26: MULTIPLE TRAUMA PATIENT - rEMERGs
26: MULTIPLE TRAUMA PATIENT - rEMERGs
26: MULTIPLE TRAUMA PATIENT - rEMERGs
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>26</strong>: <strong>MULTIPLE</strong> <strong>TRAUMA</strong> <strong>PATIENT</strong><br />
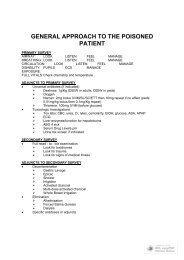
PREPARE<br />
Room and equipment<br />
Staff<br />
Discuss case/interventions<br />
Paramedic report<br />
PRIMARY SURVEY (Assessment and Management)<br />
<br />
<br />
<br />
<br />
<br />
<br />
Airway<br />
Breathing<br />
Circulation<br />
Disability<br />
Exposure<br />
Full vitals<br />
ADJUNCTS TO PRIMARY SURVEY<br />
Pulsox, cardiac monitors, BP monitor, CO2 monitor<br />
NG tube<br />
Foley<br />
ECG<br />
Xrays: Cspine, CXR, pelvis<br />
Trauma blood work<br />
ABG<br />
DPL/ABUS if appropriate<br />
SECONDARY SURVEY<br />
AMPLE history<br />
H/N<br />
Chest<br />
Abd<br />
U/G<br />
Neuro<br />
Msk<br />
Roll pt<br />
ADJUNCTS TO SECONDARY SURVEY<br />
Xrays<br />
CT head, chest, pelvis, abd, spine<br />
ABUS<br />
DPL<br />
Contrast studies<br />
Endoscopy<br />
Angiography<br />
Esophagoscopy<br />
Bronchoscopy
PRIMARY SURVEY<br />
Airway and C-spine<br />
‣ LOOK<br />
<br />
<br />
<br />
<br />
<br />
‣<br />
‣<br />
‣<br />
level of consciousness, agitated, cyanosis, retractions, AMU,<br />
evidence of facial or laryngeal injury, evidence of UAW burn<br />
(carbenaceous sputum, singed hairs, soot around mouth)<br />
LISTEN<br />
speech clear, stridor, gurgling, hoarseness<br />
FEEL<br />
maxillofacial trauma, laryngeal trauma, trachea midline, crepitus,<br />
subcutaneous emphysema<br />
MANAGE<br />
manage airway while maintaining C-spine control<br />
hierarchy: jaw thrust, oropharyngeal airway, nasopharyngeal<br />
airway, nasotracheal intubation, endotracheal intubation, jet<br />
insufflation, cricothyroidotomy; clear foreign bd and suction<br />
Breathing and Ventilation<br />
‣ LOOK<br />
RR, depth of respirations, chest wall mvmts, chest wall injuries<br />
‣ LISTEN<br />
breath sounds, heart sounds, bowel sounds in chest<br />
‣ FEEL<br />
subcutaneous emphysema, trachea midline, dull or tympanic to<br />
percussion, chest wall injury, look for internal bleeding<br />
‣ MANAGE<br />
100% 02: face mask with NRB at 10 - 12 L/min<br />
pulsoximeter, end tidal C02<br />
ventilation by BVM or ETT as necessary<br />
thoracentesis for pneumo, chest tube for hemo/pneumo, seal<br />
open chest wounds<br />
Circulation and Hemorrhage<br />
‣ LOOK<br />
identify external bleeding, skin color, diaphoresis, JVD<br />
‣ LISTEN<br />
muffled heart sounds, murmur<br />
‣ FEEL<br />
pulse rate, pulse quality, BP, cool/clammy skin<br />
quick feel of abdomen and pelvis to identify major hemorrhage<br />
‣ MANAGE<br />
cardiac monitor, BP monitor<br />
two large bore IVs, send blood for trauma panel and ABG<br />
bolus 2L RL for hypotension<br />
direct pressure to bleeding sites; no clamps unless direct<br />
visulualzn<br />
consider yourself STUCK on C if hypotensive; give initial tx and<br />
rember to return to see response and look for cause<br />
consider need for DPL or ABUS in primary survey if hypotensive<br />
Disability<br />
‣ PUPILS<br />
‣ GCS<br />
‣ Manage: RSI intubation, hyperventilation, mannitol for impending herniation<br />
Exposure/Environment<br />
‣ Full exposure and prevent hypothermia<br />
Full Vitals<br />
‣ Repeat vitals including core temp; are you stuck on primary survey b/c of poor
vitals??<br />
ADJUNCTS TO PRIMARY SURVEY<br />
Most should already be done<br />
Monitors: Pulsox, BP and cardiac monitor, ET CO2 monitor<br />
Xrays: C-spine, CXR, and pelvic Xrays (TRY to get CXR and pelvis early; C-spine can<br />
wait until secondary survey)<br />
DPL, ABUS<br />
NG and urinary tubes if not contraindicated (foley after rectal)<br />
SECONDARY SURVEY<br />
AMPLE history and details of accident including condition of vehicle, ejection, other<br />
injured passengers, seat belts, blood loss at seen, vitals on route, interventions on route,<br />
etc<br />
Head and Neck<br />
‣ Head: lacerations, contusions, fractures, burns<br />
‣ Face: maxillofacial fractures, racoon eyes, battle signs, look in mouth,<br />
burns, carbenaceous sputum, soot, singed hairs, nose for CSF leak<br />
‣ Eyes: pupil size and reactivity, EOM, visual acuity, hemorrhage, racoon<br />
eyes<br />
‣ Ears: battle signs, hemotympanum, CSF leak<br />
‣ Cranial nerves: II - XII if not already tested; occulocephalics and<br />
occulovestibular reflexes, corneal reflex, gag reflex<br />
‣ Neck: inspect for blunt injury, penetrating injury, tracheal deviation,<br />
accessory muscle use; palpate for deformity, tenderness, swelling, subQ<br />
emphysema, tracheal deviation, symmetry of pulses; listen to carotids,<br />
palpate C-spine.<br />
Chest<br />
‣ Look: blunt or penetrating trauma, acc muscle use, chest expansion, JVD<br />
‣ Listen: breath sounds and heart sounds<br />
‣ Feel: tenderness (AP and lateral compression), rib tenderness,<br />
crepitation, subcutaneous emphysema, percuss for hyperresonance or<br />
dullness<br />
Abdomen<br />
‣ Look: blunt or penetrating trauma (look closely at sides re hepatic and<br />
splenic injury may be suspected by lower rib cage lateral abrasion)<br />
‣ Listen: bowel sounds<br />
‣ Feel: palpate for tenderness, guarding, rebound; percuss for tenderness<br />
‣ DPL, ABUS, ABCT, pelvic Xrays as appropriate<br />
Urogenital<br />
‣ Look: contusions, lacerations, urethral/vaginal/rectal bleeding<br />
‣ Rectal: prostate position, bone fragments, wall integrity, sphincter tone,<br />
blood<br />
‣ Vaginal: laceration, blood, bone fragments<br />
MSK<br />
‣ Look, feel, move all joints of upper and lower limb looking for lacerations,<br />
contusions, deformities, crepitus, possible fractures<br />
‣ Compress pelvis AP and lateral<br />
‣ Assess limb pulses and neuro status distal to suspected fractures<br />
‣ Obtain Xrays of injured parts<br />
Neuro<br />
‣ Mental status and GCS
‣<br />
‣<br />
Roll Pt<br />
‣<br />
Cranial nerves<br />
Strength, Reflexes, Sensation, Coordination<br />
Look, feel for any injuries, lacerations, contusions, spine tenderness,<br />
rectal<br />
<strong>MULTIPLE</strong> <strong>TRAUMA</strong> CONCEPTS<br />
EPIDEMIOLOGY/INTRO<br />
MCC of death < 40 yo; #1 cause of PYLL<br />
Huge economic costs and chronic dz and societal loss<br />
MOST/ALL preventable<br />
MOI very important<br />
MOI and suspected injury patterns: table <strong>26</strong>-1<br />
TRIAGE<br />
Multiple casualties = the number and severity of the injuries do NOT exceed the ability of<br />
the facility to render care. Treat life-threatening injuries first.<br />
Mass casualties = the number and severity of the injuries EXCEED the capability of the<br />
facility and staff. Those w/ the greatest chance of survival, with the least expenditure of<br />
time, equipment, supplies, and personnel are managed first.<br />
<strong>TRAUMA</strong> SYSTEM<br />
Trauma centers<br />
ATLS approach<br />
Prehospital system<br />
Triage scheme (Box <strong>26</strong>-1)<br />
Quality assurance programs<br />
Trauma logs and review: M&M rounds<br />
Trauma scoring system<br />
CLINICAL MANAGEMENT KEYS<br />
Prehospital<br />
‣<br />
<br />
ED phase<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
Prevent additional injury, rapid transport, advanced notification,<br />
appropriate triage, initial tx<br />
Organized team approach with TTL doing initial assessment, coordinating<br />
procedures and investigations<br />
High priority Mx: ABC and impending herniation<br />
Low priority Mx: neuro, cardiac, abdomenal, msk, SCI, burns<br />
Treat before diagnosis in critically ill<br />
Thorough physical examination for injuries<br />
Frequent reassessment<br />
Monitoring vitals, ins/outs, serial Hb/lactate, CVP and Swan Ganz, art line
PITFALLS/KEY POINTS<br />
PRIMARY SURVEY<br />
AIRWAY + C-SPINE CONTROL PITFALLS<br />
‣ Equipment failure<br />
‣ Pt cannot be intubated a/f RSI and paralysis<br />
‣ Surgical AW cannot be performed b/c of obesity<br />
‣ Intubation of pt w/ unknown laryngeal fractureor incomplete UAW<br />
obstruction may ppt total AW obstrstruction<br />
‣ Indications for intubation: AWO real or impending, ventilation, inc ICP<br />
‣ C - spine not big concern with penetrating trauma<br />
‣ RSI with oral intubation is preferred route of AW mx<br />
BREATHING AND VENTILATION PITFALLS<br />
‣ Profound SOB and cyