course development. The essential<br />
<strong>com</strong>petencies as outlined above, serve as <strong>the</strong> framework<br />
<strong>for</strong> <strong>the</strong> course and <strong>for</strong> integrating content and learning<br />
experiences into existing courses. The Toolkit of Resources<br />
<strong>for</strong> Cultural Competent Education <strong>for</strong> Baccalaureate<br />
<strong>Nurses</strong> (2008) provides nursing models; classroom and<br />
clinical teaching strategies; curricular resources such as<br />
case studies, websites, sample curricula; evidence-based<br />
practice resources; research of culturally <strong>com</strong>petent<br />
interventions; and extensive reference and website lists.<br />
Models of Cultural Competence in Nursing Curricula<br />
There are a variety of nursing models <strong>for</strong> teaching<br />
Cultural Competence. We chose Purnell’s Model of<br />
Transcultural Health Care as <strong>the</strong> primary model. Purnell<br />
conceptualizes <strong>the</strong> development of cultural <strong>com</strong>petence<br />
along an upward curve of learning and practice from<br />
a stage of unconscious in<strong>com</strong>petence to conscious<br />
in<strong>com</strong>petence, to conscious <strong>com</strong>petence to unconscious<br />
<strong>com</strong>petence. The majority of our students rated <strong>the</strong>mselves<br />
in between <strong>the</strong> stages of conscious in<strong>com</strong>petence to<br />
conscious <strong>com</strong>petence. The Purnell Model focuses on<br />
<strong>the</strong> 12 Domains of Culture: heritage, <strong>com</strong>munication,<br />
family roles, work<strong>for</strong>ce issues, bio-cultural ecology, highrisk<br />
behaviors, nutrition, pregnancy/childbearing, death<br />
rituals, spirituality, health care practices and role of health<br />
practitioners. Students did a self-assessment, an interview<br />
of a culturally diverse person, and analyzed two o<strong>the</strong>r<br />
cultures of <strong>the</strong>ir choice based on <strong>the</strong>se 12 domains. This<br />
model was an effective framework <strong>for</strong> assessment and<br />
intervention. (Purnell & Paulanka, 2008)<br />
Leininger’s Cultural Care Diversity and Universality<br />
Theory is <strong>the</strong> primary <strong>the</strong>ory we used to integrate<br />
cultural care diversity and holistic care into practice.<br />
The conceptual framework at BRCN is Whole Person<br />
Nursing, which includes <strong>the</strong> client’s beliefs, values,<br />
family, and <strong>com</strong>munity into <strong>the</strong>ir care and is congruent<br />
with Leininger’s Theory. Parts of Campinha-Bacote’s<br />
Model: Process of Cultural Competence in <strong>the</strong> Delivery<br />
of Healthcare Services were also included. Cultural<br />
awareness, knowledge, skill, encounter and desire are<br />
essential to developing cultural <strong>com</strong>petence (2002).<br />
Immersion experiences in ano<strong>the</strong>r cultural,<br />
socioeconomic, urban, rural or o<strong>the</strong>r type of group are<br />
identified as good learning experiences <strong>for</strong> students<br />
in developing cultural <strong>com</strong>petence. These experiences<br />
are often developed as a senior elective or as part of a<br />
<strong>com</strong>munity health course. Students must have significant<br />
cultural awareness and knowledge in order to benefit most<br />
Cultural Competence continued on page 15
The Illinois Nurse October 2009 Page 15<br />
Cultural Competence continued from page 14 if we are to end existing health disparities and create a<br />
from <strong>the</strong>se experiences.<br />
more socially just healthcare environment and society <strong>for</strong><br />
all.”<br />
Issues in Teaching Cultural Competence<br />
One of <strong>the</strong> biggest issues in teaching cultural<br />
<strong>com</strong>petence is whe<strong>the</strong>r to integrate <strong>the</strong> content or teach<br />
a separate course. At BRCN, we developed a separate<br />
course, because we believed <strong>the</strong>re was not enough attention<br />
being given to students learning cultural <strong>com</strong>petence due<br />
to lack of knowledge among <strong>the</strong> faculty. After teaching it<br />
this way <strong>for</strong> one year and exploring many o<strong>the</strong>r options,<br />
we will integrate <strong>the</strong> content into all courses, and provide<br />
more education and resources <strong>for</strong> <strong>the</strong> faculty. It will be<br />
