MEMBERSHIP MYTH: INA Welcomes Our New ... - nursingALD.com
MEMBERSHIP MYTH: INA Welcomes Our New ... - nursingALD.com
MEMBERSHIP MYTH: INA Welcomes Our New ... - nursingALD.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
An Official Publication of the Illinois Nurses Association The Voice of Illinois Nursing for more than 100 Years<br />
Volume 6 • No. 1 Quarterly circulation approximately 187,000 to all RNs, LPNs, and Student Nurses in Illinois. January 2010<br />
current resident or<br />
Snapshots from Convention<br />
Pages 6 & 7<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
District 2 Presents the<br />
Foundation with a Check<br />
Page 9<br />
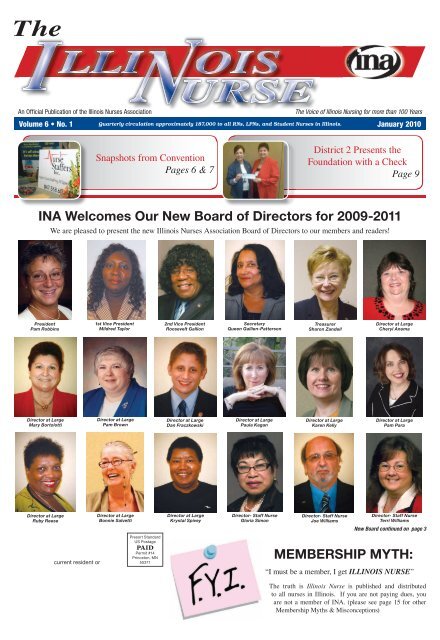
<strong>INA</strong> <strong>Wel<strong>com</strong>es</strong> <strong>Our</strong> <strong>New</strong> Board of Directors for 2009-2011<br />
President<br />
Pam Robbins<br />
Director at Large<br />
Mary Bortolotti<br />
Director at Large<br />
Ruby Reese<br />
We are pleased to present the new Illinois Nurses Association Board of Directors to our members and readers!<br />
1st Vice President<br />
Mildred Taylor<br />
Director at Large<br />
Pam Brown<br />
Director at Large<br />
Bonnie Salvetti<br />
2nd Vice President<br />
Roosevelt Gallion<br />
Director at Large<br />
Dan Fraczkowski<br />
Director at Large<br />
Krystal Spivey<br />
Secretary<br />
Queen Gallien-Patterson<br />
Director at Large<br />
Paula Kagan<br />
Director- Staff Nurse<br />
Gloria Simon<br />
Treasurer<br />
Sharon Zandell<br />
Director at Large<br />
Karen Kelly<br />
Director- Staff Nurse<br />
Joe Williams<br />
Director at Large<br />
Cheryl Anema<br />
Director at Large<br />
Pam Para<br />
Director- Staff Nurse<br />
Terri Williams<br />
<strong>New</strong> Board continued on page 3<br />
<strong>MEMBERSHIP</strong> <strong>MYTH</strong>:<br />
“I must be a member, I get ILLINOIS NURSE”<br />
The truth is Illinois Nurse is published and distributed<br />
to all nurses in Illinois. If you are not paying dues, you<br />
are not a member of <strong>INA</strong>. (please see page 15 for other<br />
Membership Myths & Misconceptions)
Page 2 January 2010 The Illinois Nurse<br />
President’s Message<br />
Transition Strategies: Not Just<br />
For Advance Practice Nurses!<br />
Pam Robbins BSN, RN<br />
President, Illinois Nurses Association<br />
Registered professional nurses<br />
who <strong>com</strong>plete graduate education<br />
achieving an advance practice<br />
nursing (APN) degree deserve a<br />
nod for scholarly progression. As<br />
if educational ac<strong>com</strong>plishment<br />
is not enough, the marketing of<br />
oneself as a new APN graduate<br />
may be the next level of challenge<br />
as one transitions from academic<br />
safety zone to the real work world.<br />
There are many resources to assist<br />
the nurse practitioner with the<br />
“how-to” building of their practice Pam Robbins<br />
ranging from marketing strategies<br />
and service reimbursement basics, billing, the legal specifics<br />
of regulation and collaboration agreements with physicians<br />
(Hamric, 2009) (Buppert, 2008). If that was not enough,<br />
how does one stay centered amongst the rigors of business<br />
and maintain any remnant of your so called life? How does<br />
one seek a work-life balance as the payoff for your efforts of<br />
educational and professional ac<strong>com</strong>plishment? We must look<br />
into our own profession and education preparedness to answer<br />
such questions and heed the same sage advice for ourselves<br />
as we would offer to our patients. The key to reigning-in<br />
anxiety is by valuing self and spirit first. This may sound<br />
selfish and untraditional from the usual sacrifice we as nurses<br />
tend to suffer on the vocational cross. We put everyone ahead<br />
of ourselves, but in all honesty, nurses will burnout using up<br />
everything for others. Who will then provide the healing<br />
strategies to our patients if we do not address what is best for<br />
“self” first?<br />
<strong>Our</strong> successfully <strong>com</strong>bined Illinois Nurses Association/<br />
Illinois Society of Advance Practice Nursing (<strong>INA</strong>/ISAPN)<br />
convention this year featured a motivational speaker, Greg<br />
Risberg CSP, MSW. A social worker at heart, he shared his<br />
insight on how we as a group of nurses view ourselves. He<br />
began his session with a question. “When someone asks<br />
you how are you, what is your immediate response?” The<br />
crowd of registered nurses and APN’s shouted out “fine!”<br />
You and I know, “fine” may be the farthest from the truth,<br />
but for various reasons, nurses, avert attention from self,<br />
and rarely share their true feelings. Greg suggested that<br />
“fine” could be an acronym for F=frustrated, I=irritated,<br />
N=neurotic and E=exhausted. The crowd roared with<br />
laughter, and at the same time the heads in the room<br />
began nodding in affirmation. If “fine” is your acronym<br />
for frustrated, irritated, neurotic and exhausted, then<br />
I re<strong>com</strong>mend considering the five strategies by Bolles<br />
(2002) to fortify yourselves. During transitional periods of<br />
life, whether from academia to practitioner, new parent or<br />
finally embracing a life decision to seek work-balance, you<br />
must sustain a positive outlook with time for self value and<br />
recognition!<br />
• Keep physically fit by developing an action plan that<br />
makes time for positive self-care<br />
• Deal with emotions by building an effective support<br />
network<br />
• Monitor mental stamina, and focus on positive views<br />
• Utilize spiritually for support in difficult times<br />
• Keep active by using time and talents within the<br />
<strong>com</strong>munity<br />
One aspect of nursing is we seem to give away all,<br />
leaving but crumbs for self. We run our proverbial<br />
tank down to empty…expend all of our fuel for one last<br />
“run,” only to find ourselves physically, emotional and<br />
spiritually drained. The term burnout is <strong>com</strong>mon place.<br />
Nurses must achieve a balance of work and life if we truly<br />
want to sustain ourselves in nursing. One nurse spoke to<br />
Greg Risberg and said she felt the response of “fine”<br />
could also reflect an acronym for “feelings inside not<br />
expressed.” Think on how to incorporate Bolles (2002)<br />
re<strong>com</strong>mendations to sustaining a positive outlook during<br />
transitional periods. Find a balance of work and life<br />
that will sustain you. These strategies can be beneficial<br />
not only for APN graduates but for anyone in transition.<br />
Taking care of self is the first place to start! Work towards<br />
answering the question that describes that you are more<br />
than just “fine!” Value self by taking measures to stay<br />
positive and physically fit. Re-energize with emotional and<br />
spiritual connections that keep you healthy and transition<br />
to “anywhere” successfully!<br />
References<br />
Bolles, R.N.(2002). What color is your parachute?<br />
Walnut Creek, CA: Ten Speed Press.<br />
Buppert, C. (2008). Nurse Practitioner’s business<br />
practice and legal guide. (3rd ed.). Sudbury, MA: Jones<br />
and Bartlett.<br />
Hamric, A., Spross, J., & Hanson, L. (2005). Advanced<br />
nursing practice: An integrative approach (4th ed.).<br />
Philadelphia: Elsevier Saunders.<br />
Risberg, Greg CSP,MSW. “You make a Difference”<br />
2009 <strong>INA</strong>/ISAPN convention.<br />
IL L I N O I S NU R S E S AS S O C I A T I O N<br />
President<br />
Pamela Robbins, BSN, RN: pamrobbins@urban<strong>com</strong>.net<br />
First vice President<br />
Mildred Taylor, BSN, RN: m.taylor.rn@<strong>com</strong>cast.net<br />
Second vice President<br />
Roosevelt Gallion, M.Ed, BSN, RN: RG2194@aol.<strong>com</strong><br />
Secretary<br />
Queen Gallien-Patterson, RN: qpatterson@aol.<strong>com</strong><br />
treasurer<br />
Sharon Zandell, RN: sharon.zandel@med.va.gov<br />
Board of Directors:<br />
Cheryl Anema: tccnurse@aol.<strong>com</strong><br />
Mary Bortolotti, RN: mandkbort@aol.<strong>com</strong><br />
Pam Brown: pbrown@brcn.edu<br />
Dan Fraczkowski: dfraczkowski@yahoo.<strong>com</strong><br />
Paula Kagan: pkagan@depaul.edu<br />
Karen Kelly, EdD, RN, CNE-BC: kkellys@aol.<strong>com</strong><br />
Pamela J. Para RN, MPH, CPHRM, ARM, FASHRM:<br />
pjpara2001@yahoo.<strong>com</strong><br />
Ruby P. Reese RN PhD<br />
Bonnie Salvetti: bonnie.salvetti@sih.net<br />
Gloria Simon: galyaodi@yahoo.<strong>com</strong><br />
Krystal Spivey: kspiveyrn@aol.<strong>com</strong><br />
Joe Williams: sangamojoe@aol.<strong>com</strong><br />
Terri L. Williams RN: sewpro9370@aol.<strong>com</strong><br />
District Presidents<br />
1 Roosevelt Gallion: RG2194@aol.<strong>com</strong><br />
2 Mary Bortolotti: mandkbort@aol.<strong>com</strong><br />
3 Sharon Peterson: speterson@crusaderclinic.org<br />
5 Royanne Shultz: royanneschultz@hotmail.<strong>com</strong><br />
8 Ann O’Sullivan: aosullivan@blessinghospital.<strong>com</strong><br />
9 Terri Williams: sewpro9370@aol.<strong>com</strong><br />
10 Jane Bruker: jkbru@aol.<strong>com</strong><br />
13 Janet Lynch: lynch.janet08@gmail.<strong>com</strong><br />
14 Martha McDonald: Martha.mcdonald@sih.net<br />
15 Eunice Mumm: emumm@webtv.net<br />
17 Ann Smith: nevann@<strong>com</strong>cast.net<br />
18 Vacant<br />
20 Cheryl Anema: tccnurse@aol.<strong>com</strong><br />
21 Sandra Webb Booker: stethes@yahoo.<strong>com</strong><br />
E & gW Commission<br />
Sandra D. Robinson, Chair: nursemoney06@yahoo.<strong>com</strong><br />
Linda Briggs: lindasbriggs@yahoo.<strong>com</strong><br />
Nicola Carter: colakola@hotmail.<strong>com</strong><br />
Sandy Fischer: fish23w@yahoo.<strong>com</strong><br />
LaGretta Green: ltg1106@aol.<strong>com</strong><br />
Judith K. Hopkins: Sicu40@aol.<strong>com</strong><br />
Thomas Magana: ndirish01@sbcglobal.net<br />
Virginia Rockett: momynator@yahoo.<strong>com</strong><br />
Christine H. Szkarlat: Christine.Szkarlat@va.gov<br />
Local unit Chairpersons/Co-Chairs<br />
City of Chicago: Timothy Hudson<br />
RC-23 State of Illinois: Lee Goehl<br />
Co-Chair Bill Schubert<br />
St. Joseph: Marlene Murphy and Chris Daly<br />
Union Health Services: Sophie Heldak<br />
University of Chicago: Karen Keller and Tom Magana<br />
University of Illinois: Marcia Hymon (D20), Leo Sherman<br />
VA Hines: Gail Robinson<br />
Christine Szkarlat (D9)<br />
VA North Chicago: Thelma Fuentes<br />
VA Westside: Murrie Davis (D01)
The Illinois Nurse January 2010 Page 3<br />
IL L I N O I S NU R S E S AS S O C I A T I O N<br />
illinois nurses Association/<br />
illinois nurses Foundation<br />
105 W. Adams, Suite 2101 911 S. Second Street<br />
Chicago, iL 60603 Springfield, iL 62704<br />
312/419-2900 217/523-0783<br />
Fax: 312/419-2920 Fax: 217/523-0838<br />
www.illinoisnurses.<strong>com</strong><br />
Executive Director:<br />
Susan Swart, MS, RN: Ext. 229, sswart@illinoisnurses.<strong>com</strong><br />
Chief Financial Officer:<br />
Rick Roche: Ext. 230, rroche@illinoisnurses.<strong>com</strong><br />
Program Director, EgW:<br />
Elwood R. Thompson: Ext. 228, ethompson@illinoisnurses.<strong>com</strong><br />
Deputy Executive Director:<br />
Sharon Canariato, MSN, MBA, RN, Ext. 235<br />
scanariato@illinoisnurses.<strong>com</strong><br />
Director of marketing and member Services:<br />
Deb Weiderman, MS, RN, Ext. 232<br />
dweiderman@illinoisnurses.<strong>com</strong><br />
Associate Director, Continuing Education:<br />
Kemi Ani, Ext. 240 kani@illinoisnurses.<strong>com</strong><br />
E&gW Staff Attorney:<br />
Alice Johnson, Ext. 239, ajohnson@illinoisnurses.<strong>com</strong><br />
E&gW Staff Specialists:<br />
Rick Lezu, 217-523-0783 rlezu@illinoisnurses.<strong>com</strong><br />
Ray Scavone, Ext. 245, rscavone@illinoisnurses.<strong>com</strong><br />
Pam Brunton, Ext. 224 pbrunton@illinoisnurses.<strong>com</strong><br />
Abass Wane, Ext. 249 awane@illinoisnurses.<strong>com</strong><br />
E&gW Coordinator:<br />
Rhonda Perkins, Ext. 223 rperkins@illinoisnurses.<strong>com</strong><br />
Coordinator, Springfield<br />
Staci Moore, 217-523-0783 staci@illinoisnurses.<strong>com</strong><br />
Staff Accountant:<br />
Toni Fox, Ext. 243 tfox@illinoisnurses.<strong>com</strong><br />
Administrative Assistant:<br />
Brenda Richardson, Ext. 248 brichardson@illinoisnurses.<strong>com</strong><br />
Melinda Sweeney, Ext. 222 msweeney@illinoisnurses.<strong>com</strong><br />
Editorial Committee<br />
Theresa Adelman, RN<br />
Alma Labunski, EdD, MS, RN, Chair<br />
Margaret Kraft, RN, PhD<br />
Linda Olson, PhD, RN<br />
Lisa Anderson Shaw DPH, MA, MSN<br />
Mary Shoemaker, PhD, BS, MS, RN<br />
The Illinois Nurse is published quarterly (4 issues yearly) by the<br />
Illinois Nurses Association, 105 W. Adams, Suite 2101, Chicago,<br />
IL 60603.<br />
For advertising rates and information, please contact Arthur L.<br />
Davis Publishing Agency, Inc., 517 Washington Street, PO Box<br />
216, Cedar Falls, Iowa 50613, (800) 626-4081, sales@aldpub.<strong>com</strong>.<br />
<strong>INA</strong> and the Arthur L. Davis Publishing Agency, Inc. reserve<br />
the right to reject any advertisement. Responsibility for errors in<br />
advertising is limited to corrections in the next issue or refund of<br />
price of advertisement.<br />
Acceptance of advertising does not imply endorsement or approval<br />
by the Illinois Nurses Association of products advertised, the<br />
advertisers, or the claims made. Rejection of an advertisement<br />
does not imply a product offered for advertising is without merit,<br />
or that the manufacturer lacks integrity, or that this association<br />
disapproves of the product or its use. <strong>INA</strong> and the Arthur L.<br />
Davis Publishing Agency, Inc. shall not be held liable for any<br />
consequences resulting from purchase or use of an advertiser’s<br />
product. Articles appearing in this publication express the<br />
opinions of the authors; they do not necessarily reflect views of<br />
the staff, board, or membership of <strong>INA</strong> or those of the national or<br />
local associations.<br />
Executive Director’s Update<br />
Susan Y. Swart, MS, RN<br />
<strong>INA</strong> Executive Director<br />
As this new biennium begins<br />
several things are keeping us busy<br />
at the association. We are assisting<br />
in the preparation for a summit<br />
in April. An invitation has been<br />
extended to multiple organizations<br />
to present a summit on the topic<br />
of Educational Advancement for<br />
Registered Nurses. This event will<br />
be open to those interested and will<br />
be held at Heartland Community<br />
College in Normal. I wish to take<br />
a moment to thank Heartland and<br />
their Dean Catherine Miller who Susan Swart<br />
have generously agreed to host<br />
this event.<br />
The Illinois Nurses Foundation is planning its first<br />
“Wisdom of Giving” Benefit. A late spring, early summer<br />
date is in the works. Please keep your eyes out for this<br />
<strong>New</strong> Board continued from page 1<br />
Other individuals elected to office for the 2009-2011<br />
term include:<br />
Congress on Health Policy & Practice<br />
Catherine Neuman<br />
P. Joan Larsen<br />
Ann Smith<br />
Commission on Continuing Education<br />
Kim White<br />
Debra Goodard<br />
Committee on Nominations<br />
Judith Nykiel<br />
Alma Labunski<br />
Patricia Lewis<br />
Mary Petrella<br />
announcement, as we are sure this will be the event to attend.<br />
Proceeds for this brunch will go to expand the scholarship<br />
programs of the Foundation.<br />
A new board was elected at the 80th Biennial Convention<br />
held in Lombard in October. I am pleased to introduce them<br />
to you on the front cover of this issue. A lot of challenges will<br />
be faced by this group as <strong>INA</strong> begins to plan for both the<br />
changing world of healthcare as well as the changing world of<br />
associations. Empowerment of the individual nurse member<br />
will be our focus as we begin to re-define our programs and<br />
services.<br />
The next big project for <strong>INA</strong> will be the launch of our<br />
new publication “CHART.” This journal will be dedicated to<br />
scholarly articles focused on various clinical and professional<br />
issues facing the nurses of Illinois. This will mark a beginning<br />
for <strong>INA</strong> as we shine a spotlight on innovative nursing practice<br />
throughout Illinois. We are reaching out to all clinicians and<br />
educators to submit articles that will help to bring attention on<br />
nursing in Illinois and our impact on the profession. <strong>Our</strong> first<br />
issue will be distributed in the spring of 2010. Please be on the<br />
lookout for the NEW and IMPROVED CHART.<br />
I am sure this will prove to be an exciting year as we<br />
progress into 2010. Please take a few minutes to look through<br />
this issue and discover the work of your colleagues. If you are<br />
not a member of the Illinois Nurses Association, I invite you<br />
to join TODAY. For a meager $4.80/week you can be<strong>com</strong>e<br />
a member of the only nursing association in Illinois that is<br />
dedicated to working on behalf of all nurses throughout this<br />
great state.
