APPROACH TO RASHES MACULOPAPU LAR RED ... - rEMERGs
APPROACH TO RASHES MACULOPAPU LAR RED ... - rEMERGs
APPROACH TO RASHES MACULOPAPU LAR RED ... - rEMERGs
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>APPROACH</strong> <strong>TO</strong> <strong>RASHES</strong><br />
<strong>MACULOPAPU</strong><br />
<strong>LAR</strong> <strong>RED</strong> RASH<br />
Viral exanthem<br />
NOS<br />
Rubeola<br />
Rubella<br />
Roseola<br />
Erythema<br />
Infectiosum<br />
Scarlet Fever<br />
RockyMtn<br />
Spotted F<br />
Hand-foot-mouth<br />
Kawasaki’s<br />
disesase<br />
Drug eruption<br />
Staph scalded skin<br />
Staph toxic shock<br />
Strep toxic shock<br />
Erythema<br />
Multiforme<br />
Steven’s -<br />
Johnson<br />
Psoriasis<br />
Urticaria<br />
Pityriasis Rosea<br />
Disseminated<br />
gonorr<br />
Scabies<br />
<strong>MACULOPAPU</strong><br />
<strong>LAR</strong> <strong>RED</strong> AND<br />
SCALY RASH<br />
+/- Patches and<br />
Placques<br />
Pityriasis Rosea<br />
Atopic Dermatitis<br />
Contact<br />
Dermatitis<br />
Seborrheic<br />
dermatitis<br />
Tinea capitis<br />
Tinea corporis<br />
Tinea pedis<br />
Tinea versicolor<br />
Lichen plannus<br />
PAPU<strong>LAR</strong> OR<br />
NODU<strong>LAR</strong><br />
RASH<br />
Pediculosis<br />
Scabies<br />
Molluscum<br />
Syphillus<br />
Warts<br />
Xanthomas<br />
Insect Bites<br />
Milia<br />
Mastocytomas<br />
Contact dermatitis<br />
Erythema<br />
Nodosum<br />
Erythema<br />
Multiforme<br />
VESICU<strong>LAR</strong>/<br />
BULLOUS<br />
Herpes simplex<br />
Varicella<br />
Herpes zoster<br />
Pemphigus<br />
Pemphigoid<br />
Bullous impetigo<br />
Staph Scalded<br />
Skin<br />
Epidermolysis<br />
bullosa<br />
TEN<br />
PUSTU<strong>LAR</strong><br />
Impetigo<br />
Folliculitis<br />
Carbuncle<br />
Hiradenitis<br />
Suppurati<br />
Gonococcal<br />
dermatitis<br />
PETECHIAL<br />
RASH/<br />
PURPURIC<br />
RASH<br />
Vascular Integrity<br />
-Trauma: NAT,<br />
etc<br />
-Vasculitis:<br />
HSP,etc<br />
-Drugs<br />
-Infections: viral,<br />
mono, ricketsia,<br />
strep, endocarditis<br />
Platelet disorder<br />
-ITP<br />
-TTP<br />
-HUS<br />
-SEPSIS/DIC<br />
-<br />
Meningococcus,et<br />
c<br />
-Drug induced<br />
-BM infiltration<br />
-Liver failure<br />
-Congenital plt<br />
d/o<br />
Coagulation<br />
disorder<br />
-Congential:<br />
VWD, hemophilia<br />
A,B<br />
-Acquired: DIC,<br />
warfarin, Vit K<br />
deficient, liver dz,<br />
renal dz
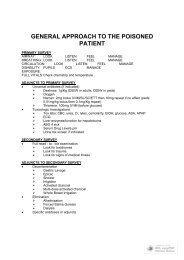
DIFFERENTIAL DIAGNOSIS OF A RASH IN A <strong>TO</strong>XIC PATIENT<br />
Steven’s Johnson syndrome<br />
Staphylococcal toxic shock syndrome<br />
Staphylococcal scalded skin syndrome<br />
Streptococcal toxic shock syndrome<br />
Pemphigus/Pemphigoid<br />
Kawasaki’s syndrome<br />
Vasculitis<br />
Drug reaction<br />
Rocky Mountain Spotted Fever<br />
GENERAL NOTES<br />
Macular = red/pink color change < 0.5cm<br />
Patch = color change > 0.5 cm<br />
Papular = raised lesion<br />
Nodule = round elevated lesion > 0.5cm<br />
Plaque = elevated lesion >0.5 cm<br />
Finish definitions<br />
Approach to diagnosis<br />
Is the person toxic?<br />
Is the rash maculopapular, scaly, papular, nodular, vesicular, bullous, pustular, petechial<br />
or purpuric?<br />
Are there any recongnizable features of the rash or history?<br />
Is the rash acute or chronic?<br />
Is the rash associated with fever or infectious symptoms?<br />
Is the rash localized to an area of contact?<br />
Is the rash scaly?<br />
Common precipitants: drugs, infections, food,<br />
THE <strong>RED</strong> <strong>MACULOPAPU</strong><strong>LAR</strong> RASH +/- SCALES<br />
SCALES, PLAQUES, PATCHES<br />
FUNGAL INFECTIONS<br />
Principles<br />
Dermatophytoses = superficial fungal infections that are limited to skin<br />
Scaling, papules, plaques and patches are most common<br />
Grow best in heat and moistoure<br />
Only grow in keratin or outer layer of skink, nails, hair
Keratin accumulates in body folds<br />
Not very contagious (except Tinea capitis)<br />
KOH preparation: branching hyphae of the dermatophytes or the short, thick hyphae and<br />
clustered spores of tinea versicolor.<br />
Cultures of hair, nail, scales using Saboranund agar X 3 weeks<br />
Tinea Capitis<br />
Clinical Features<br />
Fungal infection of the scalp<br />
MC in preschoolers but increasingly common in adults etc<br />
More common in african americans<br />
Trichophyton tonsurans is cause of current epidemic (many have seborrheic-like scaling in the<br />
abscence of alopecia)<br />
Black dots representing hair broken off near the scalp<br />
Hair loss occurs b/c hyphae grow within the shaft thus the shaft is fragile and breaks off 1-2 mm<br />
from the scalp<br />
Circular patches of baldness may result<br />
Close personal contact spread<br />
Secondary bacterial infection as a complication<br />
Diagnosis and Differential Considerations<br />
Ddx of tinea capitis: alopecia areata, atopic dermatitis, nummular eczema, bacterial infections,<br />
apsoriasis, seborrheic dermaitits, tinea amiantacea, trichotillomania (hair pulling), histiocytosis<br />
KOH prep is not helpful; fungal culture should be obtained<br />
Bacterial culture if you think there is bacterial superinfection<br />
Management<br />
Griseofulvin 20 mg/kg od x 6 weeks (or fluconazole)<br />
Systemic therapy is required<br />
Refer for follow up and family should be evaluated<br />
Selenium sulfide shampooo 250 mg 2x/week decreases shedding<br />
Kerion<br />
Dermatophytic infection of the scalp that appears as an indurated, boggy inflammatory plaque<br />
studded with pustules<br />
Usually mistaken for bacterial infection<br />
Treat with Griseofulvin + prednisone for 2 weeks (decreases inflammation and scarring)<br />
Add keflex or clox if added bacterial infection occurs<br />
Tinea Corporis<br />
Classic “ring-worm” infection<br />
Arms, legs, trunk<br />
Sharply marginated, annular lesion with raised or vesicular margins and central clearing<br />
Single, multiple, or concentric lesions<br />
Tinea cruris:involves the groin, perineum, thighs, buttock (note that the scrotum is<br />
characteristically spared)<br />
Ddx: granuloma annular psoriasis, erythrasma, intertigo with secondary candidiasis<br />
Usually respond to topical therapy alone<br />
Many effective topical antifungal agents: Lotrimin, Tinactin, Micatin, terbinafine, griseofulvin,<br />
naftifine, etc
Apply to affected area tid X 2-3 weeks or until resolution<br />
Acute inflammatory blistering lesions: wet compresses of Burow’s solution: aluminum acetate<br />
solution that is useful for oozing, wet inflammatory lesions\<br />
Tinea Pedis<br />
Athlete’s foot<br />
Scaling, maceration, vesiculation, fissuring between the toes and on the plantar surface of the<br />
foot<br />
Entire sole may be involved<br />
Secondary bacterial infections can occur<br />
Vesicular pustular form of tinea pedis should be considered with vesicles or pustules on inner<br />
aspect of foot<br />
Ddx: contact dermatitis and dyshidrotic eczema<br />
KOH prep helps differentiate<br />
Treatment: topical antifungal preparation until cleared (see above)<br />
Tinea Versicolor<br />
Superficial yeast infection caused by Pityrosporum ovale<br />
Superficial scaling patches occur mainly on the chest and trunk but may extend to the head and<br />
limbs<br />
Lesions are colorful: pink, tan, white<br />
May be itchy; patient may complain that the spots won’t tan<br />
Fine subtle scale is noted that may appear hypopigmented<br />
Pale yellow or orange florescence with Wood’s light<br />
Ddx: vitiligo, seborrheic dermatitis<br />
KOH prep: short hyphae mixed with spores (spagetti and meatballs)<br />
Mx: 2.5% selenium sulfide shampoo, imidazole creams or oral ketoconazole as a singel 400 mg<br />
dose or 200 mg po od X 5 days<br />
Recurrence rates are 30%<br />
Monthly prophylaxsis with selenium shampoos<br />
Tinea Unguium<br />
Fungal nail infection = opaque, thickened, cracked, crumbled nails<br />
Subungual debris; nail may have longitudingal yellow streaks<br />
Nail of great toe is MC location<br />
