President's Message student Nurse Political ... - nursingALD.com
President's Message student Nurse Political ... - nursingALD.com
President's Message student Nurse Political ... - nursingALD.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
An Official Publication of the Illinois <strong>Nurse</strong>s Association The Voice of Illinois Nursing for more than 100 Years<br />
Volume 5 • No. 1 December 2008<br />
Pamela Robbins, RN, BSN<br />
In the last few months the<br />
Illinois <strong>Nurse</strong>s Association<br />
(INA) has been focused on<br />
building future growth of the<br />
association and defining its<br />
relationship with the three<br />
national organizations; the<br />
United American <strong>Nurse</strong>s<br />
(UAN), the Center for American<br />
<strong>Nurse</strong>s (CAN) and the<br />
American <strong>Nurse</strong>s Association<br />
(ANA).<br />
Members of our organization<br />
strategized on how the national<br />
ANA House of Delegates June<br />
Pamela Robbins<br />
2008 bylaws amendment, ANA’s discontinuation of the<br />
UAN affiliation agreement and the agreement with the<br />
CAN, would impact INA financially. These issues shaped<br />
March 31st, 2009<br />
SPRINGFIELD—The largest <strong>student</strong> nurse event in<br />
Illinois, Student <strong>Nurse</strong> <strong>Political</strong> Action Day hosted by the<br />
Illinois <strong>Nurse</strong>s Association’s <strong>Political</strong> Action Committee,<br />
is scheduled March 31st, 2009.<br />
Students learn about the legislative process, the<br />
impact legislation has on nursing practice and experience<br />
an exhibit hall put together just for them! Schools can<br />
NEW Continuing Education<br />
this Issue<br />
Page 12<br />
President’s <strong>Message</strong><br />
the proposed amendments for the INA bylaws at the INA<br />
Emergency House of Delegates (HOD) October 2008.<br />
As of July 1, 2008 ANA required INA to pay $134/<br />
member in a bargaining unit, previously discounted when<br />
the UAN was established. With the discontinuance of<br />
the ANA/UAN affiliation agreement, INA was assessed<br />
an increase of over $116,000 dollars annually. The INA<br />
bylaws proposal to develop a “State-Only” membership<br />
addressed the immediate financial impact for our collective<br />
bargaining unit members. The “State-Only” option allows<br />
our collective bargaining unit members to join INA<br />
exclusively. This proposal was supported by the Economic<br />
and General Welfare Commission, and the bylaws passed<br />
unanimously at the HOD by the INA delegates. The INA<br />
collective bargaining nurses will not incur a dues increase<br />
and every “State-Only” collective bargaining unit member<br />
is eligible to purchase ANA membership on an individual<br />
basis.<br />
INA’s Marketing Task Force (MTF) established the<br />
following goals in July of 2007:<br />
<strong>student</strong> <strong>Nurse</strong> <strong>Political</strong> Action Day<br />
participate in a poster contest and march to the capitol<br />
building along with more than a thousand other <strong>student</strong><br />
nurses. This is a chance to see nursing’s future! Registered<br />
faculty will receive handouts to assist <strong>student</strong>s in gaining<br />
the most out of this wonderful educational experience.<br />
Go to www.illinoisnurses.<strong>com</strong> to find more information<br />
and registration information as of January 1st. You can<br />
also call, 312-419-2900 for more information. See you in<br />
Springfield!<br />
Is License Discipline a Dead<br />
End for your Career?<br />
Page 17<br />
• Market INA as the premiere professional<br />
organization for registered nurses in Illinois;<br />
• Restructure INA to meet the needs of nurses in<br />
Illinois;<br />
• Be the preferred provider of collective bargaining<br />
service for registered professional nurses in Illinois;<br />
• Restructure dues based on identified cost of services<br />
to various target groups.<br />
The goals set by this group were key in shaping a new<br />
dues category for nurses not represented by INA for the<br />
purpose of collective bargaining. This issue, and the “state<br />
only” dues, were voted on in the Membership Meeting<br />
immediately following the HOD. INA demonstrated<br />
the cost of dues for the services of both the collective<br />
bargaining member and the non-collective bargaining<br />
member.<br />
In the spirit co-operation and collaboration, INA<br />
continues to work for all its members delivering services<br />
and programs that benefit our members and promotes the<br />
professional practice of nurses. Whether through INA<br />
programs of Economic and General Welfare, Legislation,<br />
Continuing Education, or Practice INA leadership is<br />
<strong>com</strong>mitted to moving the work of our association forward.<br />
INA leadership, administration and staff are dedicated<br />
to the work of our organization, the realization gains and<br />
forward movement as directed by its members. In January,<br />
the Marketing Task Force will reconvene to review our<br />
strategic goals and will again make re<strong>com</strong>mendations to<br />
the INA Board. We invite any INA member interested in<br />
participating to contact INA Executive Director, Susan<br />
Swart at 312-419-2900 x229.<br />
INA will hold its next convention in October 2009.<br />
How can you impact your state nurse’s professional<br />
organization? Involvement! As a member, it is time to<br />
consider running for an INA state office. You are key to<br />
directing the path of nursing practice. If you are not a<br />
member, join INA today at our “state only” rate of $250/<br />
year, plus District dues. If you want to join INA and the<br />
American <strong>Nurse</strong>s Association, the rate is $390 plus<br />
the district dues. The investment of membership is the<br />
beginning to a relationship of professional networking,<br />
access to nursing knowledge, valuable resources and<br />
activation of your legislative voice to name just a few<br />
perks of INA membership. Join us and lead the way for<br />
professional nursing practice in Illinois!<br />
current resident or<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371
Page 2 December 2008 The Illinois <strong>Nurse</strong><br />
Executive Director’s Update<br />
What’s Next<br />
Susan Y. Swart, RN, MS<br />
INA Executive Director<br />
After months of prep work,<br />
numerous meetings and constant<br />
<strong>com</strong>munication with our members,<br />
the Special House of Delegates<br />
is <strong>com</strong>plete. The members came<br />
together on October 20th looked<br />
at the proposals and set the stage<br />
for the next leg of INA’s journey.<br />
Now we must focus on the<br />
future. Throughout 2009, the<br />
staff at INA will be focused on<br />
recruitment and retention of<br />
Susan Swart<br />
members and exemplary customer<br />
service. An active marketing plan is underway centered on<br />
“choice.” You, the nurse, will have a “choice” in your level of<br />
involvement and participation. We want INA to be what you,<br />
the member, need it to be. The “choice” is yours. You can join<br />
and help make the profession of nursing what I know it can<br />
be. We have set our goal and now we must work to empower<br />
every nurse through education, advocacy and legislation.<br />
We also must market the Illinois <strong>Nurse</strong>s Association as<br />
a multipurpose organization that works to protect nursing<br />
education, nursing practice, and the nurse’s work environment.<br />
Our programs are as diverse as our membership but they all<br />
serve one purpose to empower nurses so that we can practice<br />
in the safest way possible for our patients and ourselves.<br />
One thing we must all understand is that the decision to<br />
join is a political one. Not only at your place of employment<br />
but at every level. Nearly everything that a nurse wants or<br />
needs is proscribed by those in Springfield, laws, rules and<br />
policies. Reimbursement, insurance, and even our practice act<br />
is controlled by the decisions made by our legislators.<br />
It is simple. Whether you agree with everything the<br />
Illinois <strong>Nurse</strong>s Association does or not, we have the ear of the<br />
legislature. We are the ones making sure that a nurse is sitting<br />
at the table when decisions regarding healthcare and your<br />
practice are made. Other organizations have nurses working<br />
for them and yes they too sit at the table but we are the only<br />
organization of “registered professional nurses” that sits there<br />
with all of nursing in the back of our minds.<br />
WE are a diverse group, made of many specialties,<br />
organizations, practice environments, problems, ideologies<br />
and philosophies. But we are “one” profession. We should all<br />
be fighting for a safe work environment for the staff nurse,<br />
salaries for educators that are <strong>com</strong>mensurate with their level<br />
of education, laws that allow APNs to practice based on their<br />
education and preparation, state employees need fair wages,<br />
reimbursement in a timely fashion for their work related<br />
expenses and be able to go to work knowing that they will be<br />
allowed to leave at the end of their shift.<br />
We must stop turning our anger and frustration on each<br />
other; we must stop thinking that we do not control our own<br />
destiny because our adversaries are watching and they see<br />
this as weakness. We must strengthen our image and power<br />
by learning to look past the differences. We must agree to<br />
disagree on certain issues and we must never lose sight of<br />
our goals. We have over 140,000 licensed registered nurses<br />
in Illinois. Can you image what we could do if we all came<br />
together to empower this profession we have all worked so<br />
hard to be a part of?<br />
Closing thought: As we look ahead into the next century,<br />
leaders will be those who empower others. – Bill Gates<br />
Il l I n o I s nu r s e s As s o c I A t I o n<br />
President<br />
Pamela Robbins, BSN, RN: pamrobbins@urban<strong>com</strong>.net<br />
First Vice President<br />
Mildred Taylor, BSN, RN: m.taylor.rn@<strong>com</strong>cast.net<br />
Second Vice President<br />
Roosevelt Gallion, M.Ed, BSN, RN: RG2194@aol.<strong>com</strong><br />
Secretary<br />
Lori Anderson, CRNA, RN: react911@aol.<strong>com</strong><br />
Treasurer<br />
Sharon Zandell, RN: sharon.zandel@med.va.gov<br />
Board of Directors:<br />
Rebecca O. Armea, RN: rarmearn@sbcglobal.net<br />
Sandra Fischer, RN: fish23w@yahoo.<strong>com</strong><br />
Queen Gallien-Patterson, RN: qpatterson@aol.<strong>com</strong><br />
Jack Overfelt RN, CCHP: jack.overfelt@insightbb.<strong>com</strong><br />
P. Joan Larsen, RN: pjscrapbook@frontiernet.net<br />
Terri L. Williams RN: sewpro9370@aol.<strong>com</strong><br />
Joyce Bailey RN: jabrn_51@webtv.net<br />
Barbara M. Gaffke, PhD, MSN, CS: gaffke5@ameritech.net<br />
Mary Bortolotti, RN: mandkbort@aol.<strong>com</strong><br />
Mariza Marcili, CNP, RN: macam1444@aol.<strong>com</strong><br />
Karen Kelly, EdD, RN, CNE-BC: kkellys@aol.<strong>com</strong><br />
Pamela J. Para RN, MPH, CPHRM, ARM, FASHRM:<br />
pjpara2001@yahoo.<strong>com</strong><br />
Ruby P. Reese RN PhD<br />
District Presidents<br />
1 Roosevelt Gallion: RG2194@aol.<strong>com</strong><br />
2 Mary Bortolotti: mandkbort@aol.<strong>com</strong><br />
3 Sharon Peterson: speterson@crusaderclinic.org<br />
5 Royanne Shultz: royanneschultz@hotmail.<strong>com</strong><br />
8 Ann O’Sullivan: aosullivan@blessinghospital.<strong>com</strong><br />
9 Terri Williams: sewpro9370@aol.<strong>com</strong><br />
10 Jane Bruker: jkbru@aol.<strong>com</strong><br />
13 Janet Lynch: lynch.janet08@gmail.<strong>com</strong><br />
14 Martha McDonald: Martha.mcdonald@sih.net<br />
15 Vacant<br />
17 Ann Smith: nevann@netscape.<strong>com</strong><br />
18 Vacant<br />
19 Margaret Kraft: margaret.kraft@att.net<br />
20 Cheryl Anema: tccnurse@aol.<strong>com</strong><br />
21 Sandra Webb Booker: stethes@yahoo.<strong>com</strong><br />
E & GW Commission<br />
Sandra D. Robinson, Chair: nursemoney06@yahoo.<strong>com</strong><br />
Linda Briggs: lindasbriggs@yahoo.<strong>com</strong><br />
Rosemary Kelly: ranajarkelly@yahoo.<strong>com</strong><br />
Virginia Rockett: momynator@yahoo.<strong>com</strong><br />
Judith K. Hopkins: Sicu40@aol.<strong>com</strong><br />
Teresa Pickle: gaptip@sbcglobal.net<br />
Greg Shouse: gashouse1@mchsi.<strong>com</strong><br />
Christine H. Szkarlat: Christine.Szkarlat@va.gov<br />
Joseph Williams: Sangamojoe@aol.<strong>com</strong><br />
Local Unit Chairpersons<br />
City of Chicago: Donna Feaster (D21)<br />
RC-23 State of Illinois: Lee Goehl<br />
Co-Chair Bill Schubert<br />
St. Joseph: Joan Nichols (D02)<br />
Union Health Services: Stephanie Daniel (D20)<br />
University of Chicago: Angela Willis (D20)<br />
University of Illinois: Marcia Hymon (D20), Leo Sherman<br />
VA Hines: Mary Ellen Duke (D19)<br />
Christine Szkarlat (D9)<br />
VA North Chicago: Thelma Fuentes<br />
VA Westside: Murrie Davis (D01)
The Illinois <strong>Nurse</strong> December 2008 Page 3<br />
Il l I n o I s nu r s e s As s o c I A t I o n<br />
Illinois <strong>Nurse</strong>s Association/<br />
INA Foundation<br />
105 W. Adams, Suite 2101 911 S. Second Street<br />
Chicago, IL 60603 Springfield, IL 62704<br />
312/419-2900 217/523-0783<br />
Fax: 312/419-2920 Fax: 217/523-0838<br />
www.illinoisnurses.<strong>com</strong><br />
Executive Director:<br />
Susan Swart, RN, MS: Ext. 229, sswart@illinoisnurses.<strong>com</strong><br />
Chief Operating Officer:<br />
Rick Frankhart: Ext. 233 rfrankhart@illinoisnurses.<strong>com</strong><br />
Chief Financial Officer:<br />
Rick Roche: Ext. 230, rroche@illinoisnurses.<strong>com</strong><br />
Program Director, EGW:<br />
Elwood R. Thompson: Ext. 228, ethompson@illinoisnurses.<strong>com</strong><br />
Director of Nursing Practice:<br />
Sharon Canariato, MSN, MBA, RN, Ext. 235<br />
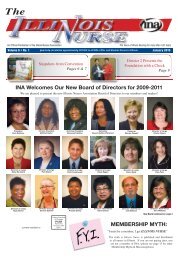
Board of Directors, Illinois <strong>Nurse</strong>s Association<br />
scanariato@illinoisnurses.<strong>com</strong><br />
Director of Membership/Marketing:<br />
Amy Taylor, RN: Ext. 232 ataylor@illinoisnurses.<strong>com</strong><br />
Associate Director, Continuing Education:<br />
Kemi Ani, Ext. 240 kani@illinoisnurses.<strong>com</strong><br />
E&GW Staff Attorney:<br />
Alice Johnson, Ext. 239, ajohnson@illinoisnurses.<strong>com</strong><br />
E&GW Staff Specialists:<br />
Rick Lezu, 217-523-0783 rlezu@illinoisnurses.<strong>com</strong><br />
Remzi Jaos, Ext. 245 rjaos@illinoisnurses.<strong>com</strong><br />
Pam Brunton, Ext. 224 pbrunton@illinoisnurses.<strong>com</strong><br />
Abass Wane, Ext. 249 awane@illinoisnurses.<strong>com</strong><br />
E&GW Coordinator:<br />
Rhonda Perkins, Ext. 223 rperkins@illinoisnurses.<strong>com</strong><br />
Coordinator, Springfield<br />
Staci Moore, 217-523-0783 staci@illinoisnurses.<strong>com</strong><br />
Staff Accountant:<br />
Toni Fox, Ext. 243 tfox@illinoisnurses.<strong>com</strong><br />
Administrative Assistant:<br />
Brenda Richardson, Ext. 248 brichardson@illinoisnurses.<strong>com</strong><br />
Melinda Sweeney, Ext. 222 msweeney@illinoisnurses.<strong>com</strong><br />
Receptionist:<br />
Natasha Angel: Ext. 200<br />
Editorial Committee<br />
Alma Labunski, EdD, MS, RN, Chair<br />
Margaret Kraft, RN, PhD<br />
Linda Olson, PhD, RN<br />
Lisa Anderson Shaw Dr. PH, MA, MSN<br />
Mary Shoemaker, PhD, BS, MS, RN<br />
The Illinois <strong>Nurse</strong> is published quarterly (4 issues yearly) by the<br />
Illinois <strong>Nurse</strong>s Association, 105 W. Adams, Suite 2101, Chicago,<br />
IL 60603.<br />
Advertising Rates Contact—Arthur L. Davis Agency, 517<br />
Washington St., P.O. Box 216, Cedar Falls, Iowa 50613, (319) 277-<br />
2414. INA and the Arthur L. Davis Agency reserve the right to<br />
reject any advertisement. Responsibility for errors in advertising<br />
is limited to corrections in the next issue or refund of price of<br />
advertisement.<br />
Acceptance of advertising does not imply endorsement or approval<br />
by the Illinois <strong>Nurse</strong>s Association of products advertised, the<br />
advertisers, or the claims made. Rejection of an advertisement<br />
does not imply a product offered for advertising is without merit,<br />
or that the manufacturer lacks integrity, or that this association<br />
disapproves of the product or its use. INA and the Arthur L. Davis<br />
Publishing Agency shall not be held liable for any consequences<br />
resulting from purchase or use of an advertiser’s product. Articles<br />
appearing in this publication express the opinions of the authors;<br />
they do not necessarily reflect views of the staff, board, or<br />
membership of INA or those of the national or local associations.<br />
2008 Power of Nursing Leadership<br />
Event a Success!<br />
The 2008 Power of Nursing Leadership Event was held<br />
on Friday, October 24th and hosted over 600 attendees<br />
as well as over twenty exhibitors! INA President, Pamela<br />
Robbins was identified as one of the Pinnacle Leaders.<br />
Congratulations to Pam and all the leaders identified at<br />
this wonderful event!<br />
Please visit our website http://web.nursing.uic.edu/<br />
pnle/index.html for 2008 event photos http://web.nursing.<br />
uic.edu/PNLE/PNLE_08_slideshow/, the 11th Illinois<br />
Outstanding Nursing Leader profile http://web.nursing.uic.<br />
edu/pnle/Awards08/<strong>Nurse</strong>_Leader/<strong>Nurse</strong>_Leader.html.<br />
Pictured: Left Top: Eileen French, Donna Thompson, Paula Dillon,<br />
Alex Guyan, Patricia Altman, Paula Goff, Ann Podoba,<br />
Virginia “Ginger” Morse, Nancy Burke, Ann Nowak,<br />
Roseanne Niese, Sue Hughes<br />
Left Bottom: Pam Robbins, Karen Stratton, unidentified person,<br />
Dean Joan Shaver, Susan Okuno-Jones, Diana Wilkie, Cindy Rentsch<br />
Not pictured: Roberta Berg, Karen Kavanaugh, Beverly McElmurry,<br />
Phyliss Kluch
Page 4 December 2008 The Illinois <strong>Nurse</strong><br />
Mildred Taylor BSN, RN Chairperson<br />
INA Government Relations Committee<br />
Legislation is pending to<br />
increase the role of the Certified<br />
Nursing Assistant (CNA) to<br />
create a CNA II position. The<br />
Illinois <strong>Nurse</strong>s Association<br />
(INA) Government Relations<br />
Committee is currently looking<br />
at the legislation creating a CNA<br />
II position with much hesitation.<br />
The additional responsibilities<br />
would echo those of a Licensed<br />
Practical <strong>Nurse</strong> (LPN) including<br />
medication administration.<br />
Mildred Taylor<br />
It is a direct violation of the <strong>Nurse</strong> Practice Act to allow<br />
unlicensed workers to administer medication, or for<br />
a Registered <strong>Nurse</strong> (RN) to delegate this act to the<br />
CNA. Illinois already has a program called the Illinois<br />
INA Government Relations Report<br />
Safe Staffing and Increased CNA Roles Lead<br />
<strong>Nurse</strong> Legislation 2009<br />
Step Up and Protect Your Profession and Patient Care<br />
Articulation Initiative that provides a CNA the opportunity<br />
to advance their career by be<strong>com</strong>ing an LPN and then a<br />
RN. The Government Relations Committee is calling for<br />
grassroots action to defeat CNA II legislation in 2009. Join<br />
the INA Grassroots Team by joining your professional<br />
association today.<br />
Ask yourself what you consider to be safe staffing. Is<br />
your facility utilizing the <strong>Nurse</strong> Staffing by Patient Acuity<br />
law passed last year? The Illinois <strong>Nurse</strong>s Association<br />
crafted this innovative legislation which includes a<br />
staffing plan utilizing the input of bedside nurses in<br />
staffing decisions. It is time to see how the staffing bill<br />
works for you and your facility. The law re<strong>com</strong>mends that<br />
staffing plans take into account patient acuity, nursing<br />
expertise and skill mix and unit specific circumstances.<br />
Safe staffing refers to having the appropriate number of<br />
nurses and the correct mix of nursing experience on every<br />
patient care unit. The patient acuity law empowers direct<br />
care nurses to have a decision-making role in the creation<br />
of safe staffing plans within their work settings. If your<br />
hospital is not following the law, you can report this to the<br />
Illinois Department of Public Health (IDPH). INA will be<br />
following the development of these staffing protocols in<br />
up<strong>com</strong>ing articles in the Illinois <strong>Nurse</strong>. We want to know<br />
how your facility is making safe staffing a priority, and<br />
your personal experience as a bedside nurse. Share your<br />
stories with us at the email addresses below.<br />
The INA Government Relations Committee’s strategic<br />
plan for the 2009 legislative session will focus on several<br />
key issues. These include mandatory overtime in state<br />
facilities and safe patient handling. <strong>Nurse</strong>s working in state<br />
facilities remain mandated for extensive overtime in unsafe<br />
staffing conditions. We need to continue fighting for each<br />
other. Protecting ourselves, our patients and our fellow<br />
nurses is the responsibility every nurse in Illinois.<br />
In closing, we often define ourselves as being a nurse.<br />
Did you know that it is against the law to refer to yourself<br />
as a nurse if you are not registered and licensed as one?<br />
INA has successfully lobbied to protect our title, it is<br />
what we have worked hard to achieve and preserve. Stand<br />
along side the nurses of Illinois to lobby to protect this<br />
title. WE are the nurses of Illinois. We are bringing this<br />
re<strong>com</strong>mendation to the federal level through the American<br />
<strong>Nurse</strong>s Association (ANA). We continue to stand up for<br />
nursing in Illinois, and we invite you to join us.<br />
For more information on legislative issues that can<br />
potentially effect our patient care and our profession,<br />
please contact:<br />
Susan Swart RN, MS<br />
INA Executive Director<br />
SSwart@illinoisnurses.<strong>com</strong><br />
Mildred Taylor BSN, RN<br />
Government Relations Chairperson<br />
Taylor.mildred@att.net<br />
M.Taylor.rn@<strong>com</strong>cast.net<br />
Sharon Canariato MBA, RN<br />
Director of Nursing Practice<br />
SCanariato@illinoisnurses.<strong>com</strong>
The Illinois <strong>Nurse</strong> December 2008 Page 5<br />
The Center for American <strong>Nurse</strong>s Calls For an End<br />
to Lateral Violence and Bullying in Nursing Work<br />
Environments<br />
New position statement offers information and re<strong>com</strong>mended<br />
strategies<br />
Silver Spring, MD.—February 27, 2008—Research has<br />
consistently shown an unacceptable level of violence in the<br />
workplaces of registered nurses (RNs). The sources of this<br />
violence include patients and their significant others, physicians,<br />
other healthcare personnel, and—perhaps most disconcerting—<br />
other RNs. Lateral violence and bullying specifically have<br />
been extensively reported and documented among healthcare<br />
professionals, with serious negative out<strong>com</strong>es for registered<br />
nurses, their patients, and healthcare employers.<br />
It is the position of the Center for American <strong>Nurse</strong>s that<br />
there is no place in a professional practice environment<br />
for lateral violence and bullying among nurses or between<br />
healthcare professionals. All healthcare organizations should<br />
implement a zero tolerance policy related to disruptive<br />
behavior, including a professional code of conduct and<br />
educational and behavioral interventions to assist nurses in<br />
addressing disruptive behavior.<br />
Center for American <strong>Nurse</strong>s Addresses Retirement Needs<br />
of <strong>Nurse</strong>s<br />
Silver Spring, MD.—August 22, 2008—Sixty percent<br />
of nurses aged 45 to 60 say they have done little to prepare<br />
themselves financially for retirement. Moreover, nurses express<br />
concern that government programs such as Social Security,<br />
Medicare, and Medicaid may be cut back when they need them.<br />
As a result, the Center for American <strong>Nurse</strong>s in partnership with<br />
the Women’s Institute for a Secure Retirement (WISER) are<br />
addressing the retirement planning needs of nurses.<br />
“The nursing profession is a rapidly aging workforce that is<br />
underserved in investor and financial education,” says WISER<br />
President M. Cindy Hounsell.”<br />
The Center and WISER, with a grant from the FINRA<br />
Investor Education Foundation, have established a major financial<br />
education initiative aimed at strengthening the financial security of<br />
our nation’s nurses. The goals of this initiative, named the <strong>Nurse</strong>s’<br />
Investor Education Project, are to:<br />
1) Gain an understanding of nurses’ baseline awareness of<br />
long-term investing and financial planning,<br />
2) Create sustainable and replicable investment education<br />
products and activities, and<br />
3) Improve nurses’ savings behavior and investment planning.<br />
The Center for American <strong>Nurse</strong>s invites you to visit their<br />
newly redesigned website, www.centerforamericannurses.org,<br />
putting the workforce advocacy tools and information you need<br />
right at your fingertips. The new website is packed with news,<br />
user friendly resources, and the Center’s new online journal<br />
NURSES FIRST, the only online journal focused on workforce<br />
advocacy issues.<br />
The Center for American <strong>Nurse</strong>s is pleased to announce its<br />
new legal webinar series. These cutting edge legal webinars will<br />
be presented by expert nurse attorneys with years of legal and<br />
courtroom experience and expertise in nursing law and issues.<br />
The first series focuses on the nursing aspects of civil,<br />
criminal, administrative, and employment law. During these<br />
75 minute sessions experts will review due process in licensure<br />
disciplinary investigations and provide you with strategies to<br />
protect yourself.<br />
Series 1—Centered on the <strong>Nurse</strong>:<br />
January 21, 2009—Nursing Rights & Responsibilities in the<br />
Workplace<br />
Edie Brous, RN, MS, MPH, JD<br />
Each live webinar will be held from 7:00 pm to 8:15 pm EST.<br />
Pricing:<br />
Center Members $49.95 per session<br />
Non-Members $69.95 per session<br />
Register for the entire Centered on the <strong>Nurse</strong> Series:<br />
Center Members $175.00<br />
Non Members $225.00<br />
Register at www.centerforamericannurses.org<br />
Each legal webinar will provide 60 minutes of lecture and<br />
15 minutes of questions and answers for a total of 75 minutes.<br />
The Center for American <strong>Nurse</strong>s is co-providing this activity<br />
with Anthony J. Jannetti, Inc. (AJJ). Anthony J. Jannetti is<br />
accredited as a provider of nursing continuing education by<br />
the American <strong>Nurse</strong>s Credentialing Center’s Commission on<br />
Accreditation.<br />
Questions: call 1-800-685-4076 or email laurel.blaydes@<br />
centerforamericannurses.org<br />
Updates From Our National Affiliates<br />
The American <strong>Nurse</strong>s Association Works Toward<br />
A Consensus Agreement On A Core Set Of<br />
National Priorities In Health Care<br />
SILVER SPRING, MD–The American <strong>Nurse</strong>s<br />
Association (ANA), the National Quality Forum (NQF),<br />
along with representatives of 26 other major national<br />
health care organizations joined forces today by publicly<br />
releasing its report, Aligning Our Efforts to Transform<br />
America’s Healthcare Goals designed to set national<br />
priorities and goals to achieve a high-performing, health<br />
care system delivering quality care to all.<br />
ANA, ANA/California, California <strong>Nurse</strong>s<br />
Association And The California School <strong>Nurse</strong>s<br />
Organization To Argue In Support Of Enforcing<br />
The California Nursing Practice Act In<br />
Aeministering Insulin To Students With Diabetes<br />
In California’s K-12 Public Schools<br />
SILVER SPRING, MD—The American <strong>Nurse</strong>s<br />
Association and its state affiliate, ANA/California, will<br />
present oral arguments on November 14, 2008 before the<br />
Honorable Lloyd G. Connelly at 9:00 a.m. in Sacramento,<br />
CA, in a case filed in the Superior Court of the State of<br />
California in 2007 against the Superintendent of Public<br />
Instruction and the California Department of Education<br />
to remedy violations of law arising from its directive,<br />
published in the form of a “Legal Advisory,” that permits<br />
unlicensed volunteer school employees to administer<br />
insulin to <strong>student</strong>s with diabetes.<br />
American <strong>Nurse</strong>s Association Mourns The Passing<br />
Of ANA Hall Of Fame Inductee And Hospice<br />
Care Pioneer, Florence Wald<br />
SILVER SPRING, MD—It is with deep sadness that<br />
we inform you of the passing of our venerable colleague,<br />
Florence Wald, RN, MSN, FAAN. Florence Wald passed<br />
away at her home in Connecticut on Saturday November,<br />
8th at the age of 91. She was internationally recognized as<br />
a pioneer in the field of hospice care.<br />
Wald studied hospice care in London. Upon her return<br />
to the states, she developed a hospice model that provides<br />
holistic and humanistic care for the dying person and<br />
requires appropriate understanding of the concepts of<br />
death and dying among nurses giving care in the hospice<br />
environment. Since that time, her exemplary work with the<br />
dying has influenced the further development of hospice<br />
care throughout the nation.<br />
Our deepest sympathies are with the Wald family, and<br />
our hope is that they derive some <strong>com</strong>fort from the great<br />
affection and respect felt for their beloved family member<br />
by the nursing <strong>com</strong>munity.<br />
ANA Wel<strong>com</strong>es New Administration, New<br />
Congress<br />
The American <strong>Nurse</strong>s Association (ANA) is celebrating<br />
a number of successes in the 2008 election. Many<br />
advocates of health care and nursing priorities were<br />
elected to the U.S. Congress on Tuesday. Although there<br />
is one race still to be decided, 88 percent of the candidates<br />
endorsed by ANA’s <strong>Political</strong> Action Committee (PAC)<br />
board will be serving in the 111th Congress.<br />
Congress passes Mental Health Parity<br />
Legislation included in Bailout Package<br />
Silver Spring, MD, October 3, 2008–The American<br />
<strong>Nurse</strong>s Association (ANA) is pleased to announce the<br />
House and Senate have approved the Mental Health Parity<br />
and Addiction Legislation, known as the Paul Wellstone<br />
and Pete Domenici Mental Health and Equity Act of 2008.<br />
This legislation would require health plans offering mental<br />
health coverage to provide the same benefits for mental<br />
illness as they do for other medical conditions. ANA has<br />
been a strong advocate for mental health parity legislation<br />
that makes a real difference in the lives of those facing<br />
mental illness.<br />
The legislation was part of the 700 billion dollar<br />
financial market rescue package passed by the Senate<br />
by a vote of 74-25. The House voted 263-171 to pass the<br />
measure which the President has signed into law.<br />
ANA’s Longtime CEO Linda J. Stierle, MSN, RN,<br />
NEA-BC, Announces Her Retirement from Full-<br />
Time Employment<br />
SILVER SPRING, MD—After a long, ac<strong>com</strong>plished<br />
tenure of more than eight years as Chief Executive Officer<br />
at the American <strong>Nurse</strong>s Association (ANA), The Honorable<br />
Linda J. Stierle, MSN, RN, NEA-BC, is announcing her<br />
retirement. Since April 1, 2000 Stierle has served in this<br />
top role developing and implementing programs designed<br />
to meet the vision and goals of the association and leading<br />
and managing the association’s national headquarters, its<br />
operations and its staff of nearly 200 individuals. Stierle<br />
also serves as CEO of the American <strong>Nurse</strong>s Foundation.<br />
The American <strong>Nurse</strong>s Association Launches New<br />
And Improved Web Site For <strong>Nurse</strong>s<br />
Site features improved usability and<br />
navigational elements<br />
SILVER SPRING, MD–The American <strong>Nurse</strong>s<br />
Association (ANA) has launched a re-designed Web<br />
site, Gero<strong>Nurse</strong>Online.org that is designed to serve as<br />
a <strong>com</strong>prehensive, rich resource for nurses and the public<br />
they serve.<br />
“ANA’s Gero<strong>Nurse</strong>Online.org Web site provides nurses<br />
with resources regarding clinical information, education<br />
and career certification instrumental in providing care<br />
for older adults, regardless of specialty. We encourage<br />
you to explore the Web site and stay informed of trends<br />
and developments in geriatric care,” said ANA President<br />
Rebecca M. Patton, MSN, RN, CNOR.<br />
The Gero<strong>Nurse</strong>Online.org’s new features include:<br />
• Career opportunities in geriatric nursing;<br />
• Links to 55 specialty nursing associations’ clinical<br />
offerings in geriatric care and geriatric websites;<br />
• Resource organizations and related resource materials;<br />
• Hospital <strong>com</strong>petencies for caring for older adults for<br />
use in nurse orientation and evaluation;<br />
• Online courses to prepare for ANCC gerontological<br />
certification; and<br />
• ANA advocacy work on behalf of geriatric nurses.<br />
For detailed information on any of these announcements<br />
please visit the ANA website www.nursingworld.org for<br />
the <strong>com</strong>plete press release.<br />
Labor Leader Institute Features RNWT Director<br />
In a plenary address, participants at this year’s Labor<br />
Leader Institute in Chicago heard RNs Working Together<br />
(RNWT) Executive Director Steve Francy describe the<br />
value of nurses from different unions <strong>com</strong>ing together<br />
to speak with a <strong>com</strong>mon voice on shared goals. RNWT<br />
is an AFL-CIO coalition of 10 unions, including UAN,<br />
representing about 200,000 RNs nationwide. The coalition<br />
has been active on issues such as safe RN-patient ratios and<br />
passage of H.R. 2123, the real safe staffing bill, sponsoring<br />
a Capitol Hill briefing on the measure in July. “There’s<br />
recognition that there is something to be gained by <strong>com</strong>ing<br />
together,” said Francy. “When the leaders of RNWT <strong>com</strong>e<br />
together, they are representing working, union nurses—not<br />
nurse executives, or managers, or educators.”<br />
UAN, MNA Pressure Stops Bad RN<br />
Immigration Bill<br />
In response to lobbying from UAN nurses and Michigan<br />
nurses in particular, Rep. John Conyers (D-MI) pulled a<br />
bill from the House Judiciary Committee’s calendar that<br />
would have expanded the availability of nurse visas without<br />
protecting nurses in the U.S. or preventing other countries<br />
from losing badly needed health care professionals. It<br />
is likely that the American Hospital Association and<br />
other nurse management groups will seek to reintroduce<br />
the bill in 2009. For more on UAN’s position on the<br />
utilization of foreign nurses as a staffing solution, please<br />
see the National Labor Assembly’s 2001 resolution: www.<br />
uannurse.org/who/resolution/2001/06.html
Page 6 December 2008 The Illinois <strong>Nurse</strong><br />
Sharon Canariato, Director of Nursing Practice<br />
As I am sitting down to<br />
write this article, we are in the<br />
midst of the 2008 presidential<br />
campaign. A major issue in this<br />
election is healthcare. According<br />
to the US Census Bureau (2007),<br />
there are 45.7 million citizens<br />
without health insurance. The<br />
current health care system in<br />
our country is struggling due to<br />
rising health care costs. To insure<br />
health care coverage is extended<br />
Sharon Canariato<br />
to all eligible residents of the<br />
United States may <strong>com</strong>plicate<br />
an already strained environment. According to the Institutes<br />
of Medicine (2004), we are the only wealthy, industrialized<br />
nation that does not provide a universal health care system.<br />
Universal healthcare is an extensive concept and would<br />
be a huge undertaking as it can be implemented in many<br />
different manners. The exact mechanism to obtain health<br />
care coverage for everyone can be very controversial.<br />
I believe that we as nurses inherently feel that no one<br />
should go without health care. We see the consequences<br />
of those patients who do not receive health care or delay<br />
seeking treatment. Illinois <strong>Nurse</strong>s Association has always<br />
supported the concept of Universal Health Care. Illinois<br />
<strong>Nurse</strong>s Association (1996) developed a position statement<br />
which supports the concept of universal access to healthcare<br />
across the lifespan by eliminating barriers to care and<br />
discrimination in service delivery. INA <strong>com</strong>mits to health<br />
care that is <strong>com</strong>prehensive and is culturally sensitive<br />
incorporating prevention focused primary care as a<br />
foundation for high quality, cost effective health care.<br />
Recently, Illinois <strong>Nurse</strong>s Association has been attending<br />
meetings and workshops with AFL-CIO. They have a<br />
campaign entitled, “Health Care for America.” Their goal<br />
is to obtain high-quality health care for everyone. While<br />
they do not wish to mandate that all citizens buy a health<br />
insurance policy, they feel that meaningful health care<br />
reform is based on several key concepts. The AFL-CIO<br />
Practice Corner<br />
Executive Council Statement (2007) lists these concepts<br />
which should be incorporated into any health care reform:<br />
• Universal Coverage—states that everyone should have<br />
healthcare coverage without exclusion or penalties.<br />
The government must pay a role in regulating,<br />
financing and providing health care.<br />
• Comprehensive, Affordable Coverage—means that<br />
coverage should be reasonably priced and employers<br />
have a role in supplementing that coverage.<br />
• Choice of Providers—indicates that individuals should<br />
retain the ability to select their own doctors and health<br />
care providers.<br />
• Financing through Shared Responsibility—states that<br />
the risks would be shared. Everyone would have the<br />
responsibility for contributing to the system. Every<br />
employer must play their part in ensuring coverage.<br />
• Effective Cost Control—means a mechanism must be<br />
in place for controlling costs. Systems and technology<br />
investments should be made to reduce errors and<br />
costs.<br />
• Do No Harm—requires that until healthcare is<br />
reformed, any existing coverage should not be<br />
undermined and put people at risk of unmet health<br />
care needs.<br />
(See http://www.aflcio.org/issues/healthcare for further<br />
information on their plan)<br />
When this column is finally released in print, the next<br />
president of the United States will have been elected. This<br />
president will be challenged with the task of improving<br />
health care in America. It will be interesting to see the<br />
progression of this exigent situation.<br />
References<br />
AFL-CIO. (2007, March). Executive Council Statement. Las<br />
Vegas, NV: Author.<br />
Institute of Medicine at the National Academies of Science.<br />
(2004, January). Insuring America’s Health: Principles and<br />
Re<strong>com</strong>mendations. Washington, DC: Author.<br />
Illinois <strong>Nurse</strong>s Association. (1996, August). Position Statement<br />
on Health Care. Chicago, IL: Author.<br />
US Census Bureau. In<strong>com</strong>e, Poverty and Health Insurance<br />
Coverage in the United States: 2007. Retrieved September 23,<br />
2008, from U.S. Census Bureau Web Site: http://www.census.gov/<br />
prod/2008pubs/p60-235.pdf<br />
Northern Illinois University’s use of the 2007-2008<br />
IBHE Nursing School Expansion Grant: A partnership<br />
with Provena Mercy Medical Center<br />
Brigid Lusk, PhD, RN Chairperson, School of<br />
Nursing, Northern Illinois University<br />
In spring 2007, NIU was one of three Illinois nursing<br />
schools that were each awarded almost $460,000 by the<br />
Illinois Board of Higher Education. The purpose of these<br />
grants was nursing program expansion.<br />
The primary <strong>com</strong>ponent of the NIU proposal was to<br />
expand the number of NIU baccalaureate nursing <strong>student</strong>s<br />
by forty <strong>student</strong>s, or almost 60% of the entering class, using<br />
facilities at Provena Mercy Medical Center in Aurora. All<br />
the theory courses, along with selected clinical courses, were<br />
located on the campus of the medical center. Additionally,<br />
there was an emphasis on the recruitment and retention of<br />
racial and ethnic minority <strong>student</strong>s. After one year, the grant’s<br />
objectives are being successfully addressed and the school has<br />
received $300,000 for the second year of the program.<br />
In Fall 2007, forty NIU <strong>student</strong>s started the sequence of<br />
nursing courses within a newly remodeled and expanded<br />
classroom at Provena Mercy Medical Center. This is an<br />
NEW CAN<br />
WEBSITE!<br />
All INA non-collective bargaining nurses have access<br />
to the newly designed Center for American <strong>Nurse</strong>s<br />
website!<br />
www.centerforamericannurses.org<br />
The mission of the Center is to create healthy work<br />
environments<br />
through advocacy, education and research<br />
(Should you have difficulty accessing the website,<br />
call INA at 312-419-2900)<br />
accelerated program and the <strong>student</strong>s will graduate in May<br />
2009. Twenty-three percent (N=9) of these <strong>student</strong>s were from<br />
racial and ethnic minority backgrounds. Although there has<br />
been a limited amount of attrition, most <strong>student</strong>s who have left<br />
the Aurora program are continuing their nursing coursework<br />
on the main NIU campus. Five senior NIU nursing <strong>student</strong>s<br />
have acted as be peer tutors to the Provena <strong>student</strong>s. Lap top<br />
<strong>com</strong>puters were purchased for half the <strong>student</strong>s—<strong>com</strong>puters<br />
for the remaining <strong>student</strong>s will be purchased through the<br />
second year’s funding. These <strong>com</strong>pensate for lack of <strong>com</strong>puter<br />
laboratory access at the medical center.<br />
Some <strong>com</strong>ments of nursing <strong>student</strong>s at the Provena<br />
site demonstrate their satisfaction with this innovative<br />
hospital-based program: “It's nice to have the program in<br />
an actual hospital...it's a motivation,” “Being in a hospital<br />
setting provides atmosphere that affirms educational choice<br />
constant reminder of goal,” “We are expected to <strong>com</strong>e to<br />
class looking and acting professional in a hospital setting on<br />
first day of school. I think it helps us to see that this is real,<br />
not just another college class.” (Student Surveys, 2007–2008<br />
Academic Year, Millennia Consulting).<br />
Madison County Retired<br />
<strong>Nurse</strong>s...Picking Up Steam<br />
Margaret Miller, RN, MSN, Retired<br />
The Madison County Retired <strong>Nurse</strong>s enjoy a good<br />
lunch, socializing, and a togetherness that only nurses<br />
can identify with at their bimonthly meetings. Proud of<br />
their past careers and services in many different areas of<br />
nursing, the retirees remain interested in current issues of<br />
medicine and nursing. Programs consist of educational<br />
topics such as county emergency preparedness, health<br />
programs for women offered at the local senior center,<br />
the Vile of Life program, MRSA in the <strong>com</strong>munity,<br />
and Alzheimers Disease. The November program was<br />
presented by one of the members, Linda Mahlandt, a<br />
volunteer with the Madison County Health Department, on<br />
telephone crisis management with suicidal people.<br />
The group meets at the Senior Services Plus building<br />
in Alton, on the second Wednesday of odd months. The<br />
meeting place is free of charge and there may be a nominal<br />
charge for food and beverages. Officers are: President,<br />
Starkey Sloan; Secretary, Nita Neunaber; Treasurer, Marie<br />
Klader; and Historian, Ellie Flick. Average attendance for<br />
the year has been 18 and an additional 19 members who<br />
paid their dues in November. New members are always<br />
wel<strong>com</strong>e.<br />
The retired nurses are always looking for opportunities<br />
to be helpful, recently brought canned goods to a local<br />
food pantry and plan to make a monetary donation to<br />
Senior Services in appreciation for use of their meeting<br />
room.<br />
The next meeting of the Madison County Retired<br />
<strong>Nurse</strong>s will be January 14th, 2009, at 11:30 AM at the<br />
Senior Services Plus Building, 2603 N. Rogers Ave,<br />
Alton. The program will be presented by INA District 10<br />
President, Jane Bruker, on her experiences working with an<br />
American Indian Nursing School in New Mexico. Anyone<br />
needing more information may call Starkey Sloan at 618-<br />
474-4009.<br />
Save the Date<br />
INA 2009 Convention<br />
October 15th, 16th & 17th<br />
Go to www.illinoisnurses.<strong>com</strong><br />
for more information.
The Illinois <strong>Nurse</strong> December 2008 Page 7<br />
VA Nursing Academy: Hines Partners with Loyola SON<br />
Sharon Zandell PhD, RN<br />
This summer, Edward Hines, Jr. VA Hospital (Hines)<br />
and the Marcella Niehoff School of Nursing, Loyola<br />
University Chicago (Loyola) received funding from<br />
Veterans Affairs to conduct a VA Nursing Academy,<br />
Enhancing Academic Partnerships Pilot Project. As<br />
one of ten sites throughout the United States, the Hines/<br />
Loyola partnership fosters greater involvement of Hines<br />
nursing staff in Loyola’s undergraduate program, greater<br />
involvement of Loyola faculty in Nursing Service activities<br />
at Hines and a joint Nursing Center for Integrated Mental<br />
Health Nursing (Center). Positions funded through the VA<br />
Nursing Academy will be used to support expansion of<br />
the Loyola 4-year baccalaureate program by matriculating<br />
transfer <strong>student</strong>s with associate degrees (AD) in other<br />
fields or 60 credit hours from a four year college/university<br />
into junior level classes.<br />
Expected out<strong>com</strong>es of the partnership include:<br />
1. Increase in enrollment of up to 40 additional<br />
baccalaureate <strong>student</strong>s each year.<br />
2. Continuation of 93% retention of <strong>student</strong>s during<br />
junior/senior years and increase to 95% NCLEX pass<br />
rate for graduates.<br />
3. Maintenance of a high level of staff, faculty and<br />
<strong>student</strong> satisfaction with clinical learning experiences<br />
at Hines.<br />
4. Employment of at least 10 Loyola graduates at Hines<br />
each year with two year retention of 90%.<br />
5. Increase in staff education at Hines and improvement<br />
in selected patient out<strong>com</strong>es specifically those<br />
related to addressing emotional, mental and<br />
behavioral needs of patients/families.<br />
6. Increase in evidence-based practice initiatives<br />
implemented.<br />
Expansion of Loyola baccalaureate enrollment will<br />
occur by matriculating 20 non-nursing AD graduate or<br />
transfer applicants into junior level coursework during the<br />
spring and fall semesters of each year starting January<br />
2009. This fall, four MSN prepared Hines staff members<br />
began teaching as part-time clinical instructors for Loyola<br />
<strong>student</strong>s as part of their full-time position at Hines.<br />
Additional staff will be involved for the spring semester.<br />
Funding provides salary dollars to hire temporary staff as<br />
their replacement and additional Loyola faculty. Loyola<br />
has provided a 45 content hour course that instructors are<br />
currently in process of <strong>com</strong>pleting. A shorter course will<br />
be provided for Hines BSN prepared staff who will act as<br />
preceptors in the spring-summer semesters.<br />
In September, Hines initiated a UHC/AACN postbaccalaureate<br />
<strong>Nurse</strong> Residency Program with 12 new<br />
graduates in its first cohort. The Center, co-directed<br />
by Dr. Nancy Harris from Hines and Dr. Shirley Butler<br />
from Loyola, has begun planning a joint evidence-based<br />
practice study at Hines. During the spring semester a joint<br />
educational endeavor will involve <strong>student</strong>s in two mental<br />
health clinical rotations partnering with acute care nurses<br />
caring for patients with <strong>com</strong>plex physical conditions who<br />
also have mental health needs. Students will focus on<br />
addressing mental health needs and assist the nurse with<br />
physical care of the patient.<br />
Project Directors<br />
Sharon L. Zandell, PhD, RN Gloria Jacobson, PhD, RN<br />
Chief, Education Service Associate Dean for<br />
Edward Hines Jr. VA Academic Affairs<br />
Hospital Marcella Niehoff School of<br />
(708) 202-5020; Nursing<br />
sharon.zandel@va.gov (773) 508-2917;<br />
gjacobs@luc.edu<br />
Recognize Your Peers<br />
Nominate Today for 2009<br />
Awards<br />
One of the goals set forth<br />
by the Awards Committee for<br />
the 2009 Awards Presentation<br />
is to be able to honor an INA<br />
member for every award.<br />
Please take some time to think<br />
about honoring those members<br />
who have made exceptional<br />
contributions over the last<br />
two years to the growth<br />
and prosperity of INA. For<br />
more information and list of<br />
available awards go to www.<br />
illinoisnurses.<strong>com</strong>.
Page 8 December 2008 The Illinois <strong>Nurse</strong><br />
Mary Maryland Elected<br />
Illinois Division President of<br />
American Cancer Society<br />
The American <strong>Nurse</strong>s<br />
Association (ANA) congratulates<br />
Mary Maryland, PhD, ANP-<br />
BC on being elected President<br />
of the Illinois Division of the<br />
American Cancer Society (ACS).<br />
Maryland is the first nurse, the<br />
second woman, and the fourth<br />
non-MD to serve ACS in this<br />
capacity. Mary Maryland will<br />
serve a two year term, acting<br />
as a spokesperson and helping<br />
to guide the American Cancer<br />
Mary Maryland<br />
Society’s missions of research, education, advocacy and<br />
patient services.<br />
Mary Maryland is a board certified adult nurse<br />
practitioner, who currently serves on the Board of Directors<br />
for ANA and the American <strong>Nurse</strong>s Credentialing Center<br />
and the Board of Trustees for ANA’s <strong>Political</strong> Action<br />
Committee. Her <strong>com</strong>mitment to patient care exemplifies<br />
the excellence of the nursing profession.<br />
INA and ANA applaud The American Cancer Society<br />
for recognizing Mary Maryland’s invaluable skills as a<br />
patient advocate and her dedication to improving health<br />
policy.<br />
ANA Web Site: www.nursingworld.org<br />
IBHE FY 2008 <strong>Nurse</strong> Educator<br />
Fellowship Awards Ceremony<br />
In the Photo (Left to Right) IBHE <strong>Nurse</strong> Educator Fellowship Recipients:<br />
1) Rashidah Abdullah, MS, RN, CNM; 2) Lee Schmidt, PhD, RN; 3) Karen Egenes, EdD, RN<br />
4) Judy Erwin, Executive Director, IBHE; 5) Frank Lyerla, PhD, RN<br />
6) Michele Bromberg, Nursing Act Coordinator; 7) Daniel E. Bluthardt, Director of Professional Regulation<br />
8) Sandra Drozdz Burke, PhD, RN; 9) Mary J. Dyck, PhD, RN, BC, LNHA<br />
10) Linda Duncan, DNP, RN; 11) Connie M. Dennis, PhD, RN<br />
Other recipients not pictured: 12) Kim Amur, PhD, RN<br />
13) Mary Weyer , EdD, RN, APN, CNS; 14) Karen Brandt Baldwin, PhD, RN<br />
15) Beth Nachtsheim Bolick, MS, RN, APN-BC, CPNP-AC, CCRN; 16) Trudy DeWaters, PhD, RN, APN<br />
17) Carla Ferguson, MSN, RN, CNE, CCRN; 18) Paula N. Kagan, PhD, RN<br />
The Illinois Board of Higher Education (IBHE) FY<br />
2008 <strong>Nurse</strong> Educator Fellowship award recipients are<br />
pictured with IBHE Executive Director Judy Erwin<br />
and IDFPR Director of Professional Regulation Daniel<br />
E. Bluthardt. The next fellowship application period is<br />
August, 2009. See ICN website, www.illinois.nursing.gov/<br />
financial.htm, for further information.<br />
The Illinois Board of Higher Education <strong>Nurse</strong> Educator<br />
Fellowship Award is a <strong>com</strong>petitive award, based on<br />
performance, for institutions of higher learning that award<br />
degrees in nursing. This <strong>Nurse</strong> Educator Fellowship was<br />
signed into law on July 11, 2006, by Governor Blagojevich,<br />
to create several new nursing initiatives aimed at<br />
improving the recruitment, training and retention of nurses<br />
in Illinois. This Act includes two new grant programs to be<br />
administered by the Illinois Board of Higher Education–a<br />
<strong>Nurse</strong> Educator Fellowship Program and a Nursing School<br />
Grant Program.<br />
The purpose of the <strong>Nurse</strong> Educator Fellowship Program<br />
is to ensure the retention of well-qualified nursing faculty<br />
at institutions of higher learning that award degrees in<br />
nursing. Awards will be used to supplement the salaries of<br />
the nursing faculty selected for the Fellowship.<br />
Participation in this program is open to Illinois<br />
institutions of higher learning with a nursing program<br />
approved by the Illinois Department of Financial and<br />
Professional Regulation and accredited by the Commission<br />
on Collegiate Nursing Education (CCNE) or the National<br />
League for Nursing Accrediting Commission (NLNAC).<br />
Fellowship nominations are limited to no more than three<br />
full-time nursing faculty members per eligible institution<br />
per award cycle.<br />
To be eligible to receive an award, applicants must meet<br />
the following criteria:<br />
♣ Illinois resident and a minimum of a master’s degree<br />
in nursing;<br />
♣ employed in a full-time nursing faculty position at an<br />
eligible institution;<br />
♣ employed by the nominating institution in a teaching<br />
position preparing registered nurses for a minimum of<br />
12 months;<br />
♣ made significant contributions to the nursing program;<br />
♣ not received an award in the past two years (FY2007<br />
and FY2008); and<br />
♣ nominated by the chief nursing administrator in an<br />
eligible institution.<br />
The Illinois Board of Higher Education (IBHE) FY<br />
2008 <strong>Nurse</strong> Educator Fellowship award application period<br />
is August, 2009. See ICN website, www.illinois.nursing.<br />
gov/financial.htm, for further information.
The Illinois <strong>Nurse</strong> December 2008 Page 9<br />
Nursing Standard Of Care<br />
And The Expert Witness<br />
Attorney Susan A. Wagner, RN<br />
What is meant by the term “standard of care” in medical<br />
negligence cases and in particular to those cases where<br />
negligence has been alleged on the part of the nurse?<br />
In cases involving medical negligence, the plaintiff has<br />
the burden of proving the standard of care against which<br />
the defendant nurse’s conduct is being measured and that<br />
the nurse defendant deviated from the standard of care<br />
resulting in an injury to the plaintiff. Generally, expert<br />
medical testimony is required to establish the standard of<br />
care and any alleged deviation from the standard of care.<br />
The “standard of care” is a phrase familiar to every<br />
nurse and is often used when referencing quality of care<br />
or evaluating care that is being provided to a patient. Most<br />
nurses would likely discuss standard of care in the context<br />
of the high expectations that they might have for the care<br />
that they provide or that is being provided by those that<br />
they supervise.<br />
However, there is an important distinction to be<br />
understood when evaluating the nursing standard of care<br />
for purposes of litigation. The legal standard of care for<br />
nurses in any given situation is a minimum standard of<br />
care and is defined as what a nurse who is reasonably<br />
careful would do under the same or similar circumstances.<br />
How is standard of care determined and can any<br />
medical professional, including a physician, testify as an<br />
expert witness as to what the standard of care is for a nurse<br />
in a particular situation?<br />
In Illinois, in most situations, the answer is “no.” The<br />
Illinois Supreme Court has held that a nurse expert must<br />
testify as to the nursing standard of care in a medical<br />
negligence lawsuit. Sullivan v. Edward Hospital, 209<br />
Ill.2d 100, 806 N.E.2d 645 (2004). The Illinois Supreme<br />
Court has held that a health care expert witness must<br />
be a licensed member of the school of medicine about<br />
which the expert proposes to testify. Dolan v. Galluzzo,<br />
77 Ill.2d 279, 396 N.E.2d 13 (1979). Additionally, the<br />
Illinois Supreme Court has recognized that by enacting the<br />
Nursing and Advanced Practice Nursing Act (225 ILCS<br />
65/5-1 et seq. (West 2000), the legislature has set forth the<br />
unique licensing and regulatory scheme for the nursing<br />
profession, therefore establishing nursing as a unique<br />
school of medicine.<br />
In support of their findings, in the Sullivan case,<br />
the Supreme Court relied in part on the amicus brief<br />
submitted by the American Association of <strong>Nurse</strong> Attorneys<br />
(TAANA). The Court referenced the persuasive argument<br />
of TAANA by stating that “a physician, who is not a nurse,<br />
is no more qualified to offer expert, opinion testimony as<br />
to the standard of care for nurses than a nurse would be<br />
to offer an opinion as to the physician’s standard of care.”<br />
Sullivan, 209 Ill.2d 100, 806 N.E.2d 645 (2004). The<br />
Sullivan case continues to be recognized as the law with<br />
regard to requirements necessary to offer expert testimony<br />
about nursing standards of care in medical negligence<br />
cases.<br />
There is a recognized exception to the Sullivan case<br />
with regard to the rule that nurses act as expert witnesses<br />
to establish the nursing standard of care in a medical<br />
negligence lawsuit. When the allegations of negligence<br />
concern <strong>com</strong>munication between a physician and a nurse<br />
and not a nursing procedure, the Supreme Court has held<br />
that a physician may testify as to the standard of care<br />
required by a nurse in that situation. Wingo v. Rockford<br />
Memorial Hospital, 292 Ill. App.3d 896, 226 Ill. Dec. 939,<br />
686 N.E.2d, 722 (1997).<br />
As an example, consider a situation where a nurse<br />
was injured in a fall at her workplace and was seen in<br />
the emergency room and diagnosed with a fractured<br />
coccyx. At the time that she was examined, she made no<br />
<strong>com</strong>plaints of any type of incontinence. However, several<br />
days after the visit to the emergency room, the nurse was<br />
seen by a chiropractor and, at that time, had <strong>com</strong>plaints of<br />
incontinence. She later filed a lawsuit based on allegations<br />
of negligence on the part of emergency room nursing staff;<br />
and during her deposition in the lawsuit, the nurse said<br />
that she told the emergency room nurse of her <strong>com</strong>plaints<br />
of incontinence. The emergency room nurse testified that<br />
the plaintiff made no <strong>com</strong>plaints about incontinence. An<br />
emergency room physician was brought in to testify as<br />
an expert witness on behalf of the plaintiff regarding the<br />
standard of care of the emergency room nursing staff. The<br />
expert testified that the standard of care for the nurses<br />
in the emergency room required that they <strong>com</strong>municate<br />
and report the patient’s <strong>com</strong>plaints of incontinence to<br />
the emergency room doctor and that if they failed to<br />
<strong>com</strong>municate this information then that was a deviation<br />
from the standard of care. The emergency room physician<br />
is allowed to testify at trial in this matter regarding nursing<br />
standard of care because it fits the exception recognized<br />
by the Courts in Illinois that allows a physician to provide<br />
expert testimony about the nursing standard of care when<br />
the alleged negligence involves <strong>com</strong>munication between<br />
the nurse and physician.<br />
As recently as July of 2008, the Fourth District<br />
Appellate Court in Illinois created an additional exception<br />
to the law that nurses must testify as expert witnesses<br />
to establish the standard of care of nurses in medical<br />
negligence cases. The Appellate Court relied on the<br />
existing exception which allows physicians to testify as to<br />
the nursing standard of care when the alleged negligence<br />
involves <strong>com</strong>munication issues and ruled that it was<br />
appropriate to allow a physician-surgeon to testify as an<br />
expert regarding the standard of care of nurses in their<br />
role as a member of a surgical team conducting a cesarean<br />
section. The Court felt that the pivotal issue in determining<br />
whether a physician may be qualified to testify as an expert<br />
witness regarding the standard of care expected of a nurse<br />
who was a surgical team member depended on the nature<br />
of the interaction between a physician and a nurse as they<br />
provide medical care for the same patient. The Court felt<br />
that the physician could testify regarding the standard of<br />
care of the nurse because the physician and nurse interact<br />
as a team to substantially contemporaneously care for the<br />
same patient. Petryshyn v. Slotky, 2008 Ill. App. Lexis,<br />
752.<br />
This case will likely be appealed to the Supreme Court<br />
which would ultimately rule on this issue and whether they<br />
uphold their previous rulings in Sullivan or allow another<br />
exception to the rule requiring nurses to testify as to the<br />
nursing standard of care in medical negligence cases.
The Illinois <strong>Nurse</strong> December 2008 Page 11<br />
The Philippine <strong>Nurse</strong>s<br />
Association of Illinois<br />
(PNAI), Inc<br />
<strong>Nurse</strong> Excellence Award<br />
The PNAI is accepting nominees for the following<br />
categories:<br />
Clinical Nursing Nursing Administration<br />
Nursing Research <strong>Nurse</strong> Education<br />
<strong>Nurse</strong> Entrepreneurship Community Service<br />
<strong>Nurse</strong> Advocate<br />
Please contact the following for application and<br />
information:<br />
Remedios Dela Cruz, President<br />
815-254--8445<br />
E-mail: remydelacruz@<strong>com</strong>cast.net<br />
Gloria O. Simon, Past President and Advisor<br />
847-414-1557<br />
Galyaodi@yahoo.<strong>com</strong><br />
The final application must be received by January 31,<br />
2009<br />
ISAPN<br />
At the Illinois Society for Advance Practice<br />
<strong>Nurse</strong>s (ISAPN) Conference in October, Aimee<br />
Terhark was sworn in as a First Lieutenant in the<br />
United States Army. Terhark said the moment,<br />
captured in the exhibit hall, was the most<br />
important moment of her life.<br />
Dedicated Illinois Nursing Web Portal Debuts—www.<br />
Modern<strong>Nurse</strong>s.<strong>com</strong><br />
Chicago, IL September 29, 2008—Search Engine Corp<br />
and the Illinois <strong>Nurse</strong>s Association just announced its new<br />
Web search engine and portal project for Illinois <strong>Nurse</strong>s,<br />
Modern<strong>Nurse</strong>s.<strong>com</strong>. This initiative was conceived of by<br />
Search Engine Corp, the global leader in private label<br />
Web search engine development, and the Illinois <strong>Nurse</strong>s<br />
Association.<br />
Modern<strong>Nurse</strong>s.<strong>com</strong> is a search engine and portal<br />
destination for Illinois nursing professionals to use as<br />
their daily online tool to research and access local,<br />
nursing and healthcare information from across the Web.<br />
Modern<strong>Nurse</strong>s.<strong>com</strong> provides local Illinois news, weather,<br />
maps and directions feature plus a variety of tools and<br />
information designed to help nursing and healthcare<br />
professionals.<br />
Rick Frankhart, Chief Operating Officers at Illinois<br />
<strong>Nurse</strong>s Association explains, “Our goal was to develop and<br />
build an online tool for Illinois nurses that will be<strong>com</strong>e<br />
their one-stop-destination to use daily. Modern<strong>Nurse</strong>s.<strong>com</strong><br />
is a great tool plus a vehicle to strengthen relationships<br />
within the Illinois nursing <strong>com</strong>munity.”<br />
For more information on the dedicated Illinois Nursing<br />
Web search engine and portal, contact us at general@<br />
Modern<strong>Nurse</strong>s.<strong>com</strong>. To learn more about Modern<strong>Nurse</strong>s.<br />
<strong>com</strong>, visit the search engine project online at http://www.<br />
Modern<strong>Nurse</strong>s.<strong>com</strong>.<br />
For more information on Search Engine Corp’s new,<br />
dedicated environmental Web search engine, contact<br />
Katrina Boschenko at (505) 660-9916. To learn more about<br />
how the everyday task of Web searching can benefit some<br />
of the nation’s top environmental organizations, visit the<br />
search engine project online at http://www.ClimateGift.<br />
<strong>com</strong>.<br />
CONTACT INFORMATION:<br />
Katrina Boschenko<br />
217 Sena Street, Santa Fe, NM 87505<br />
(505) 660-9916, Katrina@searchenginecorp.<strong>com</strong><br />
http://www.ClimateGift.<strong>com</strong>
Page 12 December 2008 The Illinois <strong>Nurse</strong><br />
The <strong>Nurse</strong>s Role in Documentation<br />
and Reimbursement<br />
by: Sharon Canariato, MSN, MBA, RN<br />
CE OFFERING<br />
1.5 CONTACT HOURS<br />
---------------------------<br />
This offering expires in 2 years:<br />
November, 2010<br />
----------------------------------<br />
The goal of this continuing education<br />
offering is to provide information on documentation<br />
and reimbursement.<br />
The objectives of this article are:<br />
1. List the rules/laws/agencies that regulate health care<br />
billing and the consequence for non-<strong>com</strong>pliance<br />
2. Outline appropriate nursing documentation and its<br />
relationship to hospital reimbursement<br />
3. Identify those scenarios not reimbursed by CMS and<br />
how a nurse’s documentation may assist<br />
The nurse through charting holds one of the keys to<br />
improved reimbursement for the hospital. There are several<br />
key charting conditions that must be accurate. Most of the<br />
scenarios discussed in this article are applicable to the<br />
hospital in general; some are specific to the Emergency<br />
Department while others pertain to observation patients.<br />
The following re<strong>com</strong>mendations are made in general,<br />
as they are good nursing practice. According to Bonnie<br />
Salvetti, RN, Special Projects Coordinator from Memorial<br />
Hospital of Carbondale, “A hospital is a business. The<br />
nurse’s role in documenting the care that they give and<br />
when they give it impacts the revenue the hospital receives.<br />
Hospitals can then in turn hire more staff, purchase<br />
equipment and update technologies.” Of course accurate<br />
documentation is a joint effort between the hospital and<br />
the nurse. The nurses charting should accurately reflect her<br />
practice and the hospital should allot sufficient time for the<br />
nurse to achieve this objective.<br />
We have always heard during our nurses training<br />
that, ‘If it wasn’t documented, it wasn’t done’. While the<br />
practice of thorough documentation is in the best interest<br />
of patient care and good nursing practice, it also holds true<br />
in the case of hospital reimbursement. There are many<br />
types of reimbursement methods but hospitals typically<br />
receive revenue through accurate billing. Documentation<br />
in the medical record must be accurate and thorough to be<br />
reflected correctly in the bill. This will insure the proper<br />
amount of reimbursement to the hospital. Salvetti goes on<br />
to say, “Nursing documentation affects three major areas.<br />
First, documentation drives observation dollars. Then the<br />
documentation of tests, treatment and services improves<br />
reimbursement. And finally, the accurate documentation of<br />
medication administration has a direct impact on returns.”<br />
A <strong>com</strong>mon source for overlooked revenue is associated<br />
with missed charges for services and procedures that were<br />
<strong>com</strong>pleted but never documented and therefore unable to<br />
be billed. Improving hospital reimbursement is contingent<br />
upon adequate staff education. <strong>Nurse</strong>s in particular<br />
need to understand the essential patient documentation<br />
skills, which are necessary clinically, legally and from a<br />
reimbursement perspective. Salvetti states, “The most<br />
important factor for a nurse to document is every event,<br />
intervention or change in patient condition.”<br />
Correct documentation will capture the correct level<br />
of care that each patient receives. If all possible charges<br />
are captured, the amount of revenue a hospital receives<br />
will be increased thereby justifying future purchases<br />
and staff increase. <strong>Nurse</strong>s can greatly help an institution<br />
by documenting in a consistent, thorough and <strong>com</strong>pliant<br />
manner. In the long run nurses would reap the benefit by<br />
increasing the revenue in the facility in which they work.<br />
According to Contino (2000), “The most <strong>com</strong>mon error<br />
occurs when hospitals don’t code every facet of patient<br />
care. <strong>Nurse</strong>s must document everything they do for a<br />
patient. They must write <strong>com</strong>pletely and legibly. If not,<br />
they may cost the institution revenue.” (p. 15)<br />
Hospitals receive money from many different payer<br />
sources. There are several establishments that pay<br />
insurance claims in the state of Illinois. Medicare is one<br />
of the larger payers of health care claims. According to<br />
the Centers for Medicare and Medicaid Services (2008),<br />
Medicare is a federal insurance program that was created<br />
in 1965 for person’s aged 65 and over regardless of in<strong>com</strong>e<br />
or medical history. In 1972 Medicare extended coverage<br />
to include those people less than 65 years of age who had<br />
disabilities. According to the Kaiser Family Foundation<br />
(2008), there are 1,752,798 Medicare enrollees in the<br />
state of Illinois. Another payer that is a joint federal and<br />
state mediated insurance program is Medicaid. Medicaid<br />
provides payment for health care services including<br />
long-term care and for people with qualifying low<br />
in<strong>com</strong>e. Lastly, there are private insurances. The US<br />
Census Bureau (2008) defines private insurance as nongovernment<br />
coverage provided through an employer or<br />
union or purchased by an individual from a private health<br />
insurance <strong>com</strong>pany. Examples of such agencies include but<br />
are not limited to: Blue Cross Blue Shield, Cigna, Aetna<br />
and numerous others.<br />
Now that the agencies that pay hospital bills have been<br />
identified, it is important to understand that there are other<br />
organizations and public acts that create the rules and<br />
regulations of health care billing. Insurance claims must be<br />
submitted in a particular manner with certain information.<br />
Many different organizations and laws establish the<br />
requirements for billing. These various entities include but<br />
are not limited to:<br />
• False Claims Act (FCA)—This Act provides a legal<br />
tool to counteract fraudulent billings turned in to the<br />
Federal Government.<br />
• Civil Monetary Penalties (CMP)—The Social<br />
Security Act authorizes the secretary of HHS to seek<br />
civil monetary penalties (CMPs) and assessments for<br />
many types of conduct such as presenting claims to<br />
a Federal health care program that the person knows<br />
or should know is for an item or service that was not<br />
provided as claimed or is false or fraudulent<br />
• Health Insurance Portability & Accountability Act<br />
(HIPAA)—An act created to improve portability and<br />
continuity of health insurance coverage in the group<br />
and individual markets, to <strong>com</strong>bat waste, fraud, and<br />
abuse in health insurance and health care delivery,<br />
to promote the use of medical savings accounts,<br />
to improve access to long-term care services and<br />
coverage, to simplify the administration of health<br />
insurance, and for other purposes.<br />
• Emergency Medical Treatment & Active Labor Act<br />
(EMTALA)—The purpose of the statute is to prevent<br />
hospitals from rejecting patients, refusing to treat<br />
them, or transferring them because they are unable to<br />
pay or are covered under the Medicare or Medicaid<br />
programs.<br />
• Stark Physician Referral Prohibition, Antikickback<br />
Statute—This statute prohibits physicians<br />
who have a financial relationship with an entity from<br />
referring their patients to the entity for designated<br />
health services.<br />
• Deficit Reduction Act—Provides states with<br />
flexibility to make significant reforms to their<br />
Medicaid programs<br />
• Reporting Hospital Quality Data for Annual<br />
Payment Update (RHQDAPU)—hospitals must<br />
submit quality performance data for all payers, on all<br />
10 required quality measures to receive the full annual<br />
payment update. Hospitals that do not participate in<br />
RHQDAPU will receive a reduction of 0.4% in the<br />
annual payment update.<br />
• CMS (Centers for Medicare & Medicaid Services)<br />
Condition of Payment—Hospitals are subject to the<br />
Terms and Conditions of Payment when providing<br />
covered services.<br />
• The Joint Commission—An independent, not-forprofit<br />
organization, The Joint Commission accredits<br />
and certifies health care organizations.<br />
• Service Line Accreditation (CLIA, ACR, etc.)—<br />
Various agencies certify performance of departments<br />
within the hospital.<br />
(Continued on page 13)
The Illinois <strong>Nurse</strong> December 2008 Page 13<br />
The <strong>Nurse</strong>s Role in Documentation and Reimbursement . . .<br />
(Continued from page 12)<br />
As rules exist for the mechanism of submitting claims<br />
and receiving payment, there must be governing bodies<br />
that insure adherence to these regulations. On a federal<br />
level, these agencies include: Office of the Inspector<br />
General, Department of Justice, Office of Civil Rights,<br />
Quality Improvement Organizations, Hospital Payment<br />
Monitoring Program, Comprehensive Error Rate Testing<br />
Program, and Medicaid Fraud Control Unit. Private entities<br />
also attempt to make sure that regulations are followed.<br />
These include The Joint Commission and other surveyors.<br />
Additionally, private patients and employers play a role in<br />
reviewing their bills, claims and hospital reimbursement.<br />
Incidentally, hospitals themselves may perform audits to<br />
<strong>com</strong>pare what services were documented in the patient’s<br />
chart against what was charged in an attempt to identify<br />
areas needing improvement.<br />
A new program is being implemented by the Centers<br />
for Medicare & Medicaid Services (2008). Recovery Audit<br />
Contractors (RAC) is a federal program that consists<br />
of Medicare auditors who are paid a percentage of all<br />
identified overpayments and underpayments made to a<br />
hospital. This program will be implemented in all states by<br />
January, 2010. The pilot for the RACs was conducted in<br />
California, New York and Florida and lasted three years.<br />
By reviewing documentation in patient charts and auditing<br />
processed claims and payment, the RACs recovered $371<br />
million in overpayments made to the hospitals.<br />
As discussed, there are rules and regulations for<br />
billing. The “watchdog groups” overseeing <strong>com</strong>pliance<br />
of billing and reimbursement always go back to the chart<br />
for confirmation of what was billed. Naturally, there are<br />
consequences for non-<strong>com</strong>pliance of established billing<br />
guidelines if discrepancies are found in the chart versus<br />
what was billed. The greatest consequence would be<br />
the potential for <strong>com</strong>promised patient safety and quality<br />
of care. Inaccurate or in<strong>com</strong>plete documentation in the<br />
chart could lead to errors and/or to a less than optimal<br />
patient out<strong>com</strong>e. Another implication to the patient for<br />
substandard documentation is the possibility that the<br />
patient could be overcharged.<br />
The hospital as well can suffer financial penalties.<br />
Inaccurate documentation and billing could lead to a<br />
reduction or elimination of payment for services. One<br />
Illinois hospital studied the documentation of IV start and<br />
stop times in the Emergency Department. The result of the<br />
audit showed a potential $400,000.00 loss in charges. The<br />
hospital then in-serviced their nurses on the documentation<br />
of IV start and stop times. Once the training was <strong>com</strong>plete,<br />
a new study realized a 90% improvement in documentation<br />
of IV start and stop times.<br />
A hospital may experience even greater ramifications<br />
to improper billing due to lacking documentation.<br />
Monetary fines could be imposed on the institution. Of<br />
great concern is that the potential exists for hospitals<br />
to be excluded from federally funded programs such as<br />
Medicare and Medicaid for not following guidelines. This<br />
would be a serious implication to hospitals if they were<br />
no longer able to accept Medicare and Medicaid patients.<br />
Other consequences to the hospital could include loss of<br />
non-profit status and loss of license. Bad publicity and<br />
subsequent loss of patients would be the final result of any<br />
of the above actions.<br />
The most basic piece of advice for ensuring accurate<br />
documentation is to make sure that all forms or pieces<br />
of paper in the chart have the patient’s name and account<br />
number. If a form does not have the appropriate identifiers,<br />
there is no proof that the information on those forms<br />
pertains to that specific patient. Additionally, writing the<br />
order to admit a patent is very often in<strong>com</strong>plete. The nurse<br />
must include in the order the type of admission. Is the<br />
admission inpatient, outpatient, observation, surgical or<br />
procedural intervention? To write an order to simply admit<br />
a patient to a particular floor or service is insufficient.<br />
The documentation of medication administration is an<br />
area where improvements could usually be made. Drug<br />
administration services that reflect time are in fact “time<br />
based codes.” Therefore, documentation should support<br />
the billed charges. Remember to sign out all medication<br />
that was given. It may seem obvious to you when the<br />
medication was given but always remember to include<br />
the date and time if it is not clearly notable. Very often<br />
the time of day a patient received a medication affects<br />
their billing. Also, it is extremely important to document<br />
the route a patient received a medication. Frequently a<br />
physician will order a medication to be given PO or IV. It<br />
is up to the nurse to document the actual route given. The<br />
different forms of medication will obviously have different<br />
costs. “In documentation of medication administration,<br />
remember that along with charting the 5 rights, but then<br />
include date, time and length of infusion,” states Salvetti.<br />
For example, a patient <strong>com</strong>es into the ED, the<br />
physician orders Morphine 2 mg PO or IVP. The<br />
nurse documents that the dose was given at 2000. The<br />
RN fails to document the route in which she gave the<br />
med. The hospital will not be able to charge for the<br />
ED nurse’s time in this process.<br />
Intravenous fluids can generate improved revenue<br />
provided the documentation is accurate. Typically,<br />
documentation for infusion services reflects the substance<br />
being infused and the flow rate but that is not enough. It<br />
is important to chart the date and time an infusion was<br />
initiated and stopped. The length of infusion can be varied.<br />
Some items in some areas of the hospital are chargeable by<br />
the minute. An IV that runs for 15 minutes may receive<br />
less money than one that lasts for 60 minutes.<br />
For example, a patient was admitted to observation<br />
status. An IV was started at 1400. There was no<br />
documentation in the patient’s chart regarding the<br />
IV at all. The hospital then has the potential loss of<br />
hundreds of dollars.<br />
With the advent of changes to Medicare reimbursement,<br />
nurse’s documentation is extremely important, especially<br />
on admission. Effective October 1, 2008 the Centers for<br />
Medicare and Medicaid Services (2008) will stop paying<br />
hospitals for the extra care provided to patients to treat<br />
hospital acquired conditions. Medicare finalized a list of<br />
types of conditions for which, it will no longer reimburse<br />
hospitals at the higher diagnosis-related group rate. This<br />
list includes:<br />
• Stage III, IV pressure ulcers<br />
• Fall or trauma resulting in serious injury<br />
• Vascular catheter-associated infection<br />
• Catheter-associated urinary tract infection<br />
• Foreign object retained after surgery<br />
• Certain surgical site infections<br />
• Air embolism<br />
• Blood in<strong>com</strong>patibility<br />
• Certain manifestations of poor blood sugar control<br />
• Certain deep vein thromboses or pulmonary<br />
embolisms<br />
There is an opportunity for nurses to identify conditions<br />
that were actually present on admission and not hospital<br />
acquired. To ac<strong>com</strong>plish this, a nurse must perform a<br />
thorough assessment followed by thorough documentation.<br />
Under the policy change, CMS will only pay for the<br />
treatment of conditions that were present when a patient<br />
was admitted into the hospital.<br />
Some examples of assistive charting include:<br />
Stage III, IV pressure ulcers<br />
Note any minor conditions that are present on<br />
admission as they may inherently worsen during a<br />
patients’ stay at the hospital. The nurse’s notes help ensure<br />
a hospital will not get stuck with the bill if something that<br />
was present on admission turns into a pressure ulcer.<br />
Therefore, thoroughly assess and document any skin<br />
conditions and/or current wounds immediately upon<br />
admission. Remember to clearly document any redness or<br />
possible underlying tissue damage in your patient’s chart.<br />
Fall or Trauma related to injury<br />
For example, a patient is admitted with a CVA. CMS<br />
will fully reimburse the hospital the estimated costs for<br />
the treatment of that condition. Should it be revealed<br />
that the patient has a hip fracture after being admitted<br />
to the hospital, the Medicare payment would not reflect<br />
treatment of that condition. However, if the patient<br />
<strong>com</strong>plained of hip pain on admission and the patient<br />
stated they fell on that affected side prior to admission<br />
and the nurse documents both, it may be considered proof<br />
that the condition existed prior to admission. Mot likely<br />
payment for both diagnoses would be made.<br />
Catheter associated Urinary Tract Infections<br />
For example, if a patient is admitted and a foley<br />
catheter is placed, any subsequent urinary tract infection<br />
would not be reimbursed by CMS. However, if a patient<br />
is admitted with an existing foley catheter and it is<br />
documented as such, payment may be reimbursed at the<br />
optimal level. It is important for the nurse to document if<br />
a patient already has foley catheter upon admission. The<br />
characteristics of the urine must be documented. Always<br />
consult a physician if you suspect the patient already has<br />
a UTI on admission<br />
Vascular catheter associated infections<br />
Similar to the above catheter associated UTI’s, any<br />
infection from a vascular catheter inserted after admission<br />
would result in reduction of payment. Remember to<br />
document if a patient has a vascular device on admission.<br />
Be sure to chart the assessment of that device, its dressing<br />
and condition of surrounding tissue on admission.<br />
It is well known that, documentation provides a legal<br />
health record for the patient. This record provides the<br />
evidence of the care the patient received, a timeline of<br />
the patient’s treatment and the subsequent response to<br />
that treatment. Nursing documentation is the mechanism<br />
to accurately reflect the work done by nurses. The work<br />
nurses do for their patients is important. Charting is<br />
the vehicle for nurses to be recognized for what they do.<br />
Without accurate documentation, however, credit for the<br />
nursing care received and appropriate charging cannot<br />
occur. Terri Williams, RN, E&M Level <strong>Nurse</strong> Specialist at<br />
St. John’s Hospital in Springfield sums it up best by saying,<br />
“Never has nursing documentation been as important as it<br />
is right now.”
Page 14 December 2008 The Illinois <strong>Nurse</strong><br />
HOW TO EARN<br />
CONTINUING EDUCATION CREDIT<br />
This course is 1.5 Contact Hours<br />
1. Read the Continuing Education Article<br />
2. Take the test on the next page.<br />
Complete the entire form<br />
DEADLINE<br />
Answer forms must be postmarked by<br />
November 1, 2010<br />
3. Mail or fax the <strong>com</strong>pleted answer form.<br />
Include processing fee as follows:<br />
INA members—$7.50<br />
Non members—$15.00<br />
Check or money order payable to INA or credit card<br />
information only<br />
MAIL: Illinois <strong>Nurse</strong>s Association<br />
Attn: Sharon Canariato<br />
105 W. Adams, Suite 2101<br />
Chicago, IL 60603<br />
FAX: Credit Card Payments Only<br />
312-419-2920<br />
ACHIEVEMENT<br />
• To earn 1.5 contact hours of continuing education, you<br />
must achieve a score of 75%<br />
• If you do not pass the test, you may take it again at no<br />
additional charge.<br />
• Certificates indicating successful <strong>com</strong>pletion of this<br />
offering will be emailed to you<br />
ACCREDITATION<br />
Illinois <strong>Nurse</strong>s Association is an approved provider of<br />
continuing nursing education by the Georgia <strong>Nurse</strong>s<br />
Association, an accredited approver by the American<br />
<strong>Nurse</strong>s Credentialing Center’s Commission on<br />
Accreditation.<br />
TEST QUESTIONS:<br />
You are a nurse working at your <strong>com</strong>munity hospital. Mr. Smith is a 70 year old male who presents to your facility<br />
with a diagnosis of Heart Failure and Fever. He lives at home with his wife and is a Medicare recipient. He has a history<br />
of Diabetes Mellitus, CVA, Rosacea, GERD and Urinary Retention. The physician orders Lasix 40 mg IVP.<br />
1. What agency is involved in the rules and regulations regarding Mr. Smith’s bill?<br />
A. AHA<br />
B. CMS<br />
C. IRS<br />
2. What consequence could a hospital face for not following the appropriate billing guidelines as it relates to<br />
documentation?<br />
A. A reduction or elimination of payment for service.<br />
B. An increase in the hospital’s infection rate.<br />
C. Closure of the gift shop.<br />
3. After the nurse administers the Lasix, which statement includes all of the information the nurse should document?<br />
A. Right Patient, Right Medication, Right Room Number<br />
B. The amount of time it took the pharmacy to deliver the medication<br />
C. The patient’s name, the name of the medication, the route of the medication, the dose of the medication, the date<br />
and time the medication was given, and the patient’s response to the administration of the medication.<br />
4. Should Mr. Smith require an intravenous infusion during his admission, what nursing documentation would most<br />
greatly affect the reimbursement for the hospital?<br />
A. Date and time the infusion was started, and the date of the tubing change<br />
B. Date and time the infusion was started, and the name of the patient’s roommate<br />
C. Date and time the infusion was started, and stopped<br />
5. What secondary diagnosis should be documented in the care plan to insure patient safety so that he does not sustain a<br />
hospital acquired injury that affects hospital reimbursement?<br />
A. Rosacea<br />
B. CVA<br />
C. GERD<br />
6. What important assessment on admission should the nurse be sure is documented to avoid the hospital incurring<br />
additional costs?<br />
A. The characteristics of the urine and the foley catheter that was present when the patient was admitted.<br />
B. The patient’s bowel sounds<br />
C. The patient’s heart sounds<br />
(Submit entire form below for contact hours)<br />
ANSWER FORM CE #13: The <strong>Nurse</strong>s Role in Documentation and Reimbursement<br />
Please circle the appropriate letter<br />
1. A B C<br />
2. A B C<br />
3. A B C<br />
----------------------------------------------------------------------------------------------------------------------------------------<br />
(Please PRINT clearly)<br />
Name: __________________________________________________________________________________________<br />
Address: _____________________________City:_________________________ State: ___________ Zip: ________<br />
Phone: ________________________________ Email Address: ____________________________________________<br />
----------------------------------------------------------------------------------------------------------------------------------------<br />
Evaluation—CE 1108 Strongly Agree (5) Strongly Disagree (1)<br />
Learner achievement of objectives:<br />
1. List the rules/laws/agencies that regulate health care billing and the consequence 5 4 3 2 1<br />
for non-<strong>com</strong>pliance<br />
2. Outline appropriate nursing documentation and its relationship to 5 4 3 2 1<br />
hospital reimbursement<br />
3. Identify those scenarios not reimbursed by CMS and how a nurse’s documentation 5 4 3 2 1<br />
may assist<br />
How many minutes did it take you to read and <strong>com</strong>plete this program? _______________________________________<br />
Suggestions for improvement? Future topics? ___________________________________________________________<br />
METHOD OF PAYMENT<br />
❑ INA Member ($7.50) INA ID#___________________________<br />
❑ Non Member ($15.00)<br />
❑ Money Order ❑ Check ❑ VISA ❑ Master Card ❑ American Express<br />
Card account number: _______________________________________________<br />
Credit card expiration date: __________ /__________<br />
4. A B C<br />
5. A B C<br />
6. A B C<br />
Signature __________________________________________________ Date ________________<br />
Mail all tests to: INA, Attn: Sharon Canariato, 105 W. Adams, Suite 2101, Chicago, IL 60603<br />
References<br />
Centers for Medicare & Medicaid Services. (n.d.). Hospital acquired conditions. Retrieved September 18, 2008, from http://www.<br />
cms.hhs.gov/apps/media/press/factsheet.asp<br />
Centers for Medicare & Medicaid Services. (n.d.). History. Retrieved September 20, 2008, from http://www.cms.hhs.gov/History<br />
Centers for Medicare & Medicaid Services. (n.d.). RAC permanent program. Retrieved October 20, 2008, from http://www.cms.hhs.<br />
gov/RAC<br />
Contino, D. S. (2000). The ABCs of APCs. Nursing Management, 31(10), 12-16.<br />
Kaiser Family Foundation. (n.d.). Illinois at a glance. Retrieved September 25, 2008, from http://www.statehealthfacts.org/<br />
<strong>com</strong>paremaptable<br />
U.S. Census Bureau. (n.d.). CPS health insurance definitions. Retrieved September 20, 2008, from http://www.census.gov/hhes
The Illinois <strong>Nurse</strong> December 2008 Page 15<br />
INA-PAC<br />
Illinois <strong>Nurse</strong>s Association <strong>Political</strong> Action Committee<br />
<strong>Nurse</strong>s want to provide quality care for their patients.<br />
The Illinois <strong>Nurse</strong>s’ Association <strong>Political</strong> Action Committee (INA-PAC)<br />
makes sure Springfield gives them the resources to do that.<br />
The work of INA-PAC is supported through the generous contributions of its members. In the <strong>com</strong>ing years, some<br />
of the most significant nursing issues could be decided legislatively–making it crucial to maintain a powerful<br />
position among lawmakers in Springfield. Help PAC, help YOU!<br />
So.... if you think nurses need more visibility<br />
.... if you think nurses united can speak more effectively in the political arena<br />
.... if you think involvement in the political process is every citizen’s responsibility<br />
Be<strong>com</strong>e a INA-PAC contributor TODAY!<br />
____ Platinum Level contributor $75.00 or more<br />
____ Gold Level contributor $50.00–74.99<br />
____ Other $_____________<br />
Date: _________________<br />
Please check above your desired level of contribution<br />
Make checks payable to INA-PAC.<br />
Name: _______________________________ E-Mail: ________________________________________<br />
Address: _____________________________________________________________________________<br />
City, State, Zip Code: ___________________________________________________________________<br />
Preferred Phone Number: ________________________________________________________________<br />
Please mail <strong>com</strong>pleted form & check to: Illinois <strong>Nurse</strong>s Association<br />
Atten: INA-PAC<br />
105 W. Adams St., Suite 2101<br />
Chicago, IL 60603<br />
What you need to know<br />
about the INA-PAC<br />
Why should nurses be politically active? Why should<br />
a nurse give money to the INA-PAC? Why should nurses<br />
care who is elected in Springfield and what does it have<br />
to do with their nursing practice anyway? These are just a<br />
few of the questions nurses ask when asked to contribute to<br />
the PAC. Please take a few minutes to read our response.<br />
Why should nurses be politically active?<br />
If we want to be at the table when decisions are made<br />
that effect nurses in Illinois, then we need to be aware of<br />
the politics and issues that are affecting nursing practice.<br />
Not only do we need to be aware, but we need to be in<br />
contact with the legislators. We need to be vocal in our<br />
position on issues that effect our profession.<br />
Why should a nurse give their money to the PAC?<br />
As nurses we need to be concerned with decisions being<br />
made in Springfield. We need to have our voices rise to the<br />
top of heap. To achieve this effectively we need to be sure<br />
that those supportive of our issues are the ones making the<br />
decisions.<br />
Ask yourself, are you concerned about the following<br />
issues?<br />
• Safe nurse staffing standards<br />
• Scope of practice<br />
• Safe patient handling—no manual lifting<br />
• Malpractice reform<br />
• Reimbursement<br />
• Nursing education funding<br />
• Public health funding<br />
• Continuing education<br />
• Funding for uninsured<br />
• Monetary/scholarship support for nursing education,<br />
certification, and training<br />
• Licensure issues<br />
• <strong>Nurse</strong> retention/shortage<br />
• Health care access<br />
• Safe work environment<br />
If so, you should know INA PAC is the only fund set<br />
up that aggressively pursues the election and re-election of<br />
candidates for state office who will stand up and support<br />
the nursing profession on key issues like these, as well as a<br />
long list of other issues critical to our future!<br />
Why should we care about what happens in<br />
Springfield?<br />
As nurses, we should care. Springfield is the place<br />
where the game of politics is played. This is where the<br />
politicians make decisions that determine what we do in<br />
our professional lives. The choice is simple, we can either<br />
learn to play the game or watch from the sidelines.<br />
Since its inception, INA PAC has worked to ensure<br />
the nursing profession speaks as a unified voice, but<br />
also providing us with an influential powerful political<br />
presence in our State Capital. Advocacy is not just having<br />
the “right” position on issues; it’s having the proper<br />
resources to deliver our message and tell our story. The<br />
Illinois <strong>Nurse</strong>s Association PAC is that resource!<br />
As important as it is to be involved in your local<br />
<strong>com</strong>munity by supporting local candidates, it’s equally<br />
as important that we are all involved on the State level as<br />
well. By participating in INA PAC, your voice is heard<br />
collectively with hundreds of nurses across the State who<br />
have a seat at the table of important public policy debates.<br />
If you don’t get involved, you might face the prospect of<br />
bad legislation or a new set of crippling regulations. To<br />
maintain our presence and represent our profession, we<br />
must raise more than $10,000 this year!<br />
The benefits of be<strong>com</strong>ing a regular PAC contributor<br />
are many. You can have a direct voice in endorsement of<br />
candidates by be<strong>com</strong>ing a member of the PAC Board of<br />
Trustees. You will learn more about the political process<br />
as well as having a better understanding of legislation<br />
under consideration in Springfield as a PAC supporter. You<br />
will gain the satisfaction of knowing your contributions<br />
will be going to support candidates that have an interest<br />
in nursing issues, and will assist in educating other nurses<br />
about political activity.<br />
What we need now is your support. Please join INA<br />
PAC today!
Page 16 December 2008 The Illinois <strong>Nurse</strong><br />
2008 “In Memory”<br />
Donations<br />
The following people have had donations made to the<br />
Illinois <strong>Nurse</strong>s Foundation in their memory in 2008. We<br />
appreciate that their support of nursing lives on through<br />
the work of the Illinois <strong>Nurse</strong>s Foundation:<br />
John Cessna, Jr.<br />
Bill Eldert<br />
Maria Gutierrez<br />
Shirley Jones<br />
Imogene King<br />
Gertrude Ladd<br />
Cindy Steury-Lattz<br />
Wanda Marvin<br />
Mary McInnes<br />
Troy Rutledge<br />
Lucille Thacker<br />
Helyn Tharpe<br />
Making Memories<br />
ILLINOIS—When the<br />
donation came in to the Illinois<br />
<strong>Nurse</strong>s Foundation in memory of<br />
Lucille Thacker, its value to the<br />
organization was immediately<br />
identified. But to Ruby Johnson,<br />
Lucille’s daughter, the donation<br />
meant so much more.<br />
“I am so proud of the Foundation, and of being a nurse.<br />
It was so significant to me when I received the letter about<br />
the donation made in my mother’s name. She was so proud<br />
I became a nurse, and to have her memory be part of<br />
what contributes to nursing’s future is fitting, but so much<br />
more,” Johnson said.<br />
Joanie Larsen, INA and INF Board Member, made that<br />
donation. Larsen frequently reaches out to the INF with<br />
donations in memory of loved ones. “I feel it is important<br />
for me to give to nursing, to perpetuate the program and<br />
remind us of those we love,” Larsen said. Choosing to<br />
donate to enhance and improve the nursing profession has<br />
been Larsen’s goal for almost two years. Her desire has<br />
reached many families like Johnson’s and we, the INF,<br />
deeply appreciate her dedication.<br />
INF Seeking Applicants for Davis<br />
Scholarship<br />
The Illinois <strong>Nurse</strong>s Foundation is seeking applicants<br />
for its new Davis Scholarship. This scholarship is for<br />
Registered <strong>Nurse</strong>s looking to continue their education to<br />
be<strong>com</strong>e nursing faculty. Please go to www.illinoisnurses.<br />
<strong>com</strong> for the documents or call 312-419-2900 for more<br />
information.<br />
IllINOIs NURsEs FOUNDATION<br />
Foundation Seeks to Aid<br />
<strong>Nurse</strong>s in Need<br />
The Illinois <strong>Nurse</strong>s Foundation understands times are<br />
hard, but they are even harder for those less fortunate.<br />
In this tough economic environment we have seen many<br />
people suffering without food, clothing or shelter. Among<br />
those in need are nurses. The Illinois <strong>Nurse</strong>s Foundation<br />
has created a Caring Garden to grow a special fund to<br />
provide this much needed assistance. Through your efforts<br />
to grow this fund, you will be tending to the future hopes<br />
of these nurses.<br />
Name:<br />
Address:<br />
City, State Zip:<br />
Donation amount:<br />
Check Check Number:<br />
Credit Card<br />
Visa MasterCard<br />
Card Number :<br />
Expiration Date:<br />
Name on Card:<br />
Verification Code (On back of card):<br />
Mail donations to:<br />
Illinois <strong>Nurse</strong>s Foundation- <strong>Nurse</strong>s in Need<br />
105 W. Adams St.,<br />
Suite 2101<br />
Chicago, IL 60603<br />
<strong>Nurse</strong>s who are facing financial hardship due to illness,<br />
natural disaster, personal or family crisis often have no<br />
place to turn. INF wants to give them hope, one more way<br />
to further our mission to support the nurses of Illinois. The<br />
donation form located here is also on our website at www.<br />
illinoisnurses.<strong>com</strong> Please support these nurses today. This<br />
special fund is the only one of its kind in Illinois; help us<br />
give the nurses in crisis a ray of hope. Donate today!
The Illinois <strong>Nurse</strong> December 2008 Page 17<br />
Amy Taylor, RN<br />
INA Director Membership/Marketing<br />
Bill* was working as a janitor at a local hotel. This<br />
was in spite of the fact he already had his nursing license<br />
reinstated after being disciplined for issues related to<br />
substance abuse. Even though he had ten years of sobriety,<br />
finding a job as a nurse after his license was disciplined<br />
was more difficult than he ever anticipated.<br />
“It seemed as if people couldn’t see past my history to<br />
the person I was today. How I had changed, and the new<br />
insight I had gained were not important. For a while I felt<br />
pretty lost,” Bill said. Facilities wouldn’t extend an offer to<br />
interview, or even call back to say they were not interested.<br />
Is it possible to get a job in nursing after receiving a<br />
discipline on your license? That is a frequent question<br />
asked by callers to the PANN helpline. In this difficult<br />
economic environment, facing unemployment is a serious<br />
and threatening dilemma. It is also frustrating when there<br />
is such a shortage of RNs, let alone experienced RNs.<br />
Laurie*, an RN with her license on probation for<br />
addiction related issues, was able to get hired quickly. “I<br />
was lucky. The managers had a very positive experience<br />
with another nurse in recovery and so they did not think<br />
of my recovery as an obstacle,” said Laurie. She has been<br />
clean for two years as of this interview.<br />
Safeguarding one’s recovery must be a top priority.<br />
Do not accept positions that could be risky if recovery<br />
is relatively recent. <strong>Nurse</strong>s tend to have a “home”<br />
department, such as ICU or ER. Returning to the same<br />
area, even in another organization, is not re<strong>com</strong>mended<br />
because there could be hidden triggers. Stressors such as a<br />
traumatic code, heavy patient assignments or interpersonal<br />
staff conflict could threaten a nurse’s recovery. There are<br />
significant consequences when relapsing after a return to<br />
work. A relapse could cost a nurse not only her job, license,<br />
or career, but also her health or life.<br />
Job Hunting Post-Discipline-<br />
• Be flexible—look for positions away from direct<br />
patient care, e.g., case management or quality<br />
improvement. (See Beyond the Bedside for more<br />
ideas.)<br />
• Be creative—explore opportunities outside of<br />
hospitals such as blood banks, dialysis centers,<br />
New PANN Meeting<br />
Success<br />
The Bolingbrook PANN Meeting that started in<br />
September continues to be successful. New nurses have<br />
been attending every week. PANN meetings are actually<br />
nurse support group meetings. There is a 12 step base, but<br />
topics for discussion may include issues directly related<br />
to nursing, such as license restrictions, job search and<br />
workplace triggers. <strong>Nurse</strong>s at these meetings continue to<br />
attend other support groups, but have voiced how helpful it<br />
is to be able to discuss these professional issues. For more<br />
information on PANN, call 312-419-2900 ext 232 or go to<br />
www.illinoisnurses.<strong>com</strong> and click on the PANN logo.<br />
PANN - Peer Assistance Network for <strong>Nurse</strong>s<br />
Is Discipline a Dead End?<br />
insurance <strong>com</strong>panies, organ donation facilities or<br />
a medical helpline. These positions do not involve<br />
access to narcotics and should provide opportunity<br />
for employment that would not be hindered by any<br />
licensure restrictions if they are present.<br />
• Don’t hide the past—discipline is noted on the Illinois<br />
Department of Financial and Professional Regulation<br />
(IDFPR) website, and is available to Human Resources<br />
departments. Introducing oneself as a “recovering<br />
addict” may not be the best route, but remember<br />
that honesty is the best policy. Describing how you<br />
have changed and what you have learned since the<br />
discipline places a positive and insightful focus on the<br />
experience.<br />
• Be patient—it may take a number of applications to<br />
finally land a position. Don’t give up!<br />
• Maintain objectivity—a job rejection is not personal<br />
even if it feels that way. Receiving a cool, judgmental<br />
reception sends a clear nonverbal message. Why would<br />
someone want to work in a facility that does not view<br />
chemical dependency as a chronic disease that is able<br />
to be managed like hypertension and diabetes?<br />
• You are not alone—more than one nurse has faced<br />
this challenge, and other nurses are currently seeking<br />
reemployment after attaining sobriety. Hopefully these<br />
numbers will increase as we are losing a significant<br />
number of viable contributors to the nursing<br />
workforce.<br />
• Self-care is important—keep support people around,<br />
and seek their reassurance when needed. Everyone is<br />
Advanced Practice<br />
<strong>Nurse</strong>s—PANN<br />
Needs You!<br />
We are creating a contact list of APNs who have<br />
certificates in addictions, and we need to know who<br />
you are. This list will be shared with our nurses facing<br />
issues related to substance abuse. This group has<br />
been cited in the new <strong>Nurse</strong> Practice Act as qualified<br />
to do chemical dependency evaluations, along with<br />
addictionists. Please send your contact information to<br />
ataylor@illinoisnurses.<strong>com</strong> or call 312-419-2900 ext.<br />
232 for more information. Thank you.<br />
Presentations Available<br />
Dee-Dee Patrick, President<br />
of PANN, is available to<br />
speak to healthcare facilities,<br />
universities or other groups on<br />
topics related to the impaired<br />
nurse, substance abuse and<br />
emotional disorders. She has<br />
experience speaking to a wide<br />
variety of audiences, and can<br />
provide the necessary education<br />
needed to better understand<br />
the issues of addiction in the<br />
Dee-Dee Patrick<br />
healthcare professional. You can contact Dee-Dee at (708)<br />
494-0008 or via email at dmp0513@aol.<strong>com</strong><br />
entitled to make a mistake. It is what one does with<br />
life afterwards that really matters.<br />
• Keep your recovery your top priority. Attend nurse<br />
support meetings to discuss your issues and maintain<br />
your objectivity.<br />
*names have been changed per request<br />
What is PANN?<br />
PANN (Peer Assistance Network for <strong>Nurse</strong>s) conducts<br />
peer support meetings that serve as a resource for nurses in<br />
recovery. Topics of discussion include Hidden Workplace<br />
Triggers and Traps, Disclosure in the Workplace,<br />
Interviewing Issues and more. If you are a nurse facing<br />
issues of substance abuse and/or mental illness, or if you<br />
are not certain if you have a problem, please call our<br />
confidential PANN helpline at 1-800-262-2500,<br />
Just as PANN offers education and support to individual<br />
nurses, PANN is available to serve as a resource to<br />
organizations that are open to learning more about the<br />
disease of addiction, especially as it relates to nursing.<br />
Research has shown that negative attitudes and stereotypes<br />
towards individuals with chemical dependency are<br />
inversely related to education about addiction.<br />
<strong>Nurse</strong>s actively involved in their recovery are some<br />
of the most dedicated, empathic and balanced staff in<br />
the profession. They can serve as effective members of<br />
the healthcare team if only provided the opportunity to<br />
demonstrate their knowledge and abilities. Organizations<br />
that support a nurse’s recovery through monitoring,<br />
structured return to work contracts, and mutual respect<br />
will benefit by retaining a dedicated and accountable<br />
health professional.<br />
Beyond the Bedside<br />
Amy Taylor, RN<br />
INA Director Membership/Marketing<br />
It’s often difficult for nurses<br />
who have worked in a clinical<br />
setting, to see options to work<br />
in a nursing capacity away from<br />
the bedside. For many nurses in<br />
recovery, this is an option they<br />
need to consider.<br />
Kathleen Kalber, RN CPUM,<br />
is the Vice President, Care<br />
Management at MCM (Medical<br />
Cost Management). “There are<br />
Kathleen Kalber<br />
definitely opportunities away<br />
from the bedside. Case management and utilization review<br />
are but two options nurses can consider. These positions<br />
allow nurses to utilize their knowledge, and advocate for<br />
patients while coordinating care,” Kalber said.<br />
In utilization management a diverse clinical background<br />
is what is needed. “A wide variety of clinical experience<br />
is always a bonus. Training specific to the documentation,<br />
coding and criteria can be provided through the employer,”<br />
Kalber added.<br />
Positions like these provide nurses the chance to work<br />
even if there are restrictions placed on a license and offer<br />
added benefits of not having to work off shifts, holidays or<br />
weekends.<br />
Would <strong>com</strong>panies consider nurses with licensure<br />
discipline for employment in these roles? “Yes, these<br />
roles would be a good choice for many nurses. I would<br />
encourage any nurse looking for a position away from the<br />
bedside to consider this field. I have found it to be very<br />
rewarding both personally and professionally,” Kalber<br />
said.
Page 18 December 2008 The Illinois <strong>Nurse</strong><br />
Location: Lisle, IL<br />
Contact Hour(s): 60<br />
Approved CE Activities<br />
Offering: 20th Annual Perinatal Nursing<br />
Symposium<br />
Provider: March of Dimes<br />
Offering Date(s): 1/09<br />
Contact Person: Kristina Weinketz<br />
Phone: 312-596-4710<br />
Location: Belleville, IL (1/7/09)<br />
Contact Hour(s): 5.0<br />
Offering: Statistical Concepts for Clinical<br />
Research<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): 3/18-3/20/09; winter 2009 and spring<br />
2010<br />
Contact Person: Adam Greene<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.5<br />
Offering: Drug Development Process<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): 2/12-2/20/09, 10/09 & 2/10<br />
Contact Person: Adam Greene<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.5<br />
Offering: Good Clinical Practices<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): spring 2009 and fall/winter 2009<br />
Contact Person: Adam Greene<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.5<br />
Offering: Fundamentals of Clinical Monitoring<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): spring 2009 & fall/winter 2009<br />
Contact Person: Adam Greene<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.5<br />
Offering: Fundamentals of Site Management<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): spring 2009, fall/winter 2009<br />
Contact Person: Sheryl Johnson<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.5<br />
Offering: Site Leadership and Strategies<br />
Provider: Graham School of General Studies,<br />
University of Chicago<br />
Offering Date(s): Spring 2009<br />
Contact Person: Sheryl Johnson<br />
Phone: 773-702-5537<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.0<br />
Offering: Clinical Research Coordinator Basic<br />
Training: A Practical Introduction to<br />
the Clinical Research Coordinator<br />
Role<br />
Provider: Northwestern University Clinical and<br />
Translational Sciences Institute<br />
Offering Date(s): To be announced through August 2010<br />
Contact Person: Mary Sullivan<br />
Phone: 312-503-7942<br />
Location: Chicago, IL<br />
Contact Hour(s): 22.0<br />
Offering: Certificate in Substance Abuse<br />
Intervention—Courses 3 and 4<br />
Provider: Department of Nursing, Governors<br />
State University<br />
Offering Date(s): Ongoing through January 2009<br />
Contact Person: Catherine Tymkow, ND, MS, APRN,<br />
WHNPC<br />
Phone: 708-534-3144<br />
Location: Independent Study<br />
Contact Hour(s): 90<br />
Offering: Restorative/Rehabilitation<br />
Certification for Licensed <strong>Nurse</strong>s<br />
Provider: Pathway Health Services, Inc.<br />
Offering Date(s): TBA through March 2009<br />
Contact Person: Joy Ward<br />
Phone: 630-734-0233<br />
Offering: Age Related Macular Degeneration<br />
(ARMD)<br />
Provider: Paul Anthony, OD<br />
Offering Date(s): To be determined through December<br />
2009<br />
Contact Person: Paul Anthony, OD<br />
Phone: 217-494-8830<br />
Location: To be announced in Central IL<br />
Contact Hour(s): 1.0<br />
Offering: Cataracts—An Overview<br />
Provider: Paul Anthony, OD<br />
Offering Date(s): To be determined through January<br />
2010<br />
Contact Person: Paul Anthony, OD<br />
Phone: 217-725-4542<br />
Location: To be announced in Central IL<br />
Contact Hour(s): 1.0<br />
Continuing Education Peer<br />
Review Panel<br />
by Kim White, PhD, APRN-BC<br />
The Illinois <strong>Nurse</strong>s Association (INA) reviews<br />
continuing education programs designed for nursing<br />
audiences and gives approval for those that meet<br />
established criteria. There are four INA Continuing<br />
Education Review Panels. Any INA member with a<br />
minimum of a baccalaureate degree in nursing is wel<strong>com</strong>e<br />
to be<strong>com</strong>e a panel member. Previous continuing education<br />
experience is not necessary. Panel experience provides<br />
an opportunity to learn how to write applications for<br />
continuing education. As a continuing education peer<br />
review panel member you can give back to your profession<br />
by facilitating quality continuing education programs,<br />
and giving Illinois nurses access to continuing education<br />
programs.<br />
Those interested in be<strong>com</strong>ing a continuing education<br />
panel reviewer should contact Kemi Ani, Associate<br />
Director of Continuing Education, at 1-800-491-2900 or<br />
KemiA@illinoisnurses.<strong>com</strong>.