Page 4 January 2010 The Illinois Nurse<br />
<strong>New</strong> Illinois Law<br />
Allows Innovative<br />
STD Treatment<br />
Method<br />
John Peller, Director of Government Relations,<br />
AIDS Foundation of Chicago<br />
jpeller@aidschicago.org<br />
Remember that patient who came back again and again,<br />
infected with chlamydia or gonorrhea, because her partner<br />
never got treated? Thanks to legislation recently enacted in<br />
Illinois and supported by the Illinois Nurses Association, a<br />
solution is on its way.<br />
Beginning January 1, 2010, a sexually transmitted<br />
disease (STD) treatment method called expedited partner<br />
therapy (EPT) will be allowed under Illinois law. EPT is<br />
re<strong>com</strong>mended by the U.S. Centers for Disease Control and<br />
Prevention (CDC) and is permitted in 20 states and one<br />
city, Baltimore. 1<br />
With EPT, providers are permitted to prescribe<br />
antibiotics to the partners of patients diagnosed with<br />
chlamydia or gonorrhea, without examining the partner.<br />
Providers can give patients medications or prescriptions to<br />
give to their partners. Providers will be required to counsel<br />
patients and give an information sheet along with the<br />
prescription or medication.<br />
EPT addresses the problem that more than half of<br />
partners of patients diagnosed with chlamydia and<br />
gonorrhea are usually never treated, often because they<br />
are asymptomatic. Both STDs are treated with single<br />
doses of widely-tolerated antibiotics, azithromycin and<br />
cefpodoxime.<br />
Chlamydia and gonorrhea are the two most <strong>com</strong>mon<br />
reportable STDs in Illinois and across the nation. In 2007,<br />
over 55,000 chlamydia cases and over 20,000 gonorrhea<br />
cases were reported in Illinois. STDs can cause severe<br />
and life-long health problems for women, including<br />
pelvic inflammatory disease (PID), infertility, and ectopic<br />
pregnancy.<br />
Illinois’ newest STD treatment law came after a twoyear<br />
effort led by the AIDS Foundation of Chicago (AFC)<br />
and a broad coalition that included the Illinois Nurses<br />
Association. The bill, SB 212, sponsored by State Sen.<br />
David Koehler (D-Peoria) and State Rep. Sara Feigenholtz<br />
(D-Chicago), was signed into law in August by Governor<br />
Pat Quinn. Read the bill text at http://tinyurl.<strong>com</strong>/yfmfpe4.<br />
Significantly, the law gives healthcare providers<br />
protections from lawsuits when providing EPT to patients,<br />
although there are few concerns with the safety of the<br />
treatment method. The immunity provision was negotiated<br />
with the Illinois Trial Lawyers Association, which agreed<br />
that the prescription provided to the partner was free care<br />
seen as a “good Samaritan” act. The state association has<br />
long agreed that providers who give free care should be<br />
immune from lawsuits.<br />
The law requires the Illinois Department of Public<br />
Health to publish guidelines on the practice of EPT.<br />
The guidelines should be available before January 1,<br />
2010, when the law be<strong>com</strong>es effective. In the meantime,<br />
nurses should familiarize themselves with the CDCs<br />
STD treatment guidelines, available at www.cdc.gov/std/.<br />
Advanced practice nurses should review agreements with<br />
supervising physicians to ensure that the agreements allow<br />
for STD treatment or EPT, and update as needed.<br />
For more information on EPT, including guidelines<br />
from other states, visit www.cdc.gov/std/ept/, or visit the<br />
AFC’s website at www.aidschicago.org.<br />
1 U.S. Centers for Disease Control and Prevention,<br />
“Legal Status of Expedited Partner Therapy (EPT)”,<br />
http://www.cdc.gov/std/ept/legal/default.htm, accessed<br />
September 29, 2009.<br />
by Sharon V. Canariato, MSN, MBA, RN<br />
<strong>INA</strong> Deputy Executive Director<br />
In 2008, ANA introduced<br />
an action report which supports<br />
the advancement of a nurse’s<br />
education. <strong>INA</strong> followed with a<br />
position paper supporting ANA’s<br />
action report. Different from<br />
entry into practice, this concept<br />
of advancing a nurses education,<br />
recognizes the value of multiple<br />
points of entry into nursing<br />
education, with the ultimate<br />
goal being baccalaureate<br />
education within ten years of<br />
initial licensure. This approach Sharon V. Canariato<br />
continues to recognize all<br />
educational entries into the<br />
profession while acknowledging the changing healthcare<br />
environment and associated <strong>com</strong>petencies necessary to<br />
adapt to those changes.<br />
A group of nursing leaders from across the state have<br />
formed a task force challenged to develop a nursing<br />
summit to discuss this very issue. Leaders representing<br />
various nursing associations, educators of associate and<br />
baccalaureate nurses and nurse managers have gathered<br />
in a collaborative effort to facilitate a statewide discussion<br />
regarding the feasibility of moving forward with this issue.<br />
The date for this open forum has been set for April 20,<br />
2010 at Heartland Community College. Further details<br />
Practice Corner<br />
Nursing Leaders Gather to Discuss Legislation That Would<br />
Require a Nurse to Attain a Baccalaureate Degree in<br />
Nursing within Ten Years of Initial Licensure<br />
regarding this event, are not yet available. <strong>Our</strong> website<br />
will list the details of the meeting as it be<strong>com</strong>es available:<br />
www.illinoisnurses.<strong>com</strong>.<br />
Some key points regarding the educational advancement<br />
of RN’s include:<br />
• The purpose of requiring the baccalaureate degree for<br />
continued licensure as a registered nurse within ten<br />
years of initial licensure is to be responsive to meet<br />
the increasingly <strong>com</strong>plex health care needs of the<br />
residents of Illinois.<br />
• This preserves associate, diploma and baccalaureate<br />
nursing education. No associate degree or diploma<br />
program would be closed.<br />
• Applies only to future educated graduates of associate<br />
and diploma nursing programs.<br />
• Nurses who are already licensed and students who<br />
have applied to or are enrolled in nursing schools<br />
would be exempt. Due to this clause, the nursing<br />
shortage would not be intensified.<br />
• Seeks to advance the education of nurses to levels<br />
closer to that of the majority of health care disciplines<br />
• There are many avenues for RNs who want to earn<br />
a bachelors degree. In Illinois, there is increased<br />
availability of program articulation.<br />
Rollo May stated, “Communication leads to <strong>com</strong>munity,<br />
that is, to understanding, intimacy and mutual valuing.”<br />
Mark your calendars to join your nursing <strong>com</strong>munity for<br />
this respectful discussion of this important issue.
The Illinois Nurse January 2010 Page 5
Page 6 January 2010 The Illinois Nurse<br />
Snapshots from Convention
The Illinois Nurse January 2010 Page 7<br />
Snapshots from Convention
Page 8 January 2010 The Illinois Nurse<br />
<strong>INA</strong> 2009 HOD Votes to<br />
Influence Health Care<br />
Reform<br />
Below is the letter sent to President Barack Obama and<br />
the US Congress:<br />
Dear President Barack Obama;<br />
On October 17, 2009, the Illinois Nurses Association’s<br />
2009 House of Delegates voted to send letters to President<br />
Barack Obama, the United States Senate, and the House<br />
of Representatives stating that: The Illinois Nurses<br />
Association seeks to influence the Federal Administration,<br />
the U.S. Senate and U.S. House of Representatives to pass<br />
a bill that provides a robust public health insurance option<br />
with fiscal responsibility, no denial of health insurance due<br />
to a pre-existing condition, no loss of coverage due to an<br />
illness, and affordable premiums.<br />
The Illinois Nurses Association has a long history<br />
in support of health care as a right, including accessible,<br />
affordable quality healthcare for all. The American<br />
Nurses Association, of which Illinois Nurses Association<br />
is a constituent member, as well as the United American<br />
Nurses/AFL-CIO, are in support of national health care<br />
reform legislation.<br />
Thank you for listening to the Illinois Nurses<br />
Association,” The Voice of Illinois Nursing for over 100<br />
years”.<br />
The Illinois Nurses Association<br />
2009 House Of Delegates<br />
<strong>INA</strong>-PAC<br />
Illinois Nurses Association Political Action Committee<br />
Nurses want to provide quality care for their patients.<br />
The Illinois Nurses’ Association Political Action Committee (<strong>INA</strong>-PAC)<br />
makes sure Springfi eld gives them the resources to do that.<br />
The work of <strong>INA</strong>-PAC is supported through the generous contributions of its members. In the <strong>com</strong>ing<br />
years, some of the most signifi cant nursing issues could be decided legislatively—making it crucial to<br />
maintain a powerful position among lawmakers in Springfi eld. Help PAC, help YOU!<br />
So. . . . . . .if you think nurses need more visibility<br />
. . . . . . . . .if you think nurses united can speak more effectively in the political arena<br />
. . . . . . . . .if you think involvement in the political process is every citizen’s responsibility<br />
Be<strong>com</strong>e a <strong>INA</strong>-PAC contributor TODAY!<br />
$_____________<br />
Date: ___________________<br />
Please indicate above your desired level of contribution<br />
Make checks payable to <strong>INA</strong>-PAC.<br />
Name: ________________________________________ E-Mail: _________________________<br />
Address: _________________________________________________________________________<br />
City, State, Zip Code: _______________________________________________________________<br />
Preferred Phone Number: ____________________________________________________________<br />
Please mail <strong>com</strong>pleted form & check to: Illinois Nurses Association<br />
Atten: <strong>INA</strong>-PAC<br />
105 W. Adams St., Suite 2101<br />
Chicago, IL 60603
The Illinois Nurse January 2010 Page 9<br />
Illinois Nurses Foundation<br />
Illinois Nurses Foundation Seeks Your<br />
Assistance For Nurses In Need<br />
The Illinois Nurses Foundation understands that times<br />
continue to be challenging, however, they are even harder<br />
for those who are less fortunate. In this tough economic<br />
environment, we have seen many people suffering without<br />
food, clothing and/or shelter. Among those in need may<br />
be nurse colleagues. Many stories such as, tending to<br />
adult children and their children and grandchildren (i.e.,<br />
multigenerational family members living under the same<br />
roof) who have undergone severe crises, dealing with<br />
deaths of immediate family members, multiple injuries<br />
with <strong>com</strong>plications which prohibited their return to<br />
employment, sudden deaths of family members, etc., are<br />
some of the typically reported stories. The Illinois Nurses<br />
Foundation created a CARING GARDEN in order to grow<br />
a special fund for providing this much needed assistance.<br />
Nurses who are facing financial hardships due to<br />
illness, natural disaster, personal or family crisis often<br />
have no place to turn. The Foundation wants to give them<br />
hope as one more way to further our mission in support<br />
of nurses in Illinois. Through your efforts in growing<br />
this fund, you will be tending to the needs and future<br />
hopes of these nurses. A donation form is located here<br />
for your convenience. It is also on our Web site at www.<br />
illinoisnurses.<strong>com</strong>. Won’t you help us give nurses in crisis<br />
a ray of hope? This special fund is the only one of its kind<br />
in Illinois.<br />
Donate to the CARING GARDEN for Nurses in Need<br />
Today!!! Don’t delay!<br />
District 2 presents the<br />
Foundation with a check<br />
Judy Nykiel, INF President; Mary Bortolotti,<br />
District 2 President.<br />
INF Silent Auction<br />
Sells Out!<br />
The Illinois Nurses Foundation held a successful<br />
silent auction during the 2009 Convention. We are happy<br />
to report that every item contributed to the INF Silent<br />
Auction was sold and a total of $2131 was donated to the<br />
Nurses in Need fund.<br />
INF would like to take this opportunity to thank those<br />
individuals who contributed items to this year’s Silent<br />
Auction, including: Cheryl Anema, Ardyss International,<br />
Kathy Blachowski, Farmer’s Guest House - Galena, Sharon<br />
Canariato, Hilton Oak Lawn, Loretta Headrick, HIS<br />
Rest Bed & Breakfast, Alma Labunski, LPGA Teaching<br />
Professional, Charlice Martin, Renaissance Hotel,<br />
Catherine Neuman, Jennifer Nykiel- Donlin, Judy Nykiel,<br />
Tom Nykiel, Ann O’Sullivan, Maureen Shekleton, Susan<br />
Swart, Deb Weiderman, District 19, District 20 and SIUE<br />
Nursing Students.
Page 10 January 2010 The Illinois Nurse<br />
Be True to Your School Nurse<br />
Susan Arndt, RN, MEd<br />
One of the reasons nursing is such a great profession<br />
is that it offers unlimited areas of practice. This not only<br />
allows the nurse to develop an expertise and specialize in<br />
areas of personal interest or significance, but also, within<br />
a lifetime career, a nurse can find new interests and<br />
perhaps change direction. However, the downside of this<br />
specialization is that often times, nurses may not have an<br />
appreciation for what their fellow nurses do. Nowhere is<br />
this most apparent than in the practice of school nursing.<br />
With a goal of building a better understanding of what<br />
school nursing is and what school nurses do, allow me to<br />
share some of the joys and challenges within the practice<br />
of school nursing. To begin with, let’s dispel some myths<br />
about school nursing.<br />
Myth #1 School nursing is boring.<br />
Not even close...!<br />
Expect the unexpected is the rule of thumb for school<br />
nurses. On a good day, a school nurse may provide first<br />
aid care, illness care, a variety of screenings, medication<br />
administration, treatment administration, emotional<br />
support, immunization, and <strong>com</strong>municable disease<br />
monitoring for anywhere between 15 and 80 children.<br />
On a less-than-good day, a school nurse may check 75<br />
heads for the teeniest little buggers that can send a whole<br />
<strong>com</strong>munity into a panic and bring full-grown teachers to<br />
their knees.<br />
And on a very bad day, a school nurse may be called on<br />
to provide care for a life-threatening injury, anaphylaxis,<br />
an act of violence, or even a disaster within the school.<br />
What many nurses do not realize is that school nurses<br />
do all of this without the cushion of other health care<br />
providers at their sides. A school nurse must be able to<br />
make instantaneous decisions and take immediate actions.<br />
A solid knowledge of nursing, extensive educational<br />
preparation and strong clinical skills provide a school nurse<br />
with the ability and confidence to respond independently<br />
and appropriately to any situation.<br />
Myth #2 Any nurse can do school nursing.<br />
That is far from the truth!<br />
School nursing is a very unique area of practice<br />
requiring a basic nursing knowledge, as well as on-going<br />
education in pediatrics, public health, emergency care,<br />
orthopedics, endocrinology, respiratory and neurological<br />
disorders, and new medications and treatments. In Illinois<br />
and many other states, postgraduate work in education<br />
and specialized certification provides a school nursing<br />
specialization.<br />
Furthermore, working within the education field<br />
requires nurses to learn an entirely new system that has<br />
different laws, language, and professionals. Legislation,<br />
such as the special education laws developed within the<br />
last thirty (30) years ensuring the rights of children with<br />
disabilities to receive free and appropriate education and<br />
Section 504 of the Rehabilitation Act ensuring equal<br />
access to education for children with disabilities, has<br />
dramatically changed the landscape and population in our<br />
schools. These changes create new challenges and have<br />
had a huge impact on the practice of school nursing. To<br />
insure <strong>com</strong>pliance and safe care of students, a school nurse<br />
needs an understanding of school law and its impact on her<br />
practice.<br />
Myth #3 School nursing is limited to putting bandaids<br />
on boo-boos.<br />
You must be kidding!<br />
One of the most rewarding features of school nursing<br />
is the positive impact the nurse can have on the academic<br />
success, social development, and self-image of a student.<br />
More importantly is how that academic success, social<br />
development, and self-concept contribute to success as an<br />
adult.<br />
This occurs when school staff recognizes a child<br />
struggling within the school. In a true collaborative effort,<br />