Mx: topical therapy rarely effective: Fluconazole, itraconazole, terbinafine are all acceptable<br />
options<br />
Recurrence common, may require nail removal<br />
CANDIDIASIS<br />
Perspective<br />
Infections more common in young, elderly, immunocompromised, diabetics, chronic steriods,<br />
endocrine disorders, cancers, antibiotics<br />
Oral Thrush
MC candidal infection<br />
MC in newborns<br />
Patches of white gray friable material covering an erythematous base on the buccal mucosa,<br />
gingiva, tongue, palate, or tonsils<br />
Fissures or crust at the corners of the mouth may be present<br />
AIDS defining illness<br />
Consider immunosuppression in abscence of abx use or dentures<br />
Dx is lichen planus (not easily scraped off as candida is)<br />
Mx<br />
Oral nystatin suspension (100,000 units/ml) qid<br />
Infants: 1ml painting the mouth qid<br />
Older children and adults: 4-6ml swish and swallow qid<br />
Treat for 7/7 or until lesions dissapear<br />
Clotrimazole troches dissolved in the mouth qid is an option in adults<br />
Oral ketoconazole or fluconazole is an option (some think this is the way to go)<br />
Soak dentures in sodium hypochlorite 1:10 solution at night<br />
Cutaneous Candidiasis<br />
Moist, warm areas of groin, axilla, folds, etc<br />
Moist lesions, bright-red macules rimmed witha collarette of scale which represents the pustule<br />
roof with scalloped borders<br />
Small satellite papules or pustules are just peripheral to the main rash<br />
Satellite lesions are the most typical indicators of candidiasis<br />
Intertirginous lesions prone to bacterial superinfection<br />
Candidal onychia and paronychia: hands frequently in hot water, thumb sucking<br />
Ddx: contact dermatitis, tinea cruris, intertrigo, malaria, folliculitis<br />
Candiasis: less sharply demarcated than tinea cruris and brighter red than intertrigo<br />
KOH prep from pustule and roof of the lesion will reveal hyphae and pseudohyphae<br />
Mx<br />
Clean mucky areas and expose to air (fan etc)<br />
Wet compresses with Burow’s solution for inflammatory lesion<br />
Imidazole cream to affected area qid (ketoconaloze, clotrimazole, miconazloe, econazole)<br />
Candidal paryonychia: protect hands from water, nystatin or clotrimazole cream to nail for for 8<br />
weeks<br />
PITYRIASIS ROSEA<br />
Mild skin eruption predominantly found in children and young adults<br />
Lesions are pink or pigmented oval papules or plaques 1-2 cm<br />
Primarily on the trunk and proximal extremities<br />
Mild scaling may be present<br />
Lesions are parallel to the ribs, form ing a Christmas tree-like distribution on the trunk<br />
Oral lesions are rare<br />
Papular or vesicular lesion variants occur in kids<br />
Herald Patch preceeds generalized eruption by one week in 50%
Herald Patch is a large 2-6cm patch<br />
Usually asymptomatic but may be mildly pruritic<br />
Self limited, resolves w/i weeks<br />
Viral cause suspected<br />
Ddx: tinea corporis, guttate psoriasis, lichen planus, drug eruption, secondary syphillus<br />
Recurrence rate<br />
Treatment only symptomatic for pruritis if present<br />
Eczema = dermatitis (constellation of disorders that include erythema, edema, vesiculation,<br />
scaling, pruritis)<br />
A<strong>TO</strong>PIC DERMATITIS<br />
Principles<br />
Cutaneous manifestation of atopic state<br />
Not an allergic disorder in itself<br />
Is associated with allergic disorders: asthma, allergic rhinitis<br />
Abnormalities of humoral and cell-mediated immunity<br />
Eosinophils, mast cells, and lymphocyte activation triggered by increased production of<br />
interleukin 4 by T-helper cells seems to be involved<br />
Increased IgE levels found in most but not all and levels do not correlate<br />
Course is remissions and exacerbations<br />
Clinical Features<br />
Inflammatory, thickened, papular or paulovesicluar lichenification<br />
May show hyperpigmentation of the skin<br />
Skin is typically dry and may be scaly<br />
Skin also can be vesicular, wet, weeping, oozing in the acute phase<br />
Infants: cheeks, extensor surfaces, diaper area<br />
Older children: antecubital and popliteal flexion areas, neck/face/chest<br />
Infantile atopic dermatitis usually begins at 4-6 months and imporves by 4-6yrs<br />
Childhood form: begins at a4-6 years and resolves or continues into adulthood<br />
INTENSE PRURTITIS is the hallmark of atopic dermatitis<br />
Itching can be focal or generalized, worse in the winter, triggered by increased body temp and<br />
stress, worse at night, excoriations common from scratching<br />
Secondary bacterial infection is common<br />
Repeat scratching and rubbing leads to lichenification (hyperpigmented, thick skin with<br />
accentuation of skin furrows)<br />
Differential Considerations<br />
Ddx: histiocytosis X, wiskott-aldrich syndrome, chronic seborrheic dermatitis, phenylkeotonuria,<br />
bruton’s x-linked agammaglobulinemias, psoriasis, scabies, drug eruption, contact dermatitis<br />
Complications: bacterial infection, otitis externa, cataracts, keratoconus, retinal detachment,<br />
cutaneous viral infections
Management<br />
Goals: control inflammation, dryness, itching<br />
Vaseline or Eucerin cream 10% (not lotion) to reduce dryness<br />
Exudative areas: apply wet dressing of gauze soaked in Burow’s solution; apply for 20 minutes<br />
qid<br />
Antihistamines<br />
Systemic steroids for very severe<br />
Cyclosporin, Ultraviolet B treatment, and other immunosuppressive are options for very severe<br />
disease<br />
Topical corticosteroids ointments are mainstay of treatment<br />
Mild disease: less concentrated ointment<br />
Face: triamcinolone 0.025% (milder) used b/c strong steroids can cause permanent cutaneous<br />
atrophy on the face<br />
Severe disease: florinated corticosteroid ointment (1/2 strength betamethasone valerate) to<br />
affected areas tid<br />
FIRST LINE TREATMENTS OF ECZEMA<br />
Antihistamines: gravol, benadryl, atarax<br />
Aveeno baths<br />
Bactroban ointment<br />
Celestoderm<br />
George’s cream<br />
Oatmeal baths<br />
Corticosteroid ointments<br />
SECOND LINE THERAPIES<br />
Protopic (Tacrolimus)<br />
Cyclosporine<br />
Prednisone<br />
Oral antibiotics<br />
<strong>RED</strong> MACULES<br />
DRUG ERUPTION<br />
Principles<br />
Different eruption of same drug in different individuals<br />
MC eruptions are urticarial and morbilliform rashes<br />
Tend to appear within a week after drug is taken (not necessarily right away)<br />
Reactions to semisynthetic penicillins tends to occur later<br />
May appear after drug has been discontinued<br />
Atopic patients with asthma, hay fever, eczema are at increased risk<br />
RARELY produce reactions: acetaminophen, codeine, digoxin, erythromycin, demerol,<br />
morphine, prednisone, maalox<br />
Clinical Features (see table 114-2)<br />
Exanthems: resemble viral and bacterial infections, usually widespread symmetric<br />
maculopapular eruptions
Eczematous drug rashes: resemble contact dermatitis but are more extensive; begin as<br />
erythematous or papular eruptions and become vesicular; prior sensitization is common with this<br />
type of reaction<br />
Vasculitis lesions: begin as erythematous papules or nodules but may ulcerate and become<br />
gangrenous. Purpuric drug eruptions may be the result of bone marrow supression, vasculitis, or<br />
platelet destruction. Platelet transfusion, plasmapharesis, steroids, splenectomy in severe cases<br />
Photosensitive druge reactions: require sunlight<br />
Phototoxic: more common; sulfa drugs/thiazides/tetracycline are common causes, not<br />
immunologic and can occur in any person; look like a sunburn but may have bullous or papular<br />
features; pruritis is minimal or absent<br />
Photoallergic: the result of antigen formation that results in sensitized lymphocytes (delayed<br />
immunoloci response); only occurs in sensitized individuals, usually 2 weeks after exposure to<br />
the drug and sunlight; not dose related, usually look eczematous and is intensely pruritic;<br />
chlorpromazine/promethazine/chlordiazepoxide are common sensitizers of photoallergic<br />
reactions; d/c drug and avoid sunlight/use sunscreen<br />
Fixed drug eruptions: appear and recur at the same anatomic site after repeateed<br />
exposures; sharply marginated and round/oval; may be pigmented, erythematous, or violaceous;<br />
may be pruritic<br />
Ddx<br />
Viral examthem, chronic exfoliative erythroderma: caused by psoriasis or eczema, sScarlet fever,<br />
Staphylococcal scarliatiniform eruption, Kawasaki’s syndrome<br />
Management<br />
D/c drug<br />
Warn that resolution will be slow<br />
Calamine lotion, cool compresses, tepid water baths with colloidal oatmeal (Aveeno) or<br />
cornstarch, antihistamines<br />
STAPHLOCOCCAL SCALDED SKIN<br />
Generally occurs in children < 6yo<br />
Erythema and crusting around the mouth<br />
Erythema then spreads to the body<br />
Bullae form and the skin desquamates<br />
Also called Stapylococcal Epidermal necrolysis<br />
Exfoliative toxin produced by phage groupt II, type 71 Stapylococci<br />
Toxin acts at the zona granulosa of skin to produce a superficial separation that results in<br />
widespread painful erythema, blisters<br />
Usually occurs in children 6 mo to 6 yrs<br />
Mortality 3% in kids but 50% in aldults and near 100% in adults with comorbidities<br />
Mucous membranes SPRA<strong>RED</strong> (can have mild inflammation but not involved to the extent of<br />
Toxic Epidermal Necrolysis)<br />
Nikolski’s sign = the easy separation of the outer portion of the epidermis form the basal layer<br />
when pressure is exerted; often but not always present<br />
Vesicles and bullae are characteristic<br />
Loss of large sheet of superficial epidermis ----> Looks like SCALDED SKIN
Main ddx is Toxic Epidermal Necrolysis (TEN): usually cause by medications, mucous<br />
membranes are INVOLVED<br />
Dx can be confirmed by biopsy or frozen section demonstrating subglandular epithelial<br />
separation<br />
Lesions dry up after desquamation and resolution within 7 days<br />
Mx<br />
Most group 2 are penicillinase resistant<br />
Most recover without abx<br />
Naficillin, cloxacillin, dicloxacillin recomended<br />
<strong>TO</strong>XIC SHOCK SYNDROMES<br />
TSS = acute febrile illness characterized by diffuse desquamating erythroderma<br />
High fever, hypotension, constitutional symptoms, MSOF, rash<br />
Exotoxin-procuding S.aureus<br />
Post op setting is most common outside of tampon related<br />
Also associated with various staph/strep infections: cellulitis, erisepalis, PTA, sinusitis, burns,<br />
septic abortion, skin abscesses<br />
Stapylococcal and Streptococcal toxic shock syndromes<br />
STAPHYLOCOCCAL <strong>TO</strong>XIC SHOCK SYNDROME<br />
Perspective<br />
Often occurs in females related to tampons<br />
Incidence has decreased remarkable since high - absorbent tampons sere withdrawn from the<br />
market<br />
Now most cases related to focal soft tissue infections with staph<br />
Pathophys and Clinical Features<br />
Staph aureus isolated in 90% of cases related to tampons<br />
Results from <strong>TO</strong>XIN FROM PHAGE GROUP 1 S. aureus<br />
Fever, “sunburn” or sandpaper rash, hypotension, tackycardia and at least three organ system<br />
involvement<br />
Mucosal inflammation, myalgia, profuse watery diarrhea, mental status changes are common<br />
Differential diagnosis: streptococcal scarlet fever, stretococcal toxic shock syndrome, rocky<br />
mountain spotted fever, kawasaki syndrome, leptospirosis<br />
Managment<br />
Fluid resuscitation<br />
Vasopressors/ionotropes: need alpha and beta adrenergics<br />
IV antibiotics to cover penicillinase-producing staph: clox, naficillin, etc<br />
Clindamycin and vancomycin options for pen allergic<br />
Remove tampon<br />
Remove foreign bodies<br />
Drain abscesses<br />
Systemic steroids if given early may help<br />
CRITERIA FOR DIAGNOSIS (SSSTT)<br />
Skin Rash (diffuse macular erythema): sunburn or sandpaper looking –> resembles scarlet fever<br />
Skin Desquamation 1-2 weeks after onset<br />
SBP < 90 or orthostatic drop + symptoms<br />
Temp > 38.9<br />
Three organ systems (clinical or lab)
GI: N/V/D<br />
MSK: myalgias, CK doubled<br />
Mucous membranes: vaginal, oral, conjunctival<br />
Renal: BUN or Scr doubled or pyuria > 5 cells/hpf<br />
Hepatic: bili , AST/ALT doubled<br />
Hem: platelets < 100<br />
Neuro: altered LOC with no focality<br />
STREP<strong>TO</strong>COCCAL <strong>TO</strong>XIC SHOCK SYNDROME (STSS)<br />
Perspective<br />
Described in 1987<br />
Predominantly caused by group A strains but can be caused by other groups<br />
Pathophysiology and Clinical features<br />
Predisposing factors: surgery, minor trauma, hematomas, muscle strain,m cellulitis, chicken pox;<br />
Mortality 30%<br />
MOST common cause in children is strep superinfection of chicken pos lesion<br />
Association with NSAID use which may mask presenting symptoms resulting in increased<br />
severity of disease<br />
Severe pain, abrupt onset<br />
Pain often present before physical findings<br />
Usually in extremities but may be pelvic, abdominal, chest, etc<br />
Minority have influenza like symptoms<br />
FEVER is the most common sign (can be hypothermic if sick)<br />
Tachycardia, hypotnesion, soft tissue infection signs, scarlet - fever like rash (sandpaper) are all<br />
common<br />
Renal failure, respiratory failure, DIC, MSOF, shock (septic and cardiogenic from cardiotoxic<br />
effects) are all complications<br />
NOTE: shock is predominantly cardiogenic: LOW CO and high SVR<br />
Streptococcal M and T serotypes<br />
Due to exotoxin A and B: toxins act as superantigens to activate T cells resulting in MASSIVE<br />
release of inflammatory mediators; fever, rash, hypotension, and MSOF<br />
Ddx: staph toxic shock, grm -ve sepsis, endotoxic shock<br />
Diagnosis<br />
Scr increase; Consider deeper infection if CK up<br />
Labs may show DIC; Blood cultures positive in 60%; Wound cultures positive in 95%<br />
DIAGNOSTIC CRITERIA (must meet both)<br />
Isolation of Group A strep<br />
From a normally sterile site (blood, CSF) is a definitive case<br />
From a normally non-sterile (sputum, skin) is a probable case<br />
Hypotension + at least two of....<br />
Renal failure<br />
Coagulopathy<br />
Liver involvement
ARDS<br />
Generalized macular rash (may desquamate)<br />
Soft tissue necrosis<br />
Management<br />
Supportive, usually ICU<br />
Initial abx needs to cover staph and strep b/c hard to distinguish<br />
Penicillin + clindamycin<br />
Ceftriaxone + clindamycin<br />
Penicillin not great against a large inoculum with nec. fasc.<br />
Clindamycin advantages: not effected by large inoculum, kills cell wall-deficient streptococci,<br />
long post administration efficacy, enhances opsonization of streptococcal organisms when grown<br />
with low concentrations of penicillin<br />
Surgical consult for early surgical debridement<br />
IV gamma globulin may help: has antibodies against staphylococcal toxins which may cross<br />
react with streptococcal toxins<br />
Steroids: case reports indicate there may be benefit of dexamethasone if given with gamma<br />
globulin<br />
Antibiotic prophylaxis NOT recommended for household contacts<br />
<strong>TO</strong>XIC EPIDERMAL NECROLYSIS<br />
Principles<br />
Non-staphylococcal induced toxic epidermal necrolysis<br />
Hallmark = separation of large sheets of epidermis from underlying dermis<br />
Full thickness of epidermis is involved<br />
Skin biopsy easily distinguishes b/w TEN and staphylococcal scalded skin<br />
Moratility 20%<br />
Rarely associated with vaccinations (polio, measles, smallpox, td)<br />
Drugs<br />
Penicillin<br />
Sulpha<br />
Tegretol<br />
NSAIDs<br />
Allopurinol<br />
Barbituates<br />
Clinical Features<br />
Mucosal lesion common; may precede exanthem<br />
Nikolski’s sign: rubbing results in desquamation of underlying skin including the pigment (staph<br />
scalded skin ----> pigment remains)<br />
Onset: face and mucous membranes<br />
Ocular involvement can occur<br />
Erythema usually precedes the loosening of the epidermis<br />
Management<br />
D/c drug<br />
Fluid replacement as per burn<br />
Control infection<br />
Steroids controversial
Plasmapharesis experimental<br />
MAINSTAY of managment is wound care and prevention of secondary bacterial infection ------><br />
should be managed in burn center<br />
ERYTHEMA MULTIFORME<br />
Etiology<br />
Drugs and HSV infections are the MCC<br />
Viral infections (heptitis, influenza) are next MCC<br />
Fungal infections: dermatophytosis, histoplasmosis, cocidiomyocosis<br />
Bacterial infections: strep and TB<br />
Collagen vascular disorders: RA, SLE, dermatomyositis, PAN<br />
Cancers<br />
Pregnancy<br />
DDX<br />
Urticaria<br />
Scalded skin syndrome<br />
Pemphigus<br />
Pemphigoid<br />
Viral exanthems<br />
Clinical Features<br />
Acute, self-limiting disease<br />
Erythematous or violaceous macules, papules, vesicles, or bullae<br />
Symmetrical distribution common<br />
Most common in PALMS and SOLES, back of hands or feet, extensor surfaces of the extremities<br />
Target Lesion with three zones of color is the hallmark: centra dark papule or vesicle, surrounded<br />
by a pale zone, a halo of erythema<br />
Steven - Johnson Syndrome = Toxic Exctodermal Necrolysis<br />
Severe form of EM<br />
Bullae, mucous membrane lesions, MSOF<br />
Chills, malaise, headache, fever, tachycardia, hypotension<br />
Purulent conjunctivitis may occur and be severe<br />
Management<br />
Look for underlying etiology<br />
Resolve spontaneously in 2-3 weeks in mild forms<br />
Severe cases: admit, iv hydration, burn unit care, systemic analgesia, systemic corticosteroids<br />
Wet compresses with dressing soaked in 1:16000 solution of potassium permanganate or 0.05%<br />
silver nitrate several times a day to bullous lesions<br />
Look for infection and hypovolemia<br />
URTICARIA<br />
Principles<br />
20% will eventually get urticaria<br />
Acute and chronic forms<br />
Chronic urticaria more common in women<br />
Histamine, bradykinin, kallikrein, acethycholine as mediatesors<br />
Immunologic reaction: anaphylaxis, serum sickness<br />
Nonimmunologic reaction: degranulation of mast cell by foods, drugs
Contact urticari: foods, textiles, animal dander and saliva, plants, topical medications, cosmetics,<br />
chemical<br />
Any drug can cause urticaria: penicillin and aspirin are most common<br />
Any food can cause urticaria: food allergy (fish, nuts, eggs) or non-immunologic histamine<br />
release (holbster, strawberries)<br />
Hereditary urticaria and angioneurotic edema exist<br />
Infections: common cause in children, less common in adults; hepatitis, mono, coxsackie more<br />
commonly produce urticaria<br />
Inhalation: pollens, mold, animal dander, dust, plant materials<br />
Stings and bites<br />
Other associations: SLE, lymphoma, carcinoma, rheumatic fever, hyperthyroid, JRA<br />
Dermatographism: urticarial wheal within 30 minutes after pressure<br />
Pressure urticaria: urticarial wheal forms 4-8 hours after pressure<br />
Cold urticaria: familial or acquired; associated with cryoglobulinemai, cryofibrogenemia,<br />
syphillus, connective tissue disorders: suppression with cyproheptadine 4mg tid, antihistamines<br />
before cold exposure; doxepin qhs<br />
Cholinergic urticaria: induced by heat, exercise, or stress; wheals of 1-2 mm surrounded by<br />
erythematous flares and occassionally satellite wheals; responds to hydroxyzine<br />
Heat and solar urticaria uncommon<br />
Chronic urticaria etiology often unknown<br />
DDX OF URTICARIA<br />
F Foods<br />
P Plants<br />
A Animals<br />
D Drugs<br />
I Infections<br />
C Contacts (cosmetics,etc)<br />
O Other:cold, cholinergic, chronic<br />
P Physical: dermatograph, pressure<br />
Clinical Features<br />
Edematous plaques with pale centers and red borders<br />
Individual hives are transient (lasting < 24hrs)<br />
New hives may continually develop<br />
Ddx: erythema multiforme, erythema marginatum (R.F.), erythema migrans (Lyme dz), JRA<br />
Management<br />
Remove inciting factor if possible<br />
H1 antagonists: benadryl, gravol, Hydroxyzine (Atarax, Vistaril): 10 - 25 mg (2 mg/kg/24hr in<br />
kids); supposed to be less sedating than benadryl, gravol<br />
H2 antagonists: actually good for skin, ranitidine/cimetidine<br />
Fexofenadine, astemizole, terfenadine are supposed to be even less sedating<br />
Prednisone X few days: effective utricaria can rebound after discontinuation<br />
When to use prednisone? Failed treatment with antihistamines, severe symptoms, anaphylaxisis
EXANTHEMS<br />
PRINCIPLES OF EXANTHEMS<br />
Exanthem = skin eruption that occurs as a symptom of a generalized disease<br />
Known infectious causes: 30+ enteroviruses (mostly coxsacki and echoviruses) as well as<br />
adenovirus have a particular nack to cause exanthems<br />
Most are maculopapular although scarlatiniform, erythematous, vesicular, and petechial rashes<br />
Usually nonpuritis, do not desquamate, and vary in extent<br />
Mucous membrane lesions may occur<br />
Echovirus type 9: meningitis, petechial exanthem resembling meningococcemia<br />
Echovirus type 16 (Boston exanthem): may resemble roseola<br />
Coxsackie group B type 5 may also resemble roseola in adults<br />
Coxsackie group A type 16: distinctive syndrome of vesicular stomatitis, oral vesicles, dorsum of<br />
hands and lateral borders of feet; may be associated with meningoencephalitis<br />
Classic viral exanthems<br />
Roseola Infantum = Exanthem subitum (HHV6)<br />
Rubella (German measles)<br />
Rubeola (measles)<br />
Erythema infectiosum = fifth disease (parvovirus B19)<br />
Enteroviruses: coxsackie, echo<br />
MEASLES (RUBEOLA)<br />
Clinical Features<br />
Highly contagious virus; droplet spread; incubation 10 days<br />
Now usually only seen in nonimmunized, immigrants<br />
Contagious from 2 days before symptoms until 4 days after rash appears<br />
Fever, malaise mark onset of symptoms; coryza, conjunctivitis, and cough begin within 24hours<br />
of the onset of symptoms<br />
Fever increases daily in a stepwise fashion until it reaches approximately 40.5 degrees celcius on<br />
the 4th - 5th day<br />
Koplick’s spots are pathognomonic: small, irregular, bright red spots with bluish-white centers<br />
that begin opposite the molars then spread to the adjacent oropharynx; usually appear on second<br />
day of illness<br />
Cutaneous eruption begins on th 3rd - 5th day of illness (rash BEFORE defervescence)<br />
Maculopapular erythematous lesions involve the forehead and upper neck then spread to the<br />
face, trunk, arms, and finally the feet (SPREADS <strong>TO</strong>P DOWN)<br />
Koplick’s spots disappear as the rash appears<br />
The rash begins to fade in the order of appearance (starts on 3rd day)<br />
Complications: OM (most common), encephalitis (1 in 1000), pneumonitis<br />
Management<br />
Antibiotics indicated for bacterial superinfections (OM, etc) only<br />
Supportive treatment only<br />
Isolation of limited value b/c not infectious by the time it is diagnosed<br />
Human immune globulin in a susceptible person within 6 days of exposure (0.25 ml/kg IM in<br />
children).<br />
Live virus vaccine given w/i 72 hrs of exposure may be effective in prevention<br />
Vitamin A shortly after exposures??<br />
? indications for immune globulin
ROSEOLA INFANTUM = EXANTHEM SUBITUM = SIXTH DISEASE<br />
Caused by Human Herpes Virus 6<br />
Fever and skin eruption<br />
95% occur in 6mo to 3yrs and most are < 2yo<br />
Febrile seizures may occur<br />
Abrupt onset fever, rising rapidly to 40 degreees<br />
Temperature continues for 3-4 days (constant or fluctuant) then rapidly decreases to normal<br />
Rash appears with defervescence<br />
Pink or rose colored macules or maculopapules 2-3 mm diameter which blanch on pressure and<br />
rarely coalesce; trunk initially the SPREAD PERIPHERALLY to neck and extremities<br />
Rash clears over 1-2 days without desquamation<br />
LOOKS WELL despite high fever<br />
Encephalitis rare, very few complications<br />
Excellent prognosis, no treatment<br />
RUBELLA = GERMAN MEASLES<br />
Fever, skin eruption, generalized lymphadenopathy<br />
Spread by droplet contact; peak in winter and spring<br />
Incubation 14 - 21 days: contagious few days before rash and 7 days after onset<br />
Infants with congenital exposures can shed virus for more than a year<br />
Adults: 1-6 day viral prodrome, symptoms dissapear w/i 24 hours after rash develops<br />
Pink to red maculopapules; first on face then spreads rapidly DOWN to the trunk and extremities<br />
Lesions on the trunk tend to coalesce but those on extremities do not<br />
Rash remains for 1-5 days classically disappearing on the 3rd day<br />
Clearing may be accompanied by fine desquamation but usually not<br />
Lymphadenopathy begins days before the rash: suboccipital, postauricular, posterior cervical<br />
No specific treatment<br />
Complications<br />
Encephalitis<br />
Thrombocytopenia<br />
Arthritis<br />
Congential Defects<br />
24% of infected fetuses have a congenital defect<br />
Maternal infection may be determined by serology: acute and convalescent increase in titers 4<br />
fold is diagnostic<br />
Routine use of PEP in an unvaccinated women in early pregnancy is not recommended<br />
ERYTEHMA INFECTIOUSUM = FIFTH DISEASE = SLAPPED-CHEEK RASH<br />
Parvovirus B19 infection<br />
Mild systemic symptoms, fever in 15%, characteristic rash<br />
Arthralgias and arthritis common in adults, rare in kids<br />
Slapped - cheek rash b/c of intensely red face with circumoral pallor<br />
Maculopapular lacelike rash in the arms, trunk, buttocks, and thighs<br />
Rash may recur with temperature changes
Incubation is 4 - 14 days<br />
Parvovirus: may also cause URTI, atypical rash, arthritis without rash<br />
Hepatitis can occur (rare)<br />
Aplastic crisis associated with parvoB19 and hemolytic anemias an sickle cell dz<br />
Pregnancy infection: fetal hydrops and death<br />
No treatment<br />
SCARLET FEVER<br />
Clinical Features<br />
Recent decline in incidence<br />
Abrupt onset with fevers, chills, malaise, sore throat followed within 12-48hrs of distinctive rash:<br />
begins on chest and spreasds rapidly<br />
Circumoral pallor, sandpaper-like texture b/c of the rough feel of the skin due to the multitude of<br />
pinhead size lesion<br />
Pharyngitis +/- erythematous or petechial lesions on the palate<br />
After resolution of the symptoms, desquamation of the inovlved areas is characteristic<br />
Complications: abscess, OM, pneumonia, rheumatic fever, post strep GN<br />
Management<br />
Antistrep abx: penicillin V 50 mg/kg/day dividied qid in kids<br />
Pen V 250 po qid in adults<br />
Benathine IM injection X 1 is an option<br />
Erythromycin 250 mg (or 40 mg/kg) po qid if pen allergic X 10 days<br />
Need full 10 days b/c only literature to show prevention of rheumatic fever is with a 10 day<br />
course<br />
KAWASAKI DISEASE<br />
Acute vasculitis primarily of infants and children<br />
Previously named Mucocutaneous lymph node syndrome<br />
Peak incidence in spring and winter<br />
Majority occur < 5 yo; 1-2 yo is most common; RARE in adults<br />
Etiology unknown<br />
Immune system activation wth vascular injury as the result<br />
Myocarditis is the most common cause of death<br />
Fever, conjunctivits, rash, mucous membrane lesions, extremity changes, cervical<br />
lymphadenopathy<br />
Cervical adenopathy: 50%, may be presenting feature<br />
Fever: high, spiking, persistent for 1-3 weeks<br />
Conjunctivitis: bilateral, bulbar > palpebral, no exudate, mild uveitis<br />
Mucous membrane lesions: injected or fissured lips, injected pharynx, or strawberry tongue, no<br />
ulcerations<br />
Extremity changes: painful, erythematous, swollen hands and feet (may not be able to walk, may<br />
present with limp); desquamation of finger and toes begins 10-20 days after fever; Beau’s lines<br />
are transverse grooves of the nail months after fever<br />
Rash: highly variable, appears within 5 days of fever, generally a maculopapular rash that may<br />
look like scarlet fever, urticaria, erythema multiforme, or morbiliform rash; may have small<br />
vesicles but no pustules or bullae
Arthritis common<br />
MCC of pediatric acquired heart dz: coronary artery aneurysms, coronary vasculitis, myocarditis,<br />
pericarditis, CHF, pericardial effusions, valve dz, arrtyhmias<br />
Coronary aneurysms: 20%; prone to MI or coronary rupture and tamponade; treatment with<br />
IVIG and high dose aspirin decreases incidence of coronary aneurysms to 3-5%<br />
Natural History<br />
Phase I: acute phase (1-2wks); fever, myocarditis, pericaridal effusions, other diagnostic signs<br />
Phase II: subacute phase (1-4 wks): fever/rahs/lymph nodes resolve and conjucntivitis persist;<br />
desquamation/arthritis/myocardial dysfunction occurs; highest risk of death<br />
Phase III: convalescent phase; clinical findings resolve, continues until ESR is normal 6-8 weeks<br />
after onset<br />
CDC Diagnostic Criteria = Unexplained fever for 5 days + 4/5 criteria<br />
C - Conjunctivitis: bilateral w/o exudate<br />
R - Rash<br />
E - Extremity changes (red, swollen, desquamating)<br />
A - Adenopathy (cervical ln, at least one > 1.5 cm)<br />
M - Mucous membrane lesions (injected lips/pharynx, tongue)<br />
Atypical Kawasaki’s<br />
Cases that don’t meet the CDC case definition<br />
More common in those < 6 months were diagnosis is more difficult<br />
Investigations<br />
Admit for echo<br />
Do ECG<br />
May need coronary angiogram<br />
CBC, lytes, creatinine, ESR, CXR, blood culture, urinalysis, ASOT titer, throat swab, LP if signs<br />
of aseptic meningitis<br />
Differential Diagnosis<br />
Rash: measles, toxic shock syndrome, Stevens-Johnson, RMSF, JRA, drug reaction, viral<br />
exanthem, scarlet fever<br />
H/N manifestations: RP abscess, GAS pharynitis, Mono<br />
Measles: severe cough, Koplik’s spots<br />
Managment<br />
IV gamaglobulin: 2 g/kg over 12 hours (may need further treatments)<br />
High dose ASA: 100 mg/kg/day divided into q6hr dosing<br />
Therapy decreases incidence of coronary aneurysm<br />
ROCKYMOUNTAIN SPOTTED FEVER<br />
Rickettsia rickettsii<br />
Transmitted to humans through tick bites (saliva at time of bite)<br />
Reported in North, South, and central america<br />
Most cases reported form SOUTHEASTERN USA<br />
Clinical Features<br />
Abrupt onset of headache, N/V, chills, fever to 40 degrees<br />
Ocassionally onset is more gradual with anorexia, malaise, fever<br />
May be prolonged (3 weeks)
May be severe (CNS, cardiac, pulomonary, GI, renal complications)<br />
Rash develops on 2nd - 4th day<br />
Erythemaous macules that blanch on pressure, appearing first on wrists and ankles then<br />
spreading up the extremities to the face and trunk w/i hours<br />
Lesions may become petechial or hemorrhagic<br />
Lesions on the palms and soles are particularly characteristic<br />
Increased capillary fragility and splenomegaly may be present<br />
Diagnosis<br />
Weil-Felix reaction (serology)<br />
Other immunologic flourescent procedures exist<br />
Treat based on suspicion b/c lab will be slow<br />
Management<br />
Tetracycline 25 mg/kg/day is the antibiotic of choice (po or iv)<br />
Doxycycline and chloramphenicol may be used as options<br />
Usual course is 10 days<br />
Avoid sulpha drugs which can exacerbate the illness<br />
Rickettsiae routinely resistant to penicillins, cephalosporins, aminoglycosides, and erythromycin<br />
PAPU<strong>LAR</strong> AND NODU<strong>LAR</strong> LESIONS<br />
CONTACT DERMATITIS<br />
Non - Allegic Contact Dermatitis<br />
Inflammatory reaction to chemical, physical, or biological agent<br />
Caustics, solvents, detergents cause irritant dermatitis<br />
Allergic contact dermatitis<br />
Delayed hypersensitivity reaction mediated by lymphocytes sensitize by the contact of the<br />
allergen to the skin<br />
Less common than (non-allergic) irritant contact dermatitis<br />
Clothing, jewelry, soaps, cosmetics, plants, medications contain allergens that commonly cause<br />
allergic contact dermatitis<br />
Rubber, poison ivy/oak/sumac (Rhus genus plants), paraphenyldenediamine (hair dyes and<br />
industrial chemicals), ethylenediamine (topical medication ingrediant) are the MCC of allergic<br />
contact dermatitis<br />
Sensitization to poison ivey results in sensitization to other similar plants: cashew, mango,<br />
lacquer, ginkgo trees<br />
Management<br />
Avoid irritant or allergen<br />
Treat secondary bacterial infections<br />
Wet compresses of Burow’s solution for oozing or vesicular lesions (qid)<br />
Topical baths OTC<br />
Prednisone 50 mg po od if severe: taper over 14 days (21 for poison ivy)<br />
Taper of steroid needed to prevent relapse<br />
Antihistamines for pruritits<br />
Wash all clothes to remove offending agent that could be contaminated
DIAPER DERMATITIS<br />
Clinical Features<br />
Occlusive diapers and clothing, heat, moisture, friction, urine and feces all contribute<br />
Tends to SPARE CREASES<br />
Erythematous plaques in the genital, perianal, gluteal, and inguinal areas<br />
May extend elsewhere with more severe cases<br />
May be superinfected with candida: moist, red patches with well demarcated borders and papular<br />
or pustular satellite lesions<br />
May reflect atopic or seborrheic dermatitis in infants (especially if lesions are found elsewhere in<br />
the body)<br />
Management<br />
Remove excess clothing<br />
Remove occlusive diapers<br />
Frequent diaper changes<br />
Leave diapers off long enough to dry area<br />
Sterilized cloth diapers preferred<br />
Exudative lesions: wet compresses with saline or Burow’s solution for 3/7<br />
Zinc oxide (Desitin) may dry the area<br />
Hydrocortisone 1% cream in severe cases<br />
Avoid ointment based topical medications for treatment b/c their occlusive nature enhances<br />
moisture retention (use cream, not ointment)<br />
Nystatin cream or powder if Candida superinfection<br />
ERYTHEMA MULTIFORME<br />
Etiology<br />
Drugs and HSV infections are the MCC<br />
Viral infections (heptitis, influenza) are next MCC<br />
Fungal infections: dermatophytosis, histoplasmosis, cocidiomyocosis<br />
Bacterial infections: strep and TB<br />
Collagen vascular disorders: RA, SLE, dermatomyositis, PAN<br />
Cancers<br />
Pregnancy<br />
DDX<br />
Urticaria<br />
Scalded skin syndrome<br />
Pemphigus<br />
Pemphigoid<br />
Viral exanthems<br />
Clinical Features<br />
Acute, self-limiting disease<br />
Erythematous or violaceous macules, papules, vesicles, or bullae<br />
Symmetrical distribution common<br />
Most common in PALMS and SOLES, back of hands or feet, extensor surfaces of the extremities<br />
Target Lesion with three zones of color is the hallmark: centra dark papule or vesicle, surrounded<br />
by a pale zone, a halo of erythema<br />
Steven - Johnson Syndrome = Toxic Exctodermal Necrolysis<br />
Severe form of EM
Bullae, mucous membrane lesions, MSOF<br />
Chills, malaise, headache, fever, tachycardia, hypotension<br />
Purulent conjunctivitis may occur and be severe<br />
Management<br />
Look for underlying etiology<br />
Resolve spontaneously in 2-3 weeks in mild forms<br />
Severe cases: admit, iv hydration, burn unit care, systemic analgesia, systemic corticosteroids<br />
Wet compresses with dressing soaked in 1:16000 solution of potassium permanganate or 0.05%<br />
silver nitrate several times a day to bullous lesions<br />
Look for infection and hypovolemia<br />
PEDUNCULOSIS<br />
Clinical Features<br />
Nits or adult lice seen on microscopic examination of hair from symptomatic areas: nits are more<br />
common than the aduult louse form<br />
Nits attach tot eh bases of hair shafts looking like white dots<br />
Adult louse look like blue or black grains<br />
Severe itching and scratiching<br />
Secondary infections can occur<br />
Pediculosis corporis: lice live in clothing, bedding and feed on the host; the parasites are usually<br />
absent from the body except in very severe cases; Erythematous macules or wheals may be<br />
present with intense itching: Treatment consists of luandering or boiling the clothes and linen;<br />
may add lindane lotion if nits are found in the hair but this is usually not neccessary<br />
Pediculosis capitits: more common in small children; pruritis is the major sympom and may be<br />
confined to the scalp; excoriations and secondary bacterial<br />
Management<br />
Permetrhin (Nix) is the recommended treatment<br />
Lindand (Kwell) lotion or cream is no longer preferred<br />
Nix remains active for 2 weeks<br />
Avoid shampoos and conditioners for 2 weeks b/c it coats and protects the lice<br />
Nix: shampoo hair, dry, apply Nix, wash out after 10 minutes (MUST be applied when the hair is<br />
dry b/c lice don’t breath for 30 min when immersed in water!); repeat dose one week after initial<br />
use<br />
Treat sexual partners<br />
Treat only symptomatic household members<br />
Wash clothes, sheets, pillow cases in hot water and dry in hot cycle<br />
Ivermectin 200 ug/kg and repeat in 10 days has been shown to eradicate lice<br />
SCABIES<br />
Clinical Features<br />
Mite infestation with severe itching<br />
Interdigital web spaces, flexion area of wrists, axillae, buttocks, lower back, penus, scrotum and<br />
breasts are the most common locations<br />
Infants have a more generalized involvement<br />
Reddish papules/vesicles surrounded by erythematous border and scratch marks<br />
Infants and young children often have generalized skin involvement includine scalp, palms,<br />
soles, face: most common presenting lesions are papules and vesiculopustules
Norwegian scabies: extensive hyperkeratosis and crusting of the hands, feet, and scalp;<br />
immunosuppressed patients; highly contagious<br />
Close personal contact transmission; multiple family members will usually have<br />
Management<br />
Permetrin 5% cream (Elimite) or crotamiton (Eurax) cream<br />
Lindane is no longer the preferred treatment<br />
Elimite: applied overnight once weekly for 2 weeks; cover the entire body (preferred treatment<br />
for infants and small children)<br />
Post scabietic nodules and pruritis may persist for months after sucessful tx<br />
Norwegian scabies requires repeated treatment<br />
Treat all family members and sexual contacts<br />
Wash and dry in hot temperatures the linens and underwear<br />
SYPHILLUS<br />
Clinical Features<br />
Treponema pallidum<br />
Incubation 10 - 90 days<br />
Primary lesion: chancre, usually single lesion, lasts 3-12 weeks and heals spontaneously, appear<br />
at site of inoculation (genitalia or mucous membranes), chancre begins as a papules and<br />
characteristically develops into an ulcer approximately 1cm in diameter with a clean base and<br />
raised borders; painless chancre unless secondary infection; lymphadenopathy<br />
Secondary stage:<br />
6weeks to 6 months with various different lesions<br />
Erythematous or pink macules or papulues, usually with a generalized symmettrical distribution<br />
Pigmented macules and papules classically appear on the palms and soles; may be scaly but<br />
rarely pruritic<br />
Papular, annular, circinate lesions are more common ion nonwhites<br />
Generalized lymphadenopathy and malaise accompany the lesions<br />
Irregular patchy alopecia<br />
Moist, flat, verucous condyloma latum may appear on genitals<br />
Diagnosis<br />
Primary: darkfield microscopy for spirochetes; not available in ED thus suspect and treat based<br />
on clinical suspicion and refer to STD clinic<br />
VDRL not very sensitive or specific in primary syphillus<br />
VDRL is better with secondary syphillus<br />
FTA-ABS serology is better (Florescent Treponema antibody absorption)<br />
Many causes of false +ve VDRLs: vaccines, mono, mycoplasma, etc<br />
Management<br />
Incubating syphillus (before chancre): 1gm of probenecid po then 4.8 million units of procain<br />
penicillin IM<br />
Primary and secondary: benzathine penicillin G 2.4 million units IM<br />
Doxycycline or tetracycline for pen allergic for 14 days<br />
Jarisch-Herxheimer reaction: febrile reaction and diffuse rash 12 hours after receiving treatment<br />
for syphillus, resolves spontaneously in 24hrs
ERYTHEMA NODOSUM<br />
Clinical Features<br />
Inflammation of the dermis and adipose tissue<br />
Painful red to violet nodules<br />
Nodules are elevated skin lesions located deep in the skin thus the overlying skin can be moved<br />
on palpation<br />
MC over anterior tibia but may be on arms or thrunk<br />
Fever and arthralgia of ankles may preceed the rash<br />
Lesions may turn yellow-purple and resemble bruises with evolution<br />
Most common in women in 20 - 50s<br />
Associations<br />
Infections: TB, sterptococci, yersinia, chlamydia, coccidio, histoplasmosis<br />
Sarcoidosis<br />
Ulcerative colitis and regional enteritis<br />
Pregnancy<br />
Idiopathich<br />
Drugs: OCP is the MCC<br />
Management<br />
Treat underlying condition<br />
CXR for ? sarcoidosis or TB should be considered<br />
Bed rest, elevate legs, wear stocking<br />
ASA 600 mg q4hr<br />
Resolves spontaneously in 4-6 weeks<br />
Potassium iodide 360 - 900 mg po od for 3-4 weeks if severe (? May act through an<br />
immunosuppressive mechanism mediated via heparin release from mast cells)<br />
VESICU<strong>LAR</strong> AND BULLOUS LESIONS<br />
PEMPHIGUS VULGARIS<br />
Clinical Features<br />
Vesicles = elevated lesions that contain clear fluid<br />
Bullae = vesicles > 1 cm<br />
Pemphigus vulgaris is an uncommon but severe disorder<br />
Bullous disease most common in 40 - 60yo<br />
Small, flaccid bullae that break easily forming superficial erosions and crusted ulcerations are the<br />
typical lesions<br />
Any area of the body may be involved<br />
Nikolsky’s sign is present<br />
60% have mucous membrane lesions<br />
Oral lesions typically preceed the cutaneous lesions by months<br />
Gums and vermilion borders of lips are particularly common<br />
Oral lesions are bullous but break easily thus superficial ulceration is seen<br />
Cause unkonwn<br />
Has been seen rarely with captopril and penicillamine<br />
Tzanck cytologic test suggest the diagnosis (finding acanthyolytic cells, degenerated rounded<br />
epithelial cells with amorphous nuclei)<br />
Acantholytic cells are not specific for pemphigus<br />
Serum immunofluorescence confirms the diagnosis
Ddx: bullous pemphigoid, epidermolysis, dermatitis herpetiformis, TEN, bullous scabes, bullous<br />
SLE<br />
Management<br />
Pain control<br />
Local wound care<br />
Steroid: 100 - 300 mg prednisone<br />
Consult dermatology<br />
Other immunosuppressants sometimes used<br />
Mortality very high without steroids<br />
Superinfection and complications of steroids are problematic<br />
PEMPHIGOID<br />
HERPES SIMPLEX<br />
HSV 1: primarily nongenital areas<br />
HSV 2: primarily genital areas<br />
Clinical Features<br />
HSV 1 most common in mouth, more common in children<br />
Cluster ov vesicles that appear, break and leave crusted erosions<br />
Can have very severe gingostomatitis with dehydration<br />
Secondary infection with staph and strep can occur<br />
Hallmark = painful group of vesicles on erythematous base<br />
Usually nondermatomal distribution<br />
Avoid contact with atopic dermatitis kids b/c of severe generalized HSV can develop in kids<br />
with atopci eczema and other dermatosis<br />
HSV2: single or grouped vesicles on penis, prodrome of local pain and hypesthesia common,<br />
constitutional symptoms and L.N. common<br />
Versicles erode over few days, become crusted, and heal over 2 weeks<br />
Located to cervix, vagina, or introitus in women<br />
Herpes cervicitis may cause severe pelvic pain in women<br />
Managment<br />
First episode of gential herpes: acyclovir (Zovirax) 200mg po 5X/day X 10/7<br />
Famciclovir or vancyclori are options<br />
Treat until resolution of lesions if not gone by 10 days<br />
Improve healing and decrease spread with treatment but do NOT prevent recurrences (acyclovir<br />
prophylaxis may help suppress herpes)<br />
Acyclovir can be started at first sign of recurrence<br />
Immunocompromised: admit for iv acyclovir<br />
Pain control important<br />
Treat partner<br />
Stomatitis: Maalox and benadryl (?treat primary gingivostomatitis with acyclovir)
VARICELLA<br />
Clinical Features<br />
Chickenpox; Varicella-zoster virus<br />
Incuation 2-3 weeks<br />
Begins with low fever and constitutional sympomts<br />
Exanthe4m conincides with these sympomts in children but follows them in adults by 1-2 days<br />
Lesions rapidly progress from macules to papulues to vesicles to crusting lesion sometimes<br />
within hours; vesicles are 2-3 mm and surrounded by erythematous border (can have larger<br />
bullae)<br />
Drying vesicles produce scabs which fall off in 5-20 days<br />
Highest concentration in trunk<br />
Hallmark = lesions in all stages (macules, papules, vesicles, crusts)<br />
Complications<br />
Bacterial superinfection of lesions<br />
Secondary bacterial pneumonia<br />
Encephalitis<br />
Thrombocytopenia<br />
Arthritis<br />
Hepatitis<br />
Glomerulonephritis<br />
Management<br />
Symptomatic treatment<br />
AVOID ASA (Reye’s syndrome)<br />
Oral acyclovir may be effective if started within 24hours of rash for patients with chronic<br />
respiratory or skin diseases; may decrease duration and symptoms<br />
Isolation usually futile b/c spread before diagnosis: keep at home though becouse spread<br />
continues until all vesicles have crusted over and dried up<br />
Varicella vaccination exists<br />
Maternal varicella 5 days before and 2 days after delivery can result in disseminated herpes in<br />
the newborn<br />
Pregnant women and immunocompromised exposed to chicken pox<br />
Check varicella-zoster titers<br />
VZIG must be given to those with negative titers who are exposed<br />
Congenital anomalies if exposed in first or early second trimester: embryopathy, limb atrophy,<br />
scarring extremities, CNS and ocular manifestations<br />
HERPES ZOSTER<br />
Clinical Features<br />
Shingles is an infection caused by varicella zoster virus<br />
Virus lives in dorsal root ganglion and is reactivated<br />
Pain in dermatome prior to appearance of rash by 1-10 days<br />
Grouped vesicles on erythematous base in dermatomal pattern<br />
Thorax and trigeminal nerves are the MC location<br />
Vesicles appear then b/cm cloudy and progress to crusts and scabs<br />
Crusts fall off at 2-3 weeks<br />
Peak incidence in 50 - 70yo (rare in children)<br />
Associations: leukemia, Hodgkin’s, other cancers (don’t need to hunt for)<br />
You CAN acquire chicken pox from exposure to shingle but uncommon
Can be a disseminated infection<br />
Complications: ocular infection, postherpetic neuralgia, meningoencephalitis, myelitis,<br />
peripheral neuropathy<br />
Ocular: 20 - 70% involve the opthalmic division of trigeminal nerve (V1); can be vision<br />
threatening; anterior uveitis, conjunctivitis, secondary glaucoma, corneal scarring can all occur;<br />
tip of the nose means that the nasociliary nerve is involved and predicts eye involvement<br />
More severe in immunosuppressed especially AIDS, Hodgkin’s, other lymphoma; cutaneous and<br />
CNS dissemination more common in these groups<br />
Postherpetic neuralgia<br />
More common in elderly and immunocompromised<br />
May lasts months to years<br />
Management<br />
Analgesia<br />
Other treatment rarely necessary<br />
Burow’s solution may be applied to hasten drying<br />
Steroids: may shorten duration of postherpetic neuralgia but does not lesson the severity of pain<br />
or affect the rate of healing<br />
Acyclovir, famciclovir, valacyclovir etc: have been shown to be effective for<br />
immunocompromised patients<br />
Capsaicin cream can be used on areas with postherpetic neurlagia\<br />
Severe ocular zoster: iv acyclovir may be of some benefit, topical steroids (is used with zoster; is<br />
NOT used with herpes simplex conjunctivitis)<br />
PUSTU<strong>LAR</strong> LESIONS<br />
IMPETIGO<br />
Principles<br />
Slowly resolving pustular eruption most common in preschool children<br />
Staph aureus is the most common cause currently<br />
Group A strep is the second MCC<br />
Predispositions: eczema, poor hygeine, malnurished, other skin conditions<br />
Clinical Features<br />
Streptococcal impetigo (ECTHYMA)<br />
Most common on the face<br />
Begins as a single pustule but then develops into multiple lesions: 1-2mm vesicles with<br />
erythematous margins; when they break they leave red erosions covered with a golden yellow<br />
crust<br />
Can be pruritic but are not paiful<br />
Regional lymphadenopathy common<br />
Very contagious among infants and children (less in older)<br />
Post strep glomerulonephritis as a complication<br />
Staphlococcal impetigo<br />
Little surrounding erythema compared to strep<br />
Staph is a more superficial infection<br />
Bullous impetigo<br />
Caused by staph phage group 2<br />
Primarily in infants and young children
Initial lesions are thin walled 1-2cm bullae; they rupture to leave a thin serous crust and<br />
collarette-like remnant of the blister roof at the rim of the crust<br />
Face, neck, extremities are most common<br />
Ddx: dermatitis, HSV infection, fungus, pemphigus vulgaris<br />
Gram stain of fluid from bullae: Gram+ve cocii<br />
Management<br />
Systemic and topical antibiotics are equally effective<br />
More extensive lesions should be treated systemically<br />
NO evidence that antibiotics prevent post strep GN<br />
Mupirocin 2% ointment tid<br />
Erythromycin qid X 10/7 or Keflex are options<br />
Bullous impetigo: penicillinase resistant semisynthetic penicillin (dicloxicillin) or erythromycin;<br />
add mupirocin 2% ointment to area as well<br />
FOLLICULITIS<br />
Inflammation of the hair follicle<br />
Usually caused by staph aureus<br />
Lesions are on usually on buttocks, thighs, and occasionally scalp/beard<br />
Ddx: acne, keratosis pilaris, fungal infection<br />
Pseudomonas associated with hot tubs, pools, antibiotic use for acne<br />
Gram stain of lesion can tell pseudomonas from staph<br />
Mx: antiseptic cleaner (chlorhexidine) daily until cleared<br />
Extensive involvement: erythromycin, dicloxacillin may be added<br />
CARBUNCLE<br />
Large abscess that develops in thick inelastic skin of back of neck, back, thighs<br />
Severe pain, fever, sepsis possible<br />
Local heat<br />
I&D when fluctuance present<br />
Abx only necessary if cocomitant cellulitis or sepsi<br />
HIRADENITIS SUPPURATIVA<br />
Apocrine sweat glands<br />
Recurrent abscess formation in axilla and groin resembles furunculosis<br />
Recurrence common; often resistant to therapy<br />
Need to I&D abscesses<br />
Antistaph abx useful if early and long course used<br />
Many require local incision and skin grafting<br />
Antiandrogen therapy is an option in resistant cases<br />
GONOCOCCAL DERMATITIS<br />
Arthritis - dermatitis syndrome<br />
MC presentation of disseminated gonococcal disease<br />
2% of patients with gonnococcus (MC in women)<br />
Fever, migratory polyarthralgias, skin lesions<br />
Multiple lesions with predominance for periarticular regions of distal extremities
Erythematous or hemorrahgic papules that evolve into pustules and vesicles with an<br />
erythematous halo (look like meningococcemia). They are tender and may have a gray necrotic<br />
hemorrhagic center. Healing with crust formation usually occurs w/i 4-5 days<br />
Recurrent crops of lesions can occur even after antibiotics started<br />
Gultures and gram stains of lesions usually negative<br />
Immunofluorescent antibody staining of direct smears from pustules more reliable<br />
Diseminated gonococcal infection<br />
Ceftriaxone 1gm iv/im q24hrs OR cefotaxime 1gm q8hr<br />
Allergic to Blactams: spectinomycin 2 gm im q12hrs<br />
Switch to po cefixime, cefuroxime, cipro, or ofloxacin<br />
Total treatment of 7 days<br />
Hospitalization for septic arthritis, meningitis, endocarditis<br />
PETECHIAL AND PURPURIC LESIONS<br />
INTRODUCTION<br />
Purpura = blood in the skin or mucous membrane; divided into petechiae and echymosis<br />
Petechia = small, golden-brown -> yellow<br />
DIFFERENTIAL DIAGNOSIS OF PURPURIC RASH<br />
VASCU<strong>LAR</strong> INTEGRITY PROBLEM<br />
Trauma: normal and Non-Accidental trauma must be thought of<br />
Infections: meningococcus, viral NOS, mono, endocarditis, ricketssia, strep<br />
Drugs<br />
HSP and other vasculitidies (kawasaki’s, serum sickness, cryoglobulinemia, vasculitis with<br />
SLE/lyme/IVDA/PBC)<br />
Vit C deficient<br />
Ehlers-danlos etc<br />
PLATELET PROBLEM<br />
Thrombocytopenia<br />
Decreased production<br />
Sepsis: esp meningococcus<br />
Drug suppression<br />
Aplastic anemia<br />
BM infiltration<br />
Increased destruction<br />
Sepsis/DIC<br />
Drug<br />
HUS<br />
TTP<br />
ITP<br />
Increased sequestration<br />
Liver dz
Splenomegaly<br />
Platelet Dysfunction<br />
Chronic renal failure, aspirin and other drugs<br />
Congenital platelet disorders<br />
COAGULATION FAC<strong>TO</strong>R PROBLEM<br />
Congenital<br />
Hemophilia A/B<br />
Von-Willebrand factor<br />
Christmas tree factor def<br />
Acquired<br />
DIC<br />
Warfarin<br />
Vit K deficiency<br />
Liver dz, renal dz<br />
<strong>APPROACH</strong> <strong>TO</strong> THE PURPURIC RASH<br />
MUST consider non-accidental trauma<br />
Other causes of sepsis actually more common than meningococcus for the sick purpuric rash<br />
The well looking person/child with a petechial rash? Is it meningococcemia????<br />
Many infections can cause petechiae or ecchymosis in absence of platelet or<br />
coagulation disorder<br />
Capillary damage from the infection<br />
Rubeola, mono, ricketsia, streptococcal, RMSF, endocarditis can all present<br />
Keep in mind the above ddx: vascular integrity problem, thrombocytopenia, coagulation factor<br />
problem<br />
Approach<br />
Toxic appearing: monitored bed, iv access, draw labs, fluid bolus, draw cultures, start antibiotics,<br />
resuscitate as needed<br />
History and Physical: drugs, infectious symptoms, bleeding history, easy bleeding or brusing,<br />
lumps or bumps, weight loss or systemic symptoms, full review of symptoms<br />
Order: CBC, diff, platelet count, retic count, PTT, INR, bleeding time<br />
Thrombocytopenia<br />
Prolonged INR/PTT: sepsis and DIC<br />
Normal INR/PTT: ITP, TTP, HUS, bone marrow suppression, bone marrow infiltration, platelet<br />
sequestration<br />
Platetlets normal, INR/PTT prolonged<br />
Hemophilia<br />
Liver dz<br />
Warfarin<br />
Platelets normal, INR/PTT normal, Bleeding Time prolonged<br />
Von-Willebrand disease<br />
Aspirin or other platelet inhibitors<br />
Platelets normal, INR/PTT normal, Bleeding Time normal<br />
Vasculitis: HSP, serum sickness, cryoglobuinemia, IVDA, kawasaki’s<br />
Trauma<br />
Infections
Drugs<br />
Connective tissue disease<br />
MALIGNANCY AND DERMA<strong>TO</strong>LOGY<br />
ACANTHOSIS NIGRANS<br />
Most do NOT have tumors but some do<br />
Malignant acanthosis nigrans: = associated with cancer (skin lesion itself is NOT cancer)<br />
Hyperpigmented verrucous velvet - like hyperplasia and hypertrophy of the skin with<br />
accentuated skin markings: body folds, especially axillae, antecubital fossae, neck and groins<br />
MC is adenocarcinoma of the stomach<br />
Others: breast, ovary, pancreas, colon, uterus<br />
Tumor produces insulin-like growth factor which stimulates the skin<br />
DERM<strong>TO</strong>MYOSITIS<br />
Some will have underlying malignancy<br />
Breast, ovary, GI, uterus<br />
ERYTHEMA MULTIFORME<br />
Associated with leukemia<br />
Also Hodkin’s<br />
ERYTHRODERMA<br />
Almost pathognomonic of Hodgkin’s lymphoma<br />
Also occurs with lymphocytic leukemia<br />
ACQUI<strong>RED</strong> ICHTHYOSIS<br />
Generalized dryness of skin, scalin, superficial cracking, or hyperkeratosis of soles and palms<br />
Hodgkin’s is MCC<br />
Other cancers also<br />
PRURITIS<br />
Hodgkin’s lympoma, leukemia, adenoCa, Sqcell Ca, carcinoid, multiple myeloma<br />
Hodgkin’s may have severe itching and burning sensations<br />
Standard treatments ineffective<br />
PURPURA<br />
MC manifestation of acute granulocytic and monocytic leukemia<br />
Also myeloma, lymphoma, polycthemia vera<br />
Thrombocytopenia secondary to BM suppression is the mechanism<br />
Non-thrombocytopenic forms do occur<br />
URTICARIA<br />
Hodgkins<br />
Leukemia<br />
Internal carcinomas
NARCOTIC ADDICTION<br />
Skin needle tracks: indurated linear hyperpigmented streaks<br />
Skin popping: subcutaneous injections result in round or oval hyperpigmented atrophic<br />
depressed scars 1-3 cm in diameter<br />
Skin abscesses<br />
Hypertrophic keloid scars<br />
Increased pigmentation at site of tourniquet use