essential to maintain <strong>the</strong> content and faculty development<br />
and support over time.<br />
Ano<strong>the</strong>r key issue, is what to teach—content or<br />
process or both. We will focus on teaching both. Content<br />
on different cultural beliefs, values, and lifestyles is<br />
important but is not adequate on its own. This tends to<br />
lead to stereotyping clients and lack of an individualized<br />
approach. The assessment process is essential to learn<br />
<strong>the</strong> client’s story and goals and what’s important to <strong>the</strong>m<br />
in order to intervene appropriately. Canales and Bowers<br />
(2001) suggest removing <strong>the</strong> artificial separation between<br />
<strong>com</strong>petent and culturally <strong>com</strong>petent nursing practice.<br />
Culturally <strong>com</strong>petent care is integral to <strong>com</strong>petent<br />
care. Their research proposed that <strong>com</strong>petent nurses<br />
“conceptualize <strong>the</strong> provision of <strong>com</strong>petent care to all<br />
persons who are perceived as different, ra<strong>the</strong>r than<br />
focusing only on those who are perceived as ‘culturally’<br />
different.” This fits perfectly with <strong>the</strong> BRCN Whole Person<br />
Nursing framework.<br />
Evaluation is a key issue in determining graduates’<br />
<strong>com</strong>petence in providing culturally <strong>com</strong>petent care.<br />
How do we know that graduates have achieved cultural<br />
<strong>com</strong>petence? What is <strong>the</strong> best method of evaluation? Is<br />
cultural <strong>com</strong>petence an endpoint or an ever-evolving<br />
process? There are many self-assessment tools available—<br />
but do <strong>the</strong>se truly evaluate cultural <strong>com</strong>petence? The<br />
American Academy of Nursing’s (AAN) Expert Panel on<br />
Culturally Competent Care developed 10 re<strong>com</strong>mendations<br />
to stimulate <strong>the</strong> development and implementation of<br />
knowledge related to culturally <strong>com</strong>petent care in 1992<br />
(AAN, 1992). The AAN expert panel reiterated <strong>the</strong>se<br />
same re<strong>com</strong>mendations in 2007: “<strong>the</strong> conceptualization,<br />
implementation, and evaluation of cultural <strong>com</strong>petence<br />
remains unclear” (Giger etal., 2007).<br />
Lipson and Desantis (2007) identify facilitators to<br />
successful implementation of teaching cultural <strong>com</strong>petence<br />
as administrative support, faculty <strong>com</strong>mitment and<br />
adequate funding. Inhibitors are described as decrease<br />
in core courses focused on culture, a recipe or laundry<br />
list approach which focuses on cultural characteristics, a<br />
microlevel approach which focuses on individual nursepatient<br />
encounters and neglect of <strong>the</strong> macrolevel factors<br />
which affect health disparities and client health, and <strong>the</strong><br />
geographical context and setting of <strong>the</strong> clinical education.<br />
And finally, Drevdahl, Canales, & Dorcy (2008) suggest<br />
that a focus on cultural <strong>com</strong>petence does not address <strong>the</strong><br />
larger health issues and risks in society. “The causes of<br />
health disparity exist at a much broader social, political<br />
and economic level, and <strong>the</strong>re<strong>for</strong>e require much broader<br />
approaches if <strong>the</strong>y are to be eliminated. We need to engage<br />
in critical thinking, reflective practice, and political action<br />
BRCN Experience<br />
In <strong>the</strong> major curriculum revision of 2007, <strong>the</strong> faculty<br />
questioned whe<strong>the</strong>r cultural <strong>com</strong>petence was really<br />
integrated into <strong>the</strong> BRCN curriculum. Two faculty, <strong>the</strong><br />
author and Carol Ann Moseley, RN, PhD, had studied<br />
education in cultural <strong>com</strong>petence extensively in writing<br />
a HRSA grant application, agreed to develop and teach a<br />
one-hour, online required course <strong>for</strong> seniors. The Purnell<br />
Model and Leininger’s Theory were <strong>the</strong> major threads of<br />
<strong>the</strong> course.<br />
The course outline is: Transcultural Diversity and<br />
Healthcare, Self-Assessment. Course assignments<br />
included: discussion questions each week, pre- and postself-assessments,<br />
interview and <strong>com</strong>parison of two cultures<br />
based on <strong>the</strong> 12 domains. Based on student and faculty<br />
evaluation after <strong>the</strong> first semester, assignments were<br />
simplified, <strong>the</strong> Cultural Competency Nursing Care Webbased<br />
Course (www.omhrc.gov) and case study internet<br />
materials were added to <strong>the</strong> course. Finally, after teaching<br />
this course <strong>for</strong> 2 semesters, based on <strong>the</strong> literature, faculty<br />
decided to drop <strong>the</strong> course and integrate <strong>the</strong> content into<br />
all of <strong>the</strong> nursing courses. The course faculty will serve as<br />
mentors and resources to o<strong>the</strong>r faculty.<br />
References<br />
American Academy of Nursing Expert Panel on Cultural<br />
Competent Nursing Care. (1992). AAN expert panel report:<br />
Culturally <strong>com</strong>petent nursing care. Nursing Outlook, 40(6),<br />
277-283.<br />
American Association of Colleges of Nursing. (2008). Cultural<br />
<strong>com</strong>petency in baccalaureate education. Retrieved August<br />
10, 2008 from http://www.aacn.nche.edu/Education/pdf/<br />
<strong>com</strong>petency.pdf<br />
American Association of Colleges of Nursing. (2008). Toolkit<br />
of resources <strong>for</strong> cultural <strong>com</strong>petency in baccalaureate<br />
education. Retrieved August 10, 2008 from http://www.aacn.<br />
nche.edu/Education/pdf/toolkit.pdf<br />
American <strong>Nurses</strong> Association. (1991). Position Paper: Cultural<br />
Diversity. Washington, DC: <strong>Nurses</strong>Books.<br />
Campinha-Bacote, J. (2002). The process of cultural <strong>com</strong>petence<br />
in <strong>the</strong> delivery of Healthcare services: A culturally <strong>com</strong>petent<br />
model of care. Retrieved October 15, 2008 from http://www.<br />
transculturalcare.net/<br />
Canales, M., & Bowers, B. (2001). Expanding <strong>the</strong><br />
conceptualizations of culturally <strong>com</strong>petent care. Journal of<br />
Advanced Nursing, 36 (1), 102-111.<br />
Drevdahl, D., Canales, M., & Dorcy, K. (2008). Of goldfish tanks<br />
and moonlight tricks: Can cultural <strong>com</strong>petency ameliorate<br />
health disparities? Advances in Nursing Science, 31(1), 13-<br />
27.<br />
Giger, J., Davidhizar, R., Purnell, L. Harden, J., Philips, J., &<br />
Strickland, O. (2007). American Academy of Nursing<br />
Expert Panel Report: developing cultural <strong>com</strong>petence<br />
to eliminate health disparities in ethnic minorities and<br />
o<strong>the</strong>r vulnerable populations. Journal of Transcultural<br />
Competence, 18, 95-102.<br />
Institute of Medicine (IOM). (2001). Crossing <strong>the</strong> quality chasm:<br />
A new health system <strong>for</strong> <strong>the</strong> 21st century. Washington, DC:<br />
National Academy Press.<br />
Institute of Medicine (IOM). (2005). Quality Through<br />
Collaboration: The <strong>Future</strong> of Rural Health Care. Washington<br />
(DC): National Academy Press.<br />
Leininger, M. (2002). Culture care <strong>the</strong>ory: A major contribution<br />
to advance transculture nursing knowledge and practice.<br />
Journal of Transcultural Nursing, 13(3), 189-192.<br />
Lipson, J., & Desantis, L. (2007). Current approaches to<br />
integrating elements of cultural <strong>com</strong>petence in nursing<br />
education. Journal of Transcultural Competence, 18 (1)<br />
10S-20S.<br />
The National Quality Forum. (2008). Endorsing a framework<br />
and preferred practices <strong>for</strong> measuring and reporting<br />
culturally <strong>com</strong>petent care. Washington, DC: NQF.<br />
Purnell, L., & Paulanka, B. (2008). Transcultural health care<br />
(3rd Ed). Philadelphia: F. A. Davis.<br />
Sullivan Commission. (2004). Missing persons: Minorities in <strong>the</strong><br />
health professions. Washington, DC.<br />
US Dept of Health and Human Services—Health resources<br />
and services Administration. (2001). Trans<strong>for</strong>ming <strong>the</strong><br />
face of health professions through cultural and linguistic<br />
<strong>com</strong>petence education: The role of HRSA centers of<br />
excellence. Retrieved August 10, 2008 from http://www.hrsa.<br />
gov/cultural<strong>com</strong>petence/<br />
U.S. Office of Minority Health. (2001). National standards <strong>for</strong><br />
culturally and linguistically appropriate services in health<br />
care. Retrieved December 16, 2006 from http://www.omhrc.<br />
gov/clas/index.htm<br />
Visit our website<br />
www.illinoisnurses.<strong>com</strong><br />
<strong>for</strong> a <strong>com</strong>plete listing of<br />
INA Approved Educational Activities