October 17, 2009<br />
<strong>INA</strong> House of Delegates<br />
Memorial Resolution<br />
a team of diverse specialists work to better understand and<br />
solve the problem. This <strong>com</strong>prehensive evaluation includes<br />
assessments and analyses from each specialist that are<br />
used to formulate a plan specific to the child and his or<br />
her needs. In this effort, each specialist contributes his or<br />
her expertise, with team members relying on the nurse for<br />
her insight into any medical condition and its impact on<br />
student academic and classroom functioning. As a valued<br />
member of this education team, the school nurse is in the<br />
sole position to make instructional judgments based on<br />
knowledge of health and school law and her evaluation of<br />
the student’s health.<br />
The product of this collaboration, an Individualized<br />
Education Plan, provides the support the student needs for<br />
success in school. Witnessing a student’s success and its<br />
positive effect on self-esteem is one of the great rewards of<br />
school nursing.<br />
Myth # 4 School nurses have the best schedules:<br />
no weekends, no holidays and summers off.<br />
OK, that one is true!<br />
Yes, school nursing is a great career! One of the reasons<br />
school nursing is such a great career is that by seeking<br />
ways to keep kids healthy and at school where learning<br />
can occur, school nurses focus on wellness more often than<br />
focusing on illness. What’s more, it is rare to drive home<br />
at the end of the day without chuckling over something a<br />
student did. Sure, the challenges are there, but when you<br />
work with kids, it is truly impossible to lose hope.<br />
School nurses, as liaisons between the students, staff,<br />
families, and medical professionals, have opportunities<br />
every day to make a difference in a life.<br />
In the end, nurses gaining an understanding and<br />
appreciation of the other areas of nursing benefit the<br />
profession as a whole. We cannot truly support each<br />
other, celebrate our collective successes, and encourage<br />
our shared challenges until we understand the work and<br />
needs of fellow nurses. As colleagues, let’s <strong>com</strong>mit to<br />
advancing our cause, the art and science of nursing, by<br />
providing support to each other as individual nurses and as<br />
a profession.<br />
Whereas,<br />
Recognition of service and dedication is always appropriate, and although the nursing profession displays these<br />
qualities in abundance, there are outstanding colleagues to be remembered, and<br />
Whereas,<br />
The nurses who have died since the 2005 House of Delegates were enthusiastic participants in the activities of the<br />
profession, American Nurses Association, Illinois Nurses Association, and District Associations, and<br />
Whereas,<br />
Their concern for others, enthusiasm for the profession and willingness to serve will be sorely missed by their<br />
colleagues and <strong>com</strong>munity alike; therefore be it<br />
RESOLVED,<br />
That this House of Delegates memorializes:<br />
• Joyce Waterman Taylor, District 1 a neuro clinical specialist at County Hospital in the 1960’s and active<br />
member of the Cook County bargaining unit;<br />
• John Garde, the longtime Executive Director of the American Association of Nurse Anesthetist and<br />
graduate from the Alexian Brothers Hospital School of Nursing;<br />
• Gladys Niggli, District 10 and <strong>INA</strong> member for 50+ years;<br />
• Mary Elizabeth Carnegie, a champion for minority nurses and the nursing profession;<br />
• Helyn Tharpe, District 10 and <strong>INA</strong> member for 50+ years;<br />
• Kathleen Hoover Papes, a tireless advocate for advancing the economic and general welfare programs<br />
of nurses;<br />
• Joan Duslak, District 19 member who gave many hours in service to our Approver unit as a CE Review<br />
Panel member;<br />
• Imogene King, nursing theorist, who taught at Loyola University from 1961-1966 and again from 1971<br />
to 1980 and received an honorary PhD from Southern Illinois University in 1980;<br />
• and Cindy Steury Lattz, District 17 member and the former <strong>INA</strong> President and<br />
therefore be it further<br />
RESOLVED,<br />
That the principles by which they lived and worked be a constant reminder of the impact one person can make on<br />
the health of a <strong>com</strong>munity and strength of the profession. Their memories will be an inspiration to us all in our<br />
<strong>com</strong>mitment to meet the challenges of the future; and therefore be it further<br />
RESOLVED,<br />
That this House of Delegates pause now for a minute of silence to honor and remember these members and all<br />
former members who marked nursing’s future which we now enjoy.
The Illinois Nurse January 2010 Page 11<br />
‘Livable Communities’<br />
Margaret Ross Kraft, PhD, RN<br />
Member, Editorial Committee<br />
Illinois Nurses Association<br />
Is your <strong>com</strong>munity a good place to grow up and to grow old? A Community for All<br />
Ages? Will your <strong>com</strong>munity meet the needs of those 65, 75, 85, 95 or even 105? If not,<br />
how can a ‘livable <strong>com</strong>munity’ for all ages be created?<br />
The dramatic rise in the numbers of older Americans will impact every aspect of<br />
<strong>com</strong>munities. The entire social, physical and fiscal fabric of <strong>com</strong>munities will be affected<br />
by the growing aging population with an impact on many areas including:<br />
• Housing<br />
• Health<br />
• Transportation<br />
• Land Use Planning<br />
• Public Safety<br />
• Parks and Recreation<br />
• Workforce Development/Education<br />
• Volunteerism/Civic Engagement<br />
• Arts and Cultural Activities<br />
• Economic Development/Fiscal Impact<br />
The development of a ‘livable <strong>com</strong>munity’ project begins with<br />
• Convening key stakeholders<br />
• Assessing existing policies, programs and services that will effect an aging<br />
population (not just aging services)<br />
• Determining challenges and opportunities to be<strong>com</strong>ing an elder friendly<br />
<strong>com</strong>munity<br />
• Engaging citizens, county agencies, businesses and the private sector to develop<br />
and implement an aging in place/<strong>com</strong>munity for all ages plan.<br />
• Getting people to understand that the importance of <strong>com</strong>munity as a whole to<br />
maintaining the quality of life for all citizens—including older adults<br />
• Getting all the key stakeholders at the table in the beginning<br />
• Establishing a shared <strong>com</strong>munity goal/vision<br />
• Tackling issues incrementally—starting small and building on success<br />
• Keeping the momentum going by publicly celebrating ac<strong>com</strong>plishments<br />
(Markham, 2007).<br />
In 2005/2006, the National Council of Area Agencies on Aging in partnership with the<br />
International City/County Management Association, National Association of Counties,<br />
National League of Cities and Partners for Livable Communities with the support of<br />
the MetLife Foundation conducted a national survey of America’s cities and counties to<br />
assess “aging readiness” and found only 46 percent of U.S. <strong>com</strong>munities had even begun<br />
any planning efforts to prepare for their aging population. The <strong>com</strong>munities with plans or<br />
programs in process tended to have addressed only one issue related to elders. The areas<br />
with the experience of heaviest in-migration of older adults were those more likely to<br />
have begun to plan.<br />
Since 1900, the percentage of Americans age 65+ has more than tripled and as the<br />
Baby Boomers age, by 2030, 70 million Americans—twice their number in 2000—<br />
will be 65+. At that point, older Americans will <strong>com</strong>prise 20% of the U.S. population,<br />
representing one in every 5 Americans (Markwood, 2007). In Illinois, the 8 ‘collar’<br />
counties surrounding Cook County (Lake, Dupage, McHenry, Kane, Kendell, Will,<br />
Kankakee, and Grundy) are experiencing an increase in the 60+ population much<br />
faster than the rest of the state. Between 2010-2020, the 60+ population of this region<br />
is expected to increase another 48.74% as <strong>com</strong>pared to 31.58% for the state. The<br />
Northeastern Illinois (NEIL) Area Agency on Aging which provides services in the collar<br />
counties began a ‘livable <strong>com</strong>munity’ initiative in 2008 within four unique <strong>com</strong>munities:<br />
Westmont, Elgin, Kankakee, Highwood, and Lockport. Criteria for participation<br />
included assurance of a mixture of high-density and low-density <strong>com</strong>munities with<br />
at least one chosen <strong>com</strong>munity representative of the economic, racial, ethnic and non-<br />
English speaking households found within the region. By sampling <strong>com</strong>munities already<br />
experiencing high concentrations of older adults in order that the Area Agency on Aging<br />
can assess how these <strong>com</strong>munities have adapted to-date.<br />
The role of NEIL in this ‘livable <strong>com</strong>munity’ project is to serve as consultant<br />
while highlighting the role of local provider agencies in <strong>com</strong>munity decisions as these<br />
<strong>com</strong>munities include the needs of older adults into their <strong>com</strong>munity readiness planning<br />
process The major activities within these four pilot <strong>com</strong>munities will be summarized in<br />
a report to the Illinois Department of Aging and other area agencies in the state. Lessons<br />
learned will help other areas within the state to address the planning for a <strong>com</strong>munity<br />
that can meet the needs of all age groups.<br />
References<br />
Markwood, S. (2007) Partnerships and Initiatives to Develop Livable Communities for<br />
Older Adults. Presentation at the NEIL Annual Meeting. April.<br />
Northeastern Illinois Area Agency on Aging. October 11, 2009. Livable Communities<br />
Progress Report for FY 2009<br />
Dr. Kraft is Assistant Professor, Marcella Niehoff School of Nursing, Loyola<br />
University-Chicago.
Page 12 January 2010 The Illinois Nurse<br />
Correctional Nursing: The Evolution of a Specialty<br />
by Mary V. Muse, MS, RN, CCHP-A<br />
Reprinted with permission from the Winter 2009 issue<br />
of CorrectCare, the quarterly magazine of the National<br />
Commission on Correctional Health Care.<br />
The field of correctional nursing is poised for its next<br />
big advance: specialty certification through NCCHC’s<br />
Certified Correctional Health Professional program. This<br />
is an idea whose time has <strong>com</strong>e. But how did we get here?<br />
Let’s reflect on the evolution of this profession.<br />
A Look at <strong>Our</strong> Past<br />
The specialty of correctional nursing has been visible<br />
for more than 30 years. Although its early days are not well<br />
chronicled, it appears to have emerged largely in response<br />
to the forces that propelled correctional health care in<br />
general, such as the 1976 U.S. Supreme Court ruling in<br />
Estelle v. Gamble.<br />
Before the 1970s, much inmate health care was provided<br />
by other inmates, correctional officers and the occasional<br />
physician. The first documentation of correctional nursing<br />
may be a 1975 article by Rena Murtha, a director of<br />
nursing for a large correctional system. In her account,<br />
nurses were “a tool of the warden, a slave of the physician<br />
and an unknown to the patient.”<br />
Since then, the literature on correctional nursing in<br />
this country has been limited. Some articles describe<br />
blurring boundaries between corrections and nursing,<br />
others found a lack of professional practice or lack of<br />
concern for inmate-patients. For many years, correctional<br />
nurses themselves felt they were viewed as substandard, as<br />
castaways who could not practice anywhere else. Similar<br />
perceptions existed of correctional physicians.<br />
It is true that initially there were no real standards<br />
or expectations for nurses or physicians working in<br />
corrections. Because recruitment was often a challenge,<br />
it was easier to simply hire someone without relying on a<br />
systematic method of reviewing credentials or experience.<br />
However, as standards for correctional health care<br />
emerged, such as those of the National Commission on<br />
Correctional Health Care, likewise standards for health<br />
professionals took hold. These standards guided provision<br />
of care in jails and prisons, helping to improve quality and<br />
to reduce negative stereotypes.<br />
Despite these advances and the hiring of better qualified<br />
nurses, the perception persisted that good nurses would not<br />
work in corrections. In large part, this belief stems from<br />
the lack of knowledge about the environment and practice<br />
of correctional nursing, often coupled with fear and,<br />
occasionally, instances of nurses taking on aspects of their<br />
security counterparts. Consequently, some nurses left this<br />
field and others were reluctant to choose it.<br />
It didn’t help that many facilities lacked the leadership<br />
and structure for nurses that exist in traditional health<br />
care settings In years past, nurses usually reported to a<br />
corrections administrator or to a physician. In the absence<br />
of solid knowledge and expertise in nursing theory and<br />
standards, this reporting structure failed to optimize<br />
nursing practice in correctional health care.<br />
A Critical Role<br />
Correctional nursing has experienced considerable<br />
growth in the past 30 years. The <strong>com</strong>plex health needs<br />
of patients entering our systems require nurses with<br />
specialized knowledge and skill. Today, correctional<br />
nurses play a critical role in ensuring inmates’ access to<br />
care and in health care delivery. It is the nurse with whom<br />
the inmate interacts most frequently and whom the officer<br />
consults when an inmate has a health problem.<br />
As in most health care settings, correctional nurses are<br />
the primary clinical providers of care. Registered nurses<br />
are necessary to lead care delivery, as well as to direct the<br />
licensed nurses who work under their guidance.<br />
Correctional nurses must be clinically <strong>com</strong>petent and<br />
well grounded in nursing practice. They must possess<br />
excellent skills in assessment and critical thinking. Their<br />
judgment is critical to the inmates’ access to care.<br />
It’s also important to have a good understanding of<br />
the level of care that can be provided in their institutions.<br />
Correctional facilities can ill afford to have nurses who<br />
cannot or will not practice within the scope of their license<br />
or correctional nursing standards, or who have an aversion<br />
to the patient population they are expected to serve.<br />
Thus, correctional nurses have a high degree of<br />
accountability and responsibility. The flip side, naturally,<br />
is that they also are highly subject to possible litigation.<br />
Today, many facilities have added correctional<br />
nurse administrators to their staff. Under this structure,<br />
expectations for nursing practice are clearly defined<br />
and quality is strongly promoted. The growth in<br />
nursing leadership positions has contributed greatly to<br />
improvements in delivery of services and quality of care.<br />
A Distinct Specialty<br />
As the practice of correctional nursing has coalesced,<br />
it was natural that professional organizations would step<br />
up to foster professionalism in this<br />
specialty. The American Nurses<br />
Association, for example, promulgates<br />
standards for correctional nursing.<br />
The ANA defines nursing as<br />
“the protection, promotion and<br />
optimization of health and abilities,<br />
prevention of illness and injury,<br />
alleviation of suffering through the<br />
diagnosis and treatment of human<br />
response, and the advocacy in the care<br />
of individuals, families, <strong>com</strong>munities,<br />
and populations.” Nurses’ broadbased<br />
knowledge and holistic focus positions them as the<br />
logical network of providers on which to build health care<br />
systems with a focus on education, practice and facilitating<br />
patients’ efforts to meet their fullest potential.<br />
The ANA’s Corrections Nursing: Scope and Standards<br />
of Practice was revised in 2006 with input from nurse<br />
Correctional nursing<br />
is poised for its next<br />
big advance: specialty<br />
certification. To learn about<br />
this CCHP program, see<br />
www.ncchc.org/cchp.<br />
leaders across the country. The standards state that<br />
“Matters of nursing judgment are solely the domain of<br />
the registered nurse.” A major emphasis of this work<br />
is primary health care. These services include intake<br />
screening and evaluation, health screening, direct patient<br />
care, assessment and evaluation of an individual’s health<br />
behavior, teaching, counseling and helping inmates to<br />
assume responsibility for their own health. The nurse also<br />
may identify and provide <strong>com</strong>munity linkages for inmates<br />
upon discharge.<br />
Thanks to the increasing professionalism in correctional<br />
nursing, our colleagues in the correctional health care<br />
arena now understand and appreciate the value of this<br />
specialty. Beyond the walls, as well, negative perceptions<br />
are fading and enthusiastic interest in correctional nursing<br />
is growing, both in the <strong>com</strong>munity and from academic<br />
institutions.<br />
It is not clear how many nurses work in correctional<br />
health care settings. However, several years ago a national<br />
study of the nursing workforce reported 18,033 RNs<br />
working in this field.<br />
Opportunities Ahead<br />
Clearly, correctional nursing is on a roll, and even<br />
greater opportunities lie ahead. Last spring, CCHP<br />
program leaders began to explore the development of<br />
specialty certification for correctional nursing. Given that<br />
53% of the more than 2,000 active CCHPs are nurses, this<br />
only made sense.<br />
Certification is the formal recognition of specialized<br />
knowledge, skills and experience that demonstrate<br />
<strong>com</strong>petence and achievement of standards of a specialty<br />
that fosters and promotes optimal health out<strong>com</strong>es. A key<br />
part of the CCHP program is a test designed to measure a<br />
candidate’s mastery of the specialty.<br />
Aided by a nurse consultant with expertise in test<br />
design and psychometrics, a CCHP task force of nurse<br />
leaders started by listing nursing task statements that<br />
describe correctional nursing and distilling this list to its<br />
key essentials. These statements were<br />
used to develop a job analysis survey<br />
tool, which was sent to a broad group<br />
of correctional nurses. The results<br />
guided and validated the development<br />
of a test for specialty certification.<br />
Certification for correctional<br />
nursing helps to legitimize this<br />
specialty and validates that these<br />
professionals must possess a unique<br />
body of knowledge and skills.<br />
Just as important, it will certainly<br />
inspire others to pursue careers in<br />
correctional nursing and will stimulate scholarly research<br />
in this field.<br />
Correctional nursing has reached a milestone. <strong>Our</strong><br />
next challenges include expanding the knowledge of<br />
correctional nursing by seeking to more clearly define the<br />
profession, to identify the various levels of care delivered<br />
by nurses, to document the impact of nursing care on<br />
patient out<strong>com</strong>es and to pursue research and evidencebased<br />
practice.<br />
This is a wonderful time for correctional nurses, our<br />
patients and the field of correctional health care as a<br />
whole.<br />
Mary V. Muse, MSN, RN, CCHP-A, is a correctional<br />
health care consultant based in the Chicago area. She is<br />
a surveyor for NCCHC, a frequent presenter at NCCHC<br />
conferences and immediate past chair of the Academy of<br />
Correctional Health Professionals. She also serves on the<br />
task force that is developing the CCHP-N program. To<br />
contact her, e-mail mvmuse@ameritech.net.<br />
The ANA book Corrections Nursing: Scope and<br />
Standards of Practice is available for purchase from<br />
NCCHC. See our catalog at www.ncchc.org or call 773-<br />
880-1460.
The Illinois Nurse January 2010 Page 13<br />
POSITION STATEMENT ON<br />
CULTURAL COMPETENCE WITH AGING<br />
ExECutivE SummARy<br />
The Illinois Nurses Association (<strong>INA</strong>) supports<br />
the position which promotes culturally <strong>com</strong>petent<br />
professionals who integrate health care delivery services<br />
for all individuals regardless of age and culture. It reflects<br />
practice with <strong>com</strong>passion and respect for the inherent<br />
dignity, worth and uniqueness of all human beings. The<br />
<strong>INA</strong> supports implementation of continuing education<br />
for all professional and auxiliary health care delivery<br />
personnel regarding integration of culturally diverse health<br />
care services for older adults.<br />
BACkgROunD<br />
Given an aging population, currently registered by the<br />
United States Bureau of Census as 49 million individuals<br />
who are 65 years of age and over, significant trends are<br />
impacting the future of aging in the United States. First,<br />
older adults are increasing their life span; the aging<br />
population is rapidly growing with 78 million baby<br />
boomers soon reaching the age of 65 and over, (births<br />
between 1941-1965) (Tucker, etal., 2006). Such populations<br />
will reach major proportions by the year 2030. Hence,<br />
the nation’s capacity to provide quality and affordable<br />
care for its rapidly growing adult population will be<strong>com</strong>e<br />
increasingly challenging.<br />
Also, the “face” of aging is changing nationwide.<br />
It is quickly be<strong>com</strong>ing a sea of cultural diversity. The<br />
many cultures, ethnicities, abilities, skills, values and<br />
experiences, span from over 60 to 100 years of age. And,<br />
given the increasing longevity in all cultures, more older<br />
adults will require health services for <strong>com</strong>plex, chronic,<br />
and possibly disabling conditions. These numbers,<br />
diversity and location will impact the way health care is<br />
delivered. Additionally, the location of care delivery, which<br />
varies from acute care to <strong>com</strong>munity settings, promotes a<br />
dramatic increase in the demand for professionals to care<br />
for them. Only 4.5% of older adults reside in institutions<br />
(Administration on Aging, 2004); 65-74 year olds live with<br />
spouse, and/or next of kin within the <strong>com</strong>munity. Those<br />
over 75 years of age generally live alone.<br />
The changing face requires professionals to be culturally<br />
<strong>com</strong>petent in integrating health care needs, values,<br />
traditions and lifestyles. Since chronic diseases affect 88<br />
percent of older adults (ASA, 2006), a disproportion of<br />
them are attributed to specific, culturally diverse groups<br />
(Suen & Tusale, 2004). Survival rates similarly vary among<br />
culture and gender; American females’ life span mean<br />
is currently 79.4; males 73. In the Chinese and Filipino<br />
culture, men outlive the women (Suen & Tusale, 2004).<br />
Higher poverty disparity rates exist for older women<br />
more than older men: greater impoverishment exists<br />
among the culturally diverse; as <strong>com</strong>pared with 25% of<br />
white women, over 40% of African American and Latin<br />
women live in poverty during their retirement years (Aging<br />
Today, 2006).<br />
Given the changing status, stereotypes regarding aging<br />
continue to pervade the culture. Negative attitudes such<br />
as, workplace skills; limited physical activity; myths<br />
regarding independence, driving skills, and long term care;<br />
gender disparities; discrimination in health care delivery;<br />
Social Security, Medicare and Medicaid status; etc., persist<br />
in perceived disparities among all cultures (Sampson &<br />
Staplin, 2003).<br />
In current health care delivery, since more than one<br />
half of hospitalized clients represent adults over 65 (Yoon,<br />
etal., 2006), only nine percent of professional nurses have<br />
indicated an interest in caring for older adults. The current<br />
shortage of registered nurses specializing in gerontological<br />
nursing magnifies the challenge. It will be<strong>com</strong>e more<br />
critical as student preferences for other nursing specialties<br />
contribute to the current shortage, with only 1.9% of<br />
students who identify working with older adults as their<br />
career choice (AACN, 2005).<br />
In the year 2000, a national survey was conducted<br />
among 590 baccalaureate educational programs; of those,<br />
only 38 reported requiring a separate gerontological theory<br />
and clinical course at the undergraduate level (Labunski,<br />
2005). Rationale for lack of inclusion was three-fold:<br />
faculty stated that aging adults were merely adults and had<br />
the same problems, thus should be not be separated. Also,<br />
students were exposed to older adults in clinical settings<br />
and long term settings early in their educational programs,<br />
which promoted even greater negative attitudes toward the<br />
aged. Third, students reported that student attitudes were<br />
affected by their faculty’s attitudes toward aging, hence,<br />
showed little interest in serving the aged.<br />
Professionals’ statements included, “although I was<br />
hesitant about spending an entire semester in this course,<br />
I really enjoyed the content and consider it so important<br />
for this population which deserves our best,” and, “this<br />
gerontological course needed to be added …; there are a<br />
lot of myths which were dispelled by taking this course; it<br />
has helped me with all of my nursing considerably” (Aud,<br />
etal., March-April 2006)<br />
In June 2001, the American Association of Colleges of<br />
Nursing (AACN) was awarded an extensive grant by the<br />
Hartford Foundation of <strong>New</strong> York to enhance curriculum<br />
development in 20 baccalaureate and 10 graduate schools<br />
of nursing. Over the four year grant program, survey<br />
results revealed that the single most necessary precursor<br />
to the successful implementation and maintenance of<br />
geriatric curricula, is faculty development—expanding<br />
their knowledge base and fostering positive attitudes<br />
toward aging (Aud, etal., March-April, 2006).<br />
Further, students need a separate, solid grounding in<br />
the art and science of gerontological nursing theory and<br />
an opportunity to apply the theory and interact with older<br />
adults in diverse clinical sites (Hancock, etal., 2006).<br />
Also, traditional early clinical sites, as in long term care<br />
facilities, although offer a slower paced environment,<br />
perpetuate the myth that the care of long term home<br />
residents requires less expertise in nursing skills,<br />
assessment, critical thinking and leadership as <strong>com</strong>pared<br />
with the care of hospitalized patients. It ignores the<br />
<strong>com</strong>plexity of nursing home residents who reflect multiple<br />
chronic conditions, <strong>com</strong>plex medication regimens, endof-life<br />
issues, decision-making and rehabilitative services<br />
post-hospitalization and in specialized care for dementia.<br />
It further ignores population statistics which as indicated<br />
above, reveal that only a small percentage of older adults<br />
reside in nursing homes (Administration on Aging, 2004).<br />
POSitiOn<br />
The Illinois Nurses Association (<strong>INA</strong>) strongly opposes<br />
the persisting, current culture of ageism. The <strong>INA</strong> supports<br />
implementation of the following interventions to promote<br />
culturally <strong>com</strong>petent professionals who integrate all<br />
culturally diverse health care services by :<br />
1. Laying the groundwork for older adults theory and<br />
clinical curricula in undergraduate programs by:<br />
a. providing faculty education and development; b.<br />
instituting separate, required undergraduate courses<br />
in gerontological nursing as part of the nursing<br />
major; and, c. thereafter, offering graduate tracks<br />
in aging adults. These suggest much hope and<br />
potential for dispelling myths regarding aging and<br />
the current culture.<br />
2. Promoting culturally <strong>com</strong>petent health care<br />
delivery , which reflects practice with <strong>com</strong>passion<br />
and respect for the inherent dignity, worth and<br />
uniqueness of every individual (ANA, 2001)<br />
3. Instituting continuing education for all professional<br />
and auxiliary health care delivery personnel<br />
regarding integration of culturally diverse health<br />
care services for older adults.<br />
4. Creating a culturally appropriate health promotion<br />
program that improves awareness, enhances<br />
motivation, builds skills and provides opportunities<br />
for physical activities and advocacy, protection,<br />
health safety and rights for all older adults ( ASA,<br />
Summer 2006), (ANA 2001).<br />
REFEREnCES<br />
Administration on Aging. (2004). A profile of older<br />
Americans. U.S. Department of Health and Human<br />
Services, Washington: DC.<br />
American Association of Colleges of Nursing. (2005).<br />
Media - nursing shortage resource; www.aacn.nche.edu<br />
American Association of Colleges of Nursing and John<br />
A. Hartford Foundation Institute for Geriatric Nursing.<br />
(2000). Older Adults: Re<strong>com</strong>mended Baccalaureate<br />
Competencies and Curricular Guidelines for Geriatric<br />
Nursing Care. Washington, DC: AACN.<br />
American Nurses Association. (2001). ANA Code for<br />
Nurses with Interpretive Statements. Kansas City: MO,<br />
ANA.<br />
Aud, M., Bostick, J., Marek, D., & McDaniel, R. (2006).<br />
Introducing baccalaureate student nurses to gerontological<br />
nursing. Journal of Professional Nursing, 2(2), 73-78.<br />
Buerhaus, P., Staiger, D., & Aurbach, D. (2000).<br />
Implications of an aging registered nurse workforce.<br />
JAMA, 28 (2), 2948-2954.<br />
Gordon, C.(Summer 2006). Promoting exercise for<br />
elders of color, Health Care and Aging. American Society<br />
on Aging, 13(2).<br />
Hancock, D., Helfers, M., Cowan, K., Letuak, S.,<br />
Barba, B., Herrick, C., Wallace, D., Rossen, E., &<br />
Bannon, M.(2006). Integration of gerontology content in<br />
nongeriatric undergraduate nursing courses. Geriatric<br />
Nursing, 27(2), 103-111.<br />
Hounsell, C. & Riojas, A.(2006). Older women face<br />
tarnished golden years. Aging Today, 27(4), American<br />
Society on Aging.<br />
Institute of Medicine. (2001). Crossing the Quality<br />
Chasm: A <strong>New</strong> Health System for the 21st Century.<br />
Washington: DC, National Academy Press.<br />
Kane, R. and Kane, R. (2005). Ageism in healthcare and<br />
long-term care, ageism in the new millenium. Generations,<br />
29(3), 49-54.<br />
Labunski, A. J. (2005). Ethics or conflict in health care.<br />
American Society of Aging, National Council on Aging,<br />
Philadelphia, PA.<br />
Labunski, A. J. (2003). Dementia care: whose ethics?<br />
American Society of Aging, National Council on Aging,<br />
Chicago: IL<br />
Latimer, D. & Thornlow, D. (2006). Incorporating<br />
geriatrics into baccalaureate nursing curricula: laying<br />
the groundwork with faculty development. Journal of<br />
Professional Nursing, 22(2), 79-83.<br />
National Commission on Nursing Workforce for Long-<br />
Term Care. (May 2005). Act Now for Your Tomorrow,<br />
Washington: DC National Commission on Nursing<br />
Workforce.<br />
Nigg, C. (2006). Helping older adults strengthen their<br />
level of <strong>com</strong>mitment to exercise, one stage at a time.<br />
Health Care and Aging, 14(2), American Society on<br />
Aging.<br />
Rosowsky, E. (2005). Ageism and professional training<br />
in aging: who will be there to help? Ageism in the <strong>New</strong><br />
Millenium. Generations, 29(3), 55-58.<br />
Sampson, S. & Staplin, L. (2003). Myths and facts<br />
about older drivers, Generations, 27(2), 32-33.<br />
Suen, L. & Tusaie, K. (2004). Is somatization a<br />
significant depressive symptom in older Taiwanese<br />
Americans? Geriatric Nursing, 25(3),157-163.<br />
Thornlow, D., Auerbahn, C. & Stanley, J. (2006). A<br />
necessity, not a luxury: preparing advanced practice nurses<br />
to care for older adults. Journal of Professional Nursing,<br />
22(2), 116-122<br />
Tucker, D., Bechtel, G., Quartana, C., Badger, N.,<br />
Werner, D., Ford, I., & Connelly, L. (2006). The OASIS<br />
program: redesigning hospital care for older adults.<br />
Geriatric Nursing, 27(2), 112-117.<br />
Yoon, S. & Schaffer, S. (2006). Herbal, prescribed and<br />
over-the-counter drug use in older women: prevalence of<br />
drug interactions. Geriatric Nursing, 27(2), 118-129.<br />
Wallace. S. (2006). Closing the gap: health disparities<br />
among older Americans. Aging Today, 27(4), American<br />
Society on Aging.<br />
Wilson, K. (2006). Introduction: where older people<br />
live, how needed care is provided, Generations, 29(4), 5-8.<br />
Effective Date: August 1997, December 2006<br />
Status: Revised Position Statement<br />
Originated by: The Assembly on Health Policy<br />
Primary Author: Alma J. Labunski, EDD, mS, Rn<br />
Adopted by: Illinois Nurses Association
Page 14 January 2010 The Illinois Nurse<br />
Are You Interested in<br />
Be<strong>com</strong>ing a Nurse Educator?<br />
If you currently have your Master’s degree in Nursing,<br />
you are qualified to teach in an RN nursing program.<br />
Teaching as an adjunct faculty member is a great way to<br />
enhance your career and help prepare the next generation<br />
of nurses. Most schools throughout the state are looking<br />
to hire part-time and full-time nurse educators. Open<br />
positions for some schools can be found at www.nursing.<br />
illinois.gov.<br />
The Clinical Faculty Academy is a great resource for<br />
new and seasoned educators. The program is a two-day<br />
skill building program for registered nurses who have a<br />
contract to serve as clinical faculty at an Illinois nursing<br />
program. The mission of the Academy is to develop<br />
qualified Master’s prepared nurses for the role of clinical<br />
nurse educators in order to increase faculty workforce,<br />
which will expand and sustain enrollments in schools of<br />
nursing.<br />
For more information on up<strong>com</strong>ing Clinical Faculty<br />
Academies across the state, or if you would like to plan an<br />
Academy in your region, please contact Mary Pat Olson,<br />
RN, MPH, Director of Workforce Development for the<br />
Metropolitan Chicago Healthcare Council at 312-906-<br />
6020, mpolson@mchc.<strong>com</strong>.<br />
Mary Petrella presents “My Hero, My Dad The Nurse”<br />
to St Joseph’s School in Joliet<br />
Mary Petrella (left) and Debbie Oriva
The Illinois Nurse January 2010 Page 15<br />
Membership Myths &<br />
Misconceptions<br />
“inA must have thousands of members—they don’t need dues or help from<br />
me.”<br />
Sadly—not true. Similar to public TV or radio which benefits all listeners<br />
(whether or not they are paying members) <strong>INA</strong> provides information, political<br />
advocacy and other services which benefit all Illinois nurses, but receives<br />
financial support from only a small percentage. Currently there are over 166,000<br />
RNs in Illinois and only 5,200 of these are members of <strong>INA</strong>.<br />
“i don’t need to be a member – someone else will take care of all that.”<br />
If not YOU, then WHO—you are the “someone else.” Non-nurses (physicians,<br />
insurance <strong>com</strong>panies, hospital administrators, trial lawyers, etc.) are waiting in<br />
line to define nursing. Without the financial support of the nurses in Illinois, <strong>INA</strong><br />
has limited ability to protect your rights as a professional registered nurse.<br />
“inA is only a union”<br />
Yes and No. We are a multi-purpose organization that provides services to<br />
all nurses in Illinois regardless of their specialty, place of employment or<br />
educational preparation. <strong>INA</strong> does provide union representation for registered<br />
nurses working in certain facilities. We are PROUD of our union work. Who<br />
else should be representing nurses in their work place if NOT NURSES? But we<br />
refuse to be defined as ONLY A UNION!<br />
“inA is made up of all nurse managers and educators—they don’t represent<br />
staff nurses.”<br />
<strong>Our</strong> membership is over 70% staff nurses that work at the bedside. <strong>Our</strong><br />
elected leadership includes a wide range of nurses from new grads and direct<br />
care staff to managers, educators and retirees. <strong>Our</strong> diversity is what makes us<br />
STRONGER.<br />
“inA is only interested in hospital nurses and policies”<br />
The association, since its’ founding in 1901, has supported and advocated<br />
for all registered nurses in Illinois—in all work settings—and across all nursing<br />
specialties. We even extend affiliate membership status to those such as the<br />
school nurses association.