ESOPHAGEAL OBSTRUCTION - rEMERGs
ESOPHAGEAL OBSTRUCTION - rEMERGs
ESOPHAGEAL OBSTRUCTION - rEMERGs
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
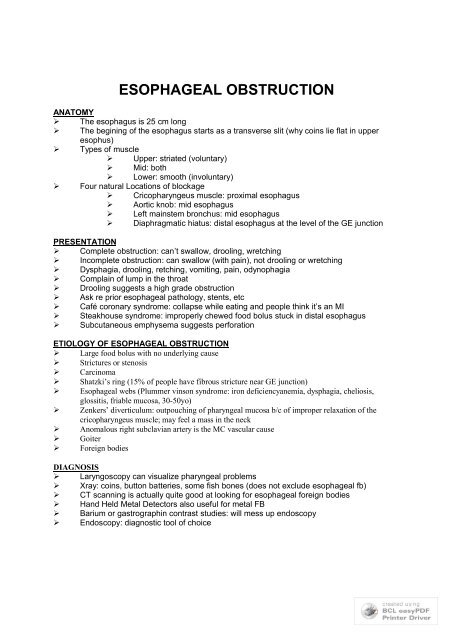
<strong>ESOPHAGEAL</strong> <strong>OBSTRUCTION</strong><br />
ANATOMY<br />
‣ The esophagus is 25 cm long<br />
‣ The begining of the esophagus starts as a transverse slit (why coins lie flat in upper<br />
esophus)<br />
‣ Types of muscle<br />
‣ Upper: striated (voluntary)<br />
‣ Mid: both<br />
‣ Lower: smooth (involuntary)<br />
‣ Four natural Locations of blockage<br />
‣ Cricopharyngeus muscle: proximal esophagus<br />
‣ Aortic knob: mid esophagus<br />
‣ Left mainstem bronchus: mid esophagus<br />
‣ Diaphragmatic hiatus: distal esophagus at the level of the GE junction<br />
PRESENTATION<br />
‣ Complete obstruction: can’t swallow, drooling, wretching<br />
‣ Incomplete obstruction: can swallow (with pain), not drooling or wretching<br />
‣ Dysphagia, drooling, retching, vomiting, pain, odynophagia<br />
‣ Complain of lump in the throat<br />
‣ Drooling suggests a high grade obstruction<br />
‣ Ask re prior esophageal pathology, stents, etc<br />
‣ Café coronary syndrome: collapse while eating and people think it’s an MI<br />
‣ Steakhouse syndrome: improperly chewed food bolus stuck in distal esophagus<br />
‣ Subcutaneous emphysema suggests perforation<br />
ETIOLOGY OF <strong>ESOPHAGEAL</strong> <strong>OBSTRUCTION</strong><br />
‣ Large food bolus with no underlying cause<br />
‣ Strictures or stenosis<br />
‣ Carcinoma<br />
‣ Shatzki’s ring (15% of people have fibrous stricture near GE junction)<br />
‣ Esophageal webs (Plummer vinson syndrome: iron deficiencyanemia, dysphagia, cheliosis,<br />
glossitis, friable mucosa, 30-50yo)<br />
‣ Zenkers’ diverticulum: outpouching of pharyngeal mucosa b/c of improper relaxation of the<br />
cricopharyngeus muscle; may feel a mass in the neck<br />
‣ Anomalous right subclavian artery is the MC vascular cause<br />
‣ Goiter<br />
‣ Foreign bodies<br />
DIAGNOSIS<br />
‣ Laryngoscopy can visualize pharyngeal problems<br />
‣ Xray: coins, button batteries, some fish bones (does not exclude esophageal fb)<br />
‣ CT scanning is actually quite good at looking for esophageal foreign bodies<br />
‣ Hand Held Metal Detectors also useful for metal FB<br />
‣ Barium or gastrographin contrast studies: will mess up endoscopy<br />
‣ Endoscopy: diagnostic tool of choice
‣<br />
Complications<br />
‣ Perforation 2%<br />
‣ Airway obstruction<br />
‣ Mediastinitis<br />
‣ Fistulas<br />
‣ Extraluminal migration<br />
‣ Esophageal strictures<br />
MANAGEMENT<br />
‣ Food Bolus<br />
‣ Never use papain: increased perforation rate<br />
‣ Glucagon 1.0 mg iv (decreases LES tone, may cause vomiting); only useful for<br />
lower esophageal impaction (no smooth muscle in upper esophagus);<br />
contraindicated in sharp FB, upper esophageal FB, insulinoma,<br />
pheochromocytoma, Zolinger-Ellison syndrome<br />
‣ COKE for gas forming properties: works 60% of the time (Tartaric acid + sodium<br />
bicarb has also been used - produces carbon dioxide)<br />
‣ Expectant managment: observe for 24 hours and then endoscopy prn; should not<br />
leave > 24hrs<br />
‣ Endoscopic removal<br />
Emergent for airway obstruction<br />
Urgent for failure of above, > 24 hours<br />
Indicated for suspected strictures, carcinoma, webs, rings, etc<br />
Emergent Endoscopy<br />
‣ Airway obstruction<br />
‣ Can’t handle secretions<br />
‣ Must come out regardless of location b/c of risk of erosion<br />
‣ Only one you could potentially watch is right at the GE junction<br />
‣ Concerns of both foreign body and caustic ingestions<br />
‣ Contains metal salt and a variety of caustic alkaline substances: sodium and<br />
potassium hydroxide<br />
‣ Majority pass uneventfully in stool and most within 4 - 7 days<br />
‣ Rare fatal complications: esophageal - aorta fistula<br />
‣ Airway assessment is key initial management<br />
‣ Radiographic localization via chest or abdominal Xrays<br />
‣ Airway or lower respiratory tract location are usually symptomatic and require<br />
bronchoscopy<br />
‣ Intact batteries past esophagus: d/c home and watch stool, return if problems<br />
‣ Children < 6yo + battery > 15mm: unlikely to pass pyloris thus must re- evaluate<br />
in 48hrs with repeat Xrays to visualize: endoscopic removal if not past pyloris<br />
‣ Esophageal location requires endoscopic removal<br />
‣ Other foreign bodies<br />
‣ Watch if at lower esophagus<br />
‣ Endoscopy if at upper esophagus<br />
‣ ED removal with sedation and foley catheter has been described for upper<br />
esophageal foreign bodies<br />
‣ Emergent endoscopy: AWO, can’t handle secretions<br />
‣ Urgent endosocpy: upper esophagus, button batteries, > 24hr duration, sharp<br />
objects
<strong>ESOPHAGEAL</strong> PERFORATION<br />
INTRODUCTION<br />
‣ Most rapidly fatal perforation of GIT; was uniformly fatal<br />
‣ Mortality now 30% depending on MOI, Pmhx, esoph pathology<br />
PATHOPHYSIOLOGY<br />
‣ NO serosal covering of the esophagous :. direct access to mediastinum<br />
‣ Upper esophageal perforation drains into the retropharyngeal space b/c of fascial planes<br />
that extend from the base of the skull to the bifurcation of the trachea<br />
‣ Thin mediastinal pleura rarely prevents drainage into pleural cavity<br />
‣ Massive chemical and bacterial mediastinitis<br />
‣ Sepsis, volume loss, obstructive shock, resp failure, death<br />
‣ Inherent wkness of left posterior esoph leads to it being the MC emesis induced rupture<br />
site<br />
‣ Esophageal pathology can alter sites<br />
‣ Rupture secondary to FB occurs at three areas of narrowing ....<br />
‣ Cricopharyngeal muscle near the esoph intoitus<br />
‣ Espophageal crossing of the left mainstem bronchus and aortic arch<br />
‣ GE junction<br />
ETIOLOGY<br />
‣ Iatrogenic (MC)<br />
‣ Endoscopy: MCC, 0.5% of endoscopy, rigid > flexible, inc w/ corrosives<br />
‣ NG/OG tubes: MCC in ED, perforates pyriform sinus<br />
‣ Foreign Bodies<br />
‣ Lacerations, pressure necrosis<br />
‣ Usu in cervical esoph unless tumor/stricture in lower esoph<br />
‣ Kids < 4yo: cricopharyngeal narrowing is MC location<br />
‣ Caustic Burns<br />
‣ Alkali: liquefaction necrosis, more commonly causes perf than acids<br />
‣ Acids: coagulation necrosis, less perforation<br />
‣ Must have endoscopy<br />
‣ Penetrating Trauma<br />
‣ 5 - 30% of all esoph perfs<br />
‣ Penetrations of neck, chest, or abd<br />
‣ Blunt Trauma<br />
‣ Rarely isolated injury; tracheal injury is MC associated injury<br />
‣ Cervical esoph is MC location<br />
‣ Commonly overlooked b/c of dramatic tracheal injury<br />
‣ Xrays: blood/air in retropharyngeal space on lateral C-spine<br />
‣ Has been assoc w/ C-spine #<br />
‣ Spontaneous Rupture<br />
‣ Bourhaave’s syndrome, Postemetic perforation<br />
‣ worst prognosis b/c massive seeding of mediastinum<br />
‣ Longitudinal left posterolateral tear MC b/c of inherent wkness<br />
‣ 80% male, middle aged a/f +++ food and EtoH<br />
‣ Neonatal has occurred<br />
‣ May occur in normal or pathological esoph
‣<br />
Rare: blunt abdominal trauma, laughing, straining, lifiting<br />
CLINICAL FEATURES<br />
‣ 2/3 with suggestive presentation: emesis then severe CP, subQ air, collapse or a/f<br />
endoscopy<br />
‣ 1/3 with less suggestive presentation<br />
‣ History<br />
‣ Substernal, epigastric, back pain<br />
‣ Usually pleuritic<br />
‣ Dyspnea with mediastinitis<br />
‣ Physical<br />
‣ Hamman’s crunch w/ air in mediastinum<br />
‣ Hydropneumothorax or empyema<br />
‣ SubQ air dissecting into neck classical but only in 50%<br />
‣ Late: fever, sepsis, resp failure, death<br />
‣ CXR<br />
‣ Mediastinal air +/- subQ air<br />
‣ Left pleural effusion<br />
‣ Pneumothorax<br />
‣ Wide mediastinum<br />
‣ May be normal<br />
‣ Lateral C spine<br />
‣ Air/fluid in retropharyngeal space<br />
‣ Perf esoph vs spontaneous pneumomediastinum<br />
‣ Spont pneumomed may occur from valsalva, very painful, 10 - 40 yo<br />
‣ NO pulmn infiltrate, NO pleural effusion, NO mediastinal AF level, with<br />
mediastinal air<br />
‣ Esophogram if in doubt<br />
‣ Ba swallow vs Gastrograffin<br />
‣ Start w/ gastrograffin water - soluble contrast which will produce less<br />
mediastinal soiling and won’t obscure endoscopy<br />
‣ Then do Barium if intact<br />
‣ Endoscopy<br />
ED MANAGEMENT<br />
‣ Early dx most imp<br />
‣ NPO, Abx, volume<br />
‣ NG tube<br />
‣ Early surgical consult
DYSPHAGIA<br />
DEFINITIONS<br />
‣ Dysphagia = difficulty swallowing<br />
‣ Odynophagia = pain on swallowing<br />
‣ Globus (Hystericus) = the sensation of a lump in the throat but is not related to the act of<br />
swallowing and thus does not constitute dysphagia<br />
ETIOLOGY<br />
‣ Box 115 - 2<br />
PATHOPHYSIOLOGY<br />
‣ Swallowing: oral, pharyngeal, and esophageal phases<br />
‣ Oral phase: absence of lubrication (Sjogren’s), weakness of tongue by CN XII lesion,<br />
thick tongue from amyloidosis, weak buccal muscles from CN VII lesion, decreased<br />
mouth opening (scleroderma) can all lead to dysphagia<br />
‣ Pharyngeal phase: weakness, incoordination<br />
‣ Esophageal phase: obstruction, weakness, incoordination<br />
PRESENTATION<br />
‣ History: ask duration, location, solids vs liquids, intermittent vs constant vs progressive,<br />
associated symptoms (pain, heartburn, systemic), previous esophageal disease,<br />
ingestants (caustics), fhx of neurological disease<br />
‣ Physical: thorough head, neck, and neurological examination, observe swallowing<br />
OROPHARYNGEAL DYSPHAGIA<br />
‣ Symptoms manifest within 1 - 2 seconds of swallowing<br />
‣ Include: lubrication problems, mastication, transfer from mouth to pharynx, passage<br />
through cricopharyngeus,<br />
‣ Also called transfer dysphagia<br />
‣ Etiology: 80% are neuromuscular, 20% structural<br />
‣ Painful lesions: pharyngitis, diptheria, mumps, apthous uslcers, herpes, candida,<br />
oropharyngeal abcesses; should be seen on physical<br />
‣ Carcinoma: functional obstruction to tongue, palate, fixation of larynx; look on physical<br />
and with laryngoscopy<br />
‣ Scleroderma: dry mouth, decreased mouth opening, neuromuscular damage to<br />
esophagus<br />
‣ CVA: most common cause for neuromuscular dysphagia, especially those involving the<br />
posterior circulation<br />
‣ Neuromuscular: poly or dermatomyositis and myasenia gravis are two other common<br />
causes
UPPER <strong>ESOPHAGEAL</strong> DYSPHAGIA<br />
‣ Symptoms manifest within 2 - 4 seconds after swallowing initiated<br />
‣ Dysphagia localized to substernal or retrosternal may be anatomically accurate but<br />
dysphagia localized to neck may be referred from anywhere in the esophagus<br />
‣ Mechanical/obstructive: usually constant and progressive<br />
‣ Motility: usually intermittent and variable<br />
‣ Inflammatory lesions: candida, thyroiditis, aphthous ulcers, epidermolysis bullosa and<br />
pemphigoid (epithelial alterations), cervical spondylitis (osteophytes impinge on<br />
esophagus), foreign bd<br />
‣ Obstructive: intrinsic<br />
‣ Carcinoma<br />
‣ Webs: Plummer - Vinson syndrome (anterior webs, dysphagia, iron<br />
deficiency anemia, cheilosis, spooning of nails, glossitis, thin<br />
oropharyngeal mucosa; usu 30 - 50 and female<br />
‣ Obstructive: extrinsic<br />
‣ Carcinoma<br />
‣ Thyromegaly<br />
‣ Vascular anomaly (anomalous right subclavian artery in adults)<br />
‣ Aneurysms<br />
‣ Zenker’s diverticulum<br />
‣ Bronchogenic carcinoma<br />
LOWER <strong>ESOPHAGEAL</strong> DYSPHAGIA<br />
‣ Symptoms manifest 4 - 10 seconds after initiation<br />
‣ Commonly described as “sticking sensation”<br />
‣ Symptoms usually perceived at the appropriate location (substernal)<br />
‣ Usually caused by luminal narrowing: constant (carcinoma) or intermittent (spasm)<br />
‣ Dysphagia in > 40 yo should be assumed to be carcinoma until proven otherwise<br />
‣ Achalasia<br />
‣ Marked increased resting pressure of LES and absence of peristalsis in<br />
body<br />
‣ Most b/w 20 - 40<br />
‣ Dysphagia most common presentation: insidious onset, solids and liquids<br />
‣ May report using maneuvers to help pass food (raising arms above head,<br />
standing erect with back straight ----> increases esophageal pressure)<br />
‣ Odynophagia, regurgitation, aspiration can all be features<br />
‣ Strictures<br />
‣ Long history of heartburn with slow onset of progressive dysphagia<br />
‣ May be sequelae of scleroderma, caustic ingestants<br />
‣<br />
Steakhouse syndrome<br />
‣<br />
‣<br />
‣<br />
‣<br />
Large piece of improperly chewed food swallowed causing esophageal<br />
obstruction in the distal esophagus, may spontaneously pass, intense<br />
discomfort<br />
Alcohol ingestion and absence of teeth are predisposing factors<br />
May occur in a normal esophagus but tends to occur in esophagus with<br />
carcinoma, stricuture, or Schatzki’s ring (fibrous stricture near the GE<br />
junction in up to 15% of normal population)<br />
Complete obstruction: can’t swallow anything else, drooling, wretching
INVESTIGATIONS<br />
‣ Neck Xrays: look for retropharyngeal abscesses, masses, foreign bodies, epiglottitis,<br />
osteophytes of cervical spine, air in Zenker’s diverticulum, trapped air around obstructing<br />
food bolus<br />
‣ CXR should be obtained in abscence of obvious oropharyngeal cause: look for<br />
mediastinal masses, aneurysms, tumors, thyroid, dilated esophagus wit air - fluid level in<br />
achalasia, air in esophagus on both views suggests scleroderma, lung infiltrates with<br />
aspiration<br />
‣ Tensilon Test: 10 mg of edrophonium for suspected myasthenia gravis<br />
‣ Foreign bodies<br />
‣ Coins most common in peds<br />
‣ Meat and bones most common in adults<br />
‣ Tend to lodge at narrowings: cricopharyngeus, aortic arch, left mainstem<br />
bronchus, and diaphragmatic hiatus<br />
‣ Endoscopy is preferred investigation<br />
‣ Contrast studies are an option but may obscure the endoscopic view: if<br />
perforation suspected use Gastrogaffin, if aspiration a possibility use<br />
Barium, if both a concern then use nonionic contrast agents (note barium<br />
obscures endoscopic view)<br />
MANAGEMENT<br />
‣ Depends on cause<br />
‣ Consider ability to orally hydrate<br />
‣ Consider risk of airway obstruction and aspiration<br />
‣ Foreign bodies<br />
‣ Oropharyngeal foreign bodies can be removed under direct visualization<br />
‣ Upper esophageal foreign bodies can be removed with a foley catheter<br />
under fluroscopic guidance<br />
‣ Lower esophageal foreign bodies (usually food)<br />
glucagon 0.5mg - 2.0 mg: causes esophageal smooth<br />
muscle relaxation for spontaneous passage, works in 50%;<br />
s/e include nasuea, vomiting, dizziness, flushing; should<br />
not be used with sharp objects, or patients with insulinoma,<br />
pheochromocytoma, and Zollinger - Ellison syndrome<br />
effervescent agents: carbonated beverages to produce<br />
C02 which helps pass the bolus; reported to work in 60%<br />
alone and in 75% in combination with glucagon<br />
endoscopy: sharp - edges, distal, contraindications to<br />
above, failure of treatment; immediate for significant<br />
distress and caustics; unclear if emergent endoscopy<br />
necessary for mild to moderate symptoms<br />
consider elective endoscopy to look for pathology even if<br />
foreign body spontaneously passes
CHEST PAIN OF <strong>ESOPHAGEAL</strong> ORIGIN<br />
INTRODUCTION<br />
‣ Etiology: GERD, Esophagitis, Perforation (traumatic, spontaneous, iatrogenic), Motility<br />
disorder: achalasia, diffuse esophageal spasm, hypertensive LES, nutcracker esoph<br />
‣ Esophageal pain can be stimulated by distension, spasm, chemical irritation, temperature<br />
‣ Note similar segmental innervation of heart and esophagus and the convergence of<br />
sympathetic afferents onto projection neurons receiving both somatic and visceral input --<br />
---------> thus chest pain rising from the esophagus may be indistinguishable from<br />
myocardial ischemia<br />
‣ Investigations: ECG mandatory, CXR often helpful, remainder depend on suspected<br />
diagnosis and condition of patient<br />
GASTRO<strong>ESOPHAGEAL</strong> REFLUX DISEASE (GERD)<br />
‣ Pathophysiology<br />
‣ Due to “Acid in the wrong place, NOT over acid production”<br />
‣ Majority of reflux episodes due to transient LES relaxation<br />
‣ GERD can occur w/o hiatus hernia and vica versa<br />
‣ Aggravating factors<br />
‣ Fat, caffeine, chocolate, salivation disorders, juices, pepermint, delayed<br />
gastric emptying, posture, obesity, hiatus hernia, inc abd pressure<br />
(pregnancy), drugs (CCBs, NTG, BB), alcohol/cigarrettes (inc acid<br />
production)<br />
‣ Typical presentation<br />
‣ Onset usu following meals or postural maneuvers (lie flat, bending)<br />
‣ Symptoms: HB, regurg, waterbrash, CP, dysphagia due to stricture or<br />
motility, resp s/s; odynophagia is rare and suggests infection<br />
‣ Atypical presentations<br />
‣ Non-cardiac CP, respiratory s/s (laryngitis, pharyngitis, asthma, chronic<br />
cough, recurrent pneumonias), globus hystericus: lump in throat<br />
(hypertonic LES in response to GER)<br />
‣ Diagnosis<br />
‣ pH reflux study (Gold standard for proving presence of GER)<br />
‣ Bernstein (GS in proving s/s due to GER)<br />
‣ Endoscopy (best to show mucosal damage and look for barrett’s<br />
‣ Barium meal<br />
‣ Radionuclide scintigraphy<br />
‣ Red Flags require endoscopy<br />
‣ Dysphagia, new onset in elderly, anemia, hemetamesis, s/s refractory to<br />
tx, atypical CP, odynophagia, pharyngitis, laryngitis, to R/O barret’s<br />
‣ Complications<br />
‣ Ulcer (5%)<br />
‣ Hemmorrhage (
‣<br />
Resp Complications: recurrent chest infections, chronic cough, laryngitis<br />
‣<br />
Management<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
Does NOT target H. pylori (not related to GERD)<br />
Phase I: dietary, elevate bed, avoid factors which dec LES tone, wt loss,<br />
stop smoking, review drugs, avoid night time eating, dietary review,<br />
frequent small meals, symptomatic antacids<br />
Phase II: H2 antagonists (ranitidine)<br />
Phase III: PPIs (omeprazole)<br />
Phase IV: surgery (fundoplication)<br />
NONREFLUX-INDUCED ESOPHAGITIS<br />
‣ Candidal Esophagitis<br />
‣ MOST COMMON infectious esophagitis<br />
‣ Predispositions: DM, antibiotics, immunocompromised<br />
‣ May be asymptomatic, may or may not have thrush as well<br />
‣ Symptoms: odynophagia, retrosternal CP, and/or dysphagia<br />
‣ Complications: bleeding, stricture, sinus tracts w/ lung abcesses<br />
‣ Endoscopy and Bx are required for Dx (barium not good enough)<br />
‣ Treatment: nystatin po ketoconazole/fluconazole iv if immunocompromi<br />
‣ Ampho B required if there is evidence of systemic spread<br />
‣ Herpes Simplex Esophagitis<br />
‣ SECOND most common cause of infection esophagitis<br />
‣ Presentation similar +/- URTI or herpetic mouth or skin lesions<br />
‣ Usually immunocompromised but not always<br />
‣ Dx: endoscopy + bx<br />
‣ Tx: NOT required in immunocompetent<br />
‣ Acyclovir IV for immunocomprmsd<br />
‣ Odynophagia relieved by antacids + viscous Xylocaine<br />
‣ Other Infectious Esophagitis<br />
‣ Bacteria rare but can be involved secondarily from the lung<br />
‣ CMV, HIV, and fungi are uncommon and usu assoc. w/<br />
immunocompromised<br />
‣ Immune - Mediated Esophagitis<br />
‣ Crohn’s disease<br />
‣ Epidermolysis bullosa and pemphigoid<br />
‣ Graft vs Host disease<br />
‣ Sarcoidosis and esosinophillic gastroenteritis<br />
‣ Chemical - Induced Esophagitis<br />
‣ Caustics: acid and alkali (worse), requires endoscopy<br />
‣ Pill - induced: NSAIDS, Kcl, anticholinergics common; take med w/o<br />
enough water and wake up with severe chest pain and odynophagia;<br />
especially common in motility disorders<br />
‣ Radiation Esophagitis
MOTILITY DISORDERS<br />
‣ Nutcracker Esophagus<br />
‣ Normal propagation but high amplitude waves in distal esophagus and<br />
prolonged contraction, LES normal (pressure may be elevated)<br />
‣ C/O angina-like CP not usu dysphagia<br />
‣ Most common abnormal manometric finding in pts reffered for non-cardiac<br />
CP<br />
‣ Tx: nitrates, CCBS, antireflux treatment<br />
‣ Diffuse Esophageal Spasm<br />
‣ Normal peristalsis w/ frequent high pressure nonpropagated or tertiary<br />
waves and multipeaked waves<br />
‣ C/O CP + dysphagia<br />
‣ Tx: nitrates, CCBs, esophageal myotomy<br />
‣ Achalasia<br />
‣ Aperistalsis in esphageal bd, elevated LES pressure, and inadequeate<br />
LES relaxation leading to prominent dilation of proximal esoph on XR;<br />
distal end narrows to a “beak”<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
Vigorous achalasia: associated vigorous contractions in esph body<br />
Pathology: degeneration of inhibitory neurons w/i the esoph and LES<br />
myenteric plexus; nerve damage also occurs in vagal nerve trunks and<br />
the dorsal motor nuclei<br />
Trypanosoma cruzi (Chaga’s dz) can distroy myenteric neurons (BRAZIL)<br />
Neoplasm can also cause secondary achalasia<br />
Symptoms: dysphagia +/- CP and HB (due to degeneration of stagnant<br />
contents, not GER)<br />
Treatment: CCBs and nitrates, pneumatic balloon dilation of LES is usu<br />
required, Heller myotomy via laproscope if above fails, botulinum toxin<br />
injection effective but only lasts for 1yr
GASTRO<strong>ESOPHAGEAL</strong> REFLUX DISEASE<br />
Introduction<br />
‣ MOST COMMON condition of the esoph: daily 7%, weekly 14%, monthly in 40%<br />
‣ Spectrum from normal to severe symptoms, barret’s esoph, adenoCa<br />
Normal Barriers to GER<br />
‣ Lower esophageal sphincter: most important barrier, near normal in pts w/ GERD<br />
‣ Esophageal clearance: primary and secondary peristalsis, neutralization by saliva<br />
‣ Mucosal resistance<br />
Pathophysiology<br />
‣ Due to “Acid in the wrong place, NOT over acid production”<br />
‣ Majority of reflux episodes due to transient LES relaxation<br />
‣ GERD can occur w/o hiatus hernia and hiatus hernia can occur w/o GERD<br />
‣ Aggravating factors<br />
- fat, caffeine, chocolate - salivation disorders<br />
- juices, pepermint - delayed gastric emptying<br />
- posture - obesity<br />
- hiatus hernia - inc abd pressure (pregnancy)<br />
- drugs (CCBs, NTG, - alcohol/cigarrettes<br />
‣ Drugs that worsen GERD: CCB, NTG, BB, anticholinergics, etc)<br />
Clinical Features<br />
‣ Onset usu following meals or postural maneuvers (lie flat, bending)<br />
‣ Symptoms: HB, regurg, waterbrash, CP, dysphagia due to stricture or motility, resp s/s;<br />
odynophagia is rare and suggests infection<br />
‣ Pregnancy: increased abd P and relaxed LES due to progesterone<br />
‣ Atypical presentations<br />
‣ non-cardiac CP<br />
‣ respiratory s/s: laryngitis, pharyngitis, asthma, chronic cough, pneumonias<br />
‣ globus hystericus: lump in throat (hypertonic LES in response to GER)<br />
Diagnosis<br />
‣ pH reflux study (Gold standard for proving presence of GER)<br />
‣ 24hr pH recording determines if symptoms are due to reflux<br />
‣ Red Flags require endoscopy<br />
- dysphagia, new onset in elderly, anemia, hemetamesis, s/s refractory to tx,<br />
atypical CP, odynophagia, pharyngitis, laryngitis<br />
- once in a lifetime endoscopy to R/O barret’s<br />
- young, mild s/s ------- empiric tx w/o endoscopy<br />
Complications of GERD<br />
‣ Ulcer (5%)<br />
‣ Esophagitis<br />
‣ Hemmorrhage (
- occurs in 10% of pts w/ GERD<br />
- 10% of pts w/ barrett’s esoph have coexistent adenoCa at time of dx<br />
- 40Xs risk of Ca than general population<br />
- should be followed w/ endoscopy and bx<br />
Differential dx<br />
‣ Cardiac ischemia is the main ddx<br />
‣ Note that GERD pain can radiate similar to ischemia<br />
‣ Radiation to abdomen is 3Xs more commonn in GERD than ischemia<br />
‣ Exacerbation of symptoms after meals (fullness sensation) is more suggestive of GERD<br />
‣ Worse with swallowing suggests GERD<br />
‣ Relief by antacids does NOT r/o cardiac<br />
Treatment<br />
‣ Does NOT target H. pylori (not related to GERD)<br />
‣ PHASE I<br />
- lifestyle, dietary, elevate bed, avoid factors which dec LES tone, wt lo<br />
loss, stop smoking, review drugs, avoid night time eating, dietary review,<br />
frequent small meals, symptomatic antacids<br />
‣<br />
‣<br />
‣<br />
PHASE II<br />
- H2 antagonist<br />
‣ cimetidine (tagamet) 300mg bid<br />
‣ ranitidine (zantac) 150mg bid<br />
‣ famotidine (pepcid)40mg od<br />
‣ nizantidine (axid) 150mg bid<br />
- prokinetics<br />
‣<br />
PHASE III<br />
- PPIs<br />
‣<br />
‣<br />
‣<br />
PHASE IV<br />
- sugery (fundal plication)<br />
cisapride (prepulsid) 20mg bid - qid (inc LES tone, and inc<br />
gastric emptying)<br />
omeprazole (losec) 20mg od<br />
lanoprazole (prevasid) 30mg od<br />
pantoprazole (pantoloc) 40mg od
ABDO PAIN: GASTRIC OR DUODENAL ORIGIN<br />
CLINICAL HIGHLIGHTS<br />
ETIOLOGY<br />
‣ Peptic Ulcer Disease<br />
‣ Non - ulcer Dyspepsia<br />
‣ Gastritis<br />
‣ Superior Mesenteric Artery (SMA) syndrome<br />
‣ Gastric Volvulus<br />
HISTORY<br />
‣ Location<br />
‣<br />
‣<br />
‣ Radiation<br />
‣<br />
‣<br />
‣ Character<br />
‣<br />
‣<br />
‣<br />
‣ Timing<br />
‣<br />
‣<br />
‣<br />
Other<br />
‣<br />
‣<br />
‣<br />
‣<br />
Gastric tends to be epigastrium and slightly left<br />
Duodenal tends to be epigastrium and slightly right<br />
Back: think perforated duodenal ulcer<br />
Shoulder: think perforation of ulcer with subdiaphragmatic air<br />
Constant, gnawing: think GU, DU (rarely a colicky pain)<br />
Hot, burning, bloating: think gastritis<br />
Cramping: think SMA syndrome<br />
Gastritis: onset of pain w/i 1hr of eating, food increases pain<br />
GU/DU: food relieves pain most commonly (more reliable with DU than<br />
GU)<br />
DU may waken patient at 0200: think DU b/c gastric secretion increases<br />
then (ulcer pain is rarely present on wakening)<br />
SMA: precipitated by food<br />
Alleviators: antacids decrease 90% of PUD pain and 75% of gastritis pain<br />
Onset: very sudden onset think gastric volvulus or perforation<br />
PHYSICAL<br />
‣ Peritonitis: perforation or late volvulus with strangulation<br />
‣ Decreased bowel sounds: same<br />
‣ OB+ve stool: bleeding PUD<br />
‣ Virchow’s node: think Ca<br />
INVESTIGATIONS<br />
‣ Blood work depends on presentation<br />
‣ AXR: look for free air with perforation or large, distended stomach with volvulus<br />
‣ ECG mandatory in adults<br />
MANAGEMENT<br />
‣ NG tube for perforation or suspected volvulus (can’t pass tube)<br />
‣ Emergent OR for perforation or volvulus<br />
‣ Further management depends on working dx
DUODENAL ULCERS<br />
EPIDEMIOLOGY<br />
‣ 5-15% of western population (incidence decreasing) during life<br />
‣ Duodenal Ulcer (DU) 4Xs more common than Gastric Ulcer (GU)<br />
‣ 3 male:1 female<br />
‣ No increase risk of Ca<br />
‣ Hereditary factors<br />
ETIOLOGY<br />
‣ 90% related to H.pylori<br />
‣ 7% related to NSAIDS<br />
‣ 3% other: ZES, stress, ischemia, viral<br />
PATHOGENESIS<br />
‣ Imbalance b/w damaging factors (acid/pepsin) and protective factors (mucus, HCO3,<br />
Pgs)<br />
‣ Strong evidence for HP as etiologic factor<br />
‣ May produce toxins which cause gastric mucosal damage<br />
‣ May prevent antral G cells from sensing lumenal acid thus increasing<br />
serum gastrin and ultimately increasing acid secretion<br />
‣ Other associated pathogenic factors<br />
‣ Drugs: NSAIDS<br />
‣ Smoking: 2Xs rate, 2Xs recurrence, 2Xs as long to heal, higher death<br />
rate, higher complication rate (best thing you can do is get pt to stop<br />
smoking)<br />
‣ Alcohol: damages mucosa but not assoc w/ulcers<br />
‣ Caffeine: increase acid secretion<br />
‣ Diet: causes dyspepsia but little documented role in ulcers<br />
‣ Stress: more perforation, more s/s<br />
‣ Associations w/ cirrhosis, COPD, renal failure (uremia)<br />
‣ Location<br />
‣ 90% in 1 st part of duodenum (90% of these w/i 3cm of pyloric-duo jnt)<br />
‣ Anterior > posterior<br />
CLINICAL FEATURES<br />
‣ Pain<br />
‣ Many patients w/ active DU have no ulcer symptoms<br />
‣ Epigastric pain, ill defined border, +/- back radiation, may be RUQ<br />
‣ Sharp, burning, gnawing, boring<br />
‣ Typically occurs before or 90min - 3hrs a/f eating (frequently wakes<br />
patient up at 0200 b/c of high gastric output)<br />
‣ Increase w/ fasting<br />
‣ Relieved by food and antacids (neutralize acid)<br />
‣ Episodes may persist for days to weeks and tend to be recurrent &<br />
episodic<br />
‣ Remissions last from weeks to years<br />
‣ Pain increase w/ food + vomiting suggests gastric outlet obstruction
‣<br />
‣<br />
May present w/ Complications<br />
‣ GI hemmorrhage: acute or chronic, minor —> massive (erosion of<br />
gastroduodenal artery can produce massive bleeding)<br />
‣ Perforation of duodenal bulb: sudden onset of severe, generalized<br />
abdominal pain radiating to back/shoulder with peritoneal findings of an<br />
acute abdomen +/- free air on AXR; may be more subtle with more<br />
constant pain, failure of treatment<br />
‣ Gastric outlet obstruction: due to edema, spasm, fibrosis; presents with<br />
N+V, crampy abdo pain, dilated stomach, succusion splash<br />
‣ Posterior penetration into pancreas :. pancreatitis<br />
Physical Examination<br />
‣ Epigastric tenderness<br />
‣ Weight loss unusual in DU in absence of gastric outlet obstruction<br />
‣ Peritonitis if perforated<br />
‣ Succussion splash w/ gastric outlet obstruction due to air/fluid retension in<br />
stomach (unreliable)<br />
DIAGNOSIS<br />
‣ UGI series: 90% sensitive w/ double contrast<br />
‣ Endoscopy: most accurate method of dx<br />
‣ HP testing: may be unnecessary b/c the organism is presumed to be there<br />
‣ Measure serum gastrin in gastrinoma suspected: Fhx, diarrhea, multiple ulcers, poor<br />
response to Rx, unusual location<br />
TREATMENT<br />
‣ Lifestyle modification<br />
‣ Reduce acid<br />
‣ Antacids: Malox, Mylanta (s/e: constipation or diarrhea)<br />
‣ Anticholinergics: pirenzipine (high s/e, contraind in glaucoma, not used)<br />
‣ Antigastin: proglumide<br />
‣ Mucosal protectants<br />
‣ Sucralfate: not absorbed :. safe in pregnancy<br />
‣ Prostaglandins: misoprostol used for prevention of NSAID induced ulcers<br />
‣ PGE2 may b/cm treatment of choice<br />
‣ Triple Therapy HP Eradication (3x2x1) + Maintenance w/ H2 ant for 4-6wks<br />
‣ Eradication: 3 drugs, 2 times a day, 1 week<br />
- metronidazole (flagyl) losec<br />
or + clarithromycin (biaxin) + or<br />
amoxicillin (amoxil)<br />
ranitidine-bisthmus<br />
‣<br />
‣ Maintenance: H2 antagonist for 4-6wks<br />
Surgery<br />
‣ Perforation indication for immediate laparotomy, bleeding may require<br />
surgery<br />
‣ Gastric outlet obstruction treated w/ NG tube followed by vagotomy w/<br />
drainage<br />
‣ Preventive Sx: vagotomy or gastrectomy
GASTRIC ULCERS<br />
EPIDEMIOLOGY<br />
‣ Incidence peaks in 50s (10yrs later than DU)<br />
‣ Incidence NOT decreasing<br />
‣ 3 males: 2 females<br />
‣ Less common clinically than DU<br />
‣ Increase risk of Ca (1/200): Must R/O Ca<br />
ETIOLOGY<br />
‣ 80% associated w/ HP<br />
‣ 15% associated w/ NSAIDs<br />
‣ 5% other: stress, ischemia, infections, ZES<br />
PATHOLOGY<br />
‣ Imbalance b/w protective and damaging factors<br />
‣ Interplay b/w HP, drugs, smoking, alcohol, caffeine, stress,<br />
‣ Pathophysiological Characteristics<br />
‣ Normal or reduced acid secretion rates<br />
‣ NOT associated w/ hypergastrinemia or hyperchloremia<br />
‣ Decreased parietal cell mass<br />
‣ Decreased pyloric sphincter pressure (in response to acid , secretin, fat,<br />
and CCK in duo) leading to increased duogastric reflux thus increased bile<br />
acids and pancreatic enzymes in stomach (bile + Hcl very damaging)<br />
‣ Location<br />
‣ Majority found at fundic-antral junction on lesser curvature<br />
‣ Ulcers on greater curvature and cardia are more likely to be Ca<br />
CLINICAL FEATURES<br />
‣ Pain<br />
‣ Epigastric pain is MC symptom but the pattern is less characteristic<br />
‣ Less consistent relief w/ food or antacids<br />
‣ N+V may occur in absence of gastric outlet obstruction<br />
‣ May present with complications<br />
‣ Hemorrhage<br />
‣ Gastric outlet obstruction<br />
DIAGNOSIS<br />
‣ UGI series: note that NSAID induced ulcers are often too superficial to be seen and<br />
cannot dx benign vs malignant<br />
‣ Endoscopy: must be done to R/O Ca, important to determine in HP is present<br />
TREATMENT<br />
‣ Lifestyle<br />
‣ Eradication triple therapy + Maintenance therapy<br />
‣ D/C NSAIDs
NSAID INDUCED ULCERS<br />
EPIDEMIOLOGY<br />
‣ Cause 15% of gastric ulcers<br />
‣ Cause 7% of duodenal ulcers<br />
‣ Cause gastric mucosal petechieae in virtually all, erosions in most, and ulcers in some<br />
(2% with symptomatic ulcers/complications)<br />
PATHOGENESIS<br />
‣ Local effect: non-ionized drug (HA) in stomach acid can enter gastric epithelial cell<br />
‣ Systemic effect: absorption into blood, distribution to stomach epithelial cells (note some<br />
systemic effects required for ulcer formation; reason why enteric coated can still cause<br />
ulcers)<br />
‣ Common pathway: inhibition of cyclo-oxygenase and inhibition of PG synthesis which<br />
results in decreased mucus production, decreases mucosal blood flow, decreased HCO3<br />
production, and decreased cell healing<br />
‣ Selective COX-2 inhibitors selectively block COX-2 (joints) > COX -1 (stomach)<br />
‣ Predisposing factors<br />
‣ Age<br />
‣ Previous PUD<br />
‣ High dose NSAID<br />
‣ Corticosteroid use<br />
‣ Severe medical conditions<br />
MANAGEMENT<br />
‣ D/C NSAIDs<br />
‣ Misoprostol<br />
‣ Evaluate for H. pylori<br />
‣ Acid reduction: H2 antagonist or PPI<br />
Stress Ulcerations<br />
‣ Mostly ICU patients<br />
‣ Stomach (fundus) most common<br />
‣ Usually only recognized by UGI bleeding<br />
‣ Pathogenesis?: ishcemia, hypersecretion of acid<br />
especially in CNS diseaase (“Cushing’s ulcers”)<br />
‣ Prophylaxis decreases ulcers but increases<br />
pneumonia:<br />
‣ Treatment same as for bleeding peptic ulcers<br />
Risk Factors:<br />
Mechanical ventilation, multiorgan failure, septic, severe<br />
surgery/trauma, CNS insult, burns > 35% BSA.
NONULCER DYSPEPSIA<br />
DEFINITIONS<br />
‣ Dyspepsia = a group of symptoms that suggest upper gastrointestinal tract disease.<br />
Often used to mean upper abdominal pain/discomfort but may include early satiety, postprandial<br />
bloating or distension, nausea/vomiting<br />
‣ Functional Dyspepsia (nonulcer dyspepsia) = chronic or recurrent upper abdominal pain<br />
or discomfort that is not explained by biochemical or structural abnormalities on diagnostic<br />
evaluation. Also called essential dyspepsia, idiopathic dyspepsia.<br />
EPIDEMIOLOGY<br />
‣ Prevelance of 30% for chronic dyspepsia (>1mo) and 6% for acute dyspepsia (
MEDICATION OPTIONS<br />
‣ Gastric Acid Suppressants<br />
‣ H2 antagonists and PPIs<br />
‣ Generally shown to provide little help<br />
‣ Improvement in dyspeptic symptoms w/ acid suppression has been<br />
shown to be only 25% better than placebo<br />
‣ Prokinetics<br />
‣ Metaclopramide (maxaran), Cisapride (propulsid), Domperidone<br />
‣ More effective<br />
‣ Improvement of symptoms 50% greater than placebo<br />
‣ H. pylori erradication<br />
‣ Controversial<br />
‣ Reasonable for the FP who does not have endoscopic evidence of<br />
organic disease when treating dyspepsia empirically<br />
‣ Psychotropic Medication<br />
‣ TCAs, SSRIs, anxiolytics<br />
‣ No data from controlled studies to support the use of these agents<br />
routinely<br />
‣<br />
Antinociceptive Agents<br />
‣ Low dose TCAs, kappa opiod agonists (fedotozine), Serotonin<br />
receptor antagonists (ondansetron, granisetron), SST analogs<br />
(ocreotide)<br />
‣ Role not yet determined<br />
APPROACH TO MANAGEMENT<br />
‣ Interview important to initiate symptom based dx, explore pt concerns and<br />
expectations, explore psychosocial isssues, educate, and determine if pt has a<br />
fear of Ca<br />
‣ Evidence of organic disease, Ca fear, or severe symptoms perceived by pt or Dr.<br />
‣ Endoscopy<br />
‣ Empiric Tx if nothing found<br />
‣ No evidence of organic dz, or normal investigations<br />
‣ Empiric Tx<br />
‣ Approach three subgroups
GASTRITIS<br />
ACUTE<br />
‣ Alcohol<br />
‣ NSAIDs<br />
‣ Bacteria<br />
‣ Food poisoning<br />
‣ Stress<br />
CHRONIC<br />
‣ Autoimmune - congenital pernicious anemia<br />
‣ Bacteria - HP<br />
‣ Chemical - bile relux (following Sx,EtOH)<br />
‣ Drugs - NSAIDs<br />
‣ Eosinophillic - eosinophillic gastroenterities<br />
‣ Follicular - HP<br />
‣ Granulomatous - TB, Chron’s<br />
‣ Hypertrophic - menetrier’s dz<br />
*Chronic gastritis 10Xs more likely to get gastric Ca*<br />
MANAGEMENT<br />
‣ Endoscopic diagnosis<br />
‣ Management depending on condition present<br />
SUPERIOR MESENTERIC ARTERY SYNDROME<br />
‣<br />
‣<br />
SMA crosses the duodenal segment of small intestine and leads to obstruction<br />
Pain precipitated by eating<br />
HELICOBACTER PYLORI (HP)<br />
MICROBIOLOGY<br />
‣ Gram -ve rod, spiral, flagellated, giesma +ve, urease producing<br />
‣ Source unknown but person-person spread most likely<br />
‣ most acquired in childhood<br />
‣ family spread<br />
‣ fecal-oral spread most likely<br />
‣ Risk factors for infection are mainly low SES and age<br />
‣ Prevalence increase w/ age (1% per year of life when >30yo); plateaus at approximately<br />
40 -50% at > 50yo<br />
‣ Multiple genotypes w/ virulent strains causing ulcer disease. This explains why not all<br />
individuals w/ the HP infection get ulcer disease<br />
‣ Only 15% of infected b/c symptomatic (all have gastritis, 15% develop PUD)<br />
‣ Lives in mucus layer<br />
‣ a few adhere to mucosa but DO NOT penetrate mucosa
‣<br />
urease splits urea and produces ammonia which neutralizes the acid<br />
H.PYLORIA AND HUMAN DISEASE<br />
‣ Definite Associations ......<br />
‣ Gastritis: all HP infected patients have gastritis which resolves w/ HP<br />
eradication<br />
‣ Gastric Ulcers: 90% of nonmalignant, nonNSAID ulcers are associated w/<br />
HP; eradication prevents recurrence; nearly 100% recurrence w/o<br />
eradication<br />
‣ Duodenal Ulcers: 95% of nonNSAID ulcers are associated w/ HP,<br />
eradication reduces recurrence to zero; failure of eradication leasds to<br />
100% recurrence<br />
‣ Possible Associations ......<br />
‣ Nonulcer dyspepsia<br />
‣ NSAID induced gastropathy<br />
‣ MALT (Mucosal Associated Lymphoid Tissue) lymphoma<br />
‣ Gastric Adenocarcinoma: increase risk 9Xs<br />
‣ Nonassociated Conditions<br />
‣ GERD<br />
‣ Irritable bowel syndrome<br />
‣ Cholecystitis<br />
DIAGNOSIS<br />
‣ Biopsy histology: gold standard<br />
‣ Biopsy urease gel: rapid, less expensive<br />
‣ Urea breath test: inexpensive, doesn’t detect ulcer, should not be used for initial dx,<br />
reserved for confirmation of eradication<br />
‣ Serology: inexpensive, test of choice when endoscopy not needed, remains +ve awhile :.<br />
cannot be used to confirm eradication, false -ves: Abx, bismuth compounds, PPIs w/i last<br />
month<br />
WHO SHOULD BE TESTED?<br />
‣ Radiologically/Endosopically confirmed gastric or duodenal ulcer —> NO testing<br />
necessary b/c it is assumed that HP is present and eradication is indicated w/o testing<br />
‣ Confirmation of eradication is generally not necessary<br />
‣ Confirm eradication w/ urea breath test @ 4 - 8 wks following eradication therapy if high<br />
risk (ex: previous ulcer complications or multiple medical problems)<br />
ERADICATION WITH TRIPLE THERAPY<br />
‣ Amoxicillin (1gm bid) X 7d<br />
‣ Clarithromycin (500mg bid) X7d **3 drugs, 2 times a day, for 1 week**<br />
‣ Omeprazole (30mg bid) X 7d<br />
‣ Who should be treated?<br />
(1) Recommended .....<br />
‣ nonmalignant, nonNSAID gastric/duodenal ulcer<br />
confirmed by radiology or endoscopy<br />
(2) Recommended by some .....<br />
‣ nonulcer dyspepsia (ulcer - like subgroup)<br />
‣ strong fhx of gastric cancer
‣ NSAID therapy<br />
‣ following surgery for PUD<br />
(3) Not Recommended ....<br />
‣ asymptomatic pts<br />
HP & PUD<br />
‣ 90% of DU have antral bx w/ HP +ve<br />
‣ 80% of GU have antral bx w/ HP +ve<br />
‣ 90% of gastritis have HP<br />
‣ 100% of chronic active gastritis have HP<br />
‣ Relapse common in HP not eradicated<br />
‣ 0 - 4% per year recurrence if HP eradicated<br />
‣ 40 - 80% per year recurrence if HP NOT eradicated<br />
‣ MOA<br />
‣ antral gastritis ------ decrease ST and increase gastrin ------<br />
increased gastric acid secretion ------- duo metaplasia -------<br />
colonation by HP in duodenum ----- duodenal bulb inflammation -----<br />
duodenitis ----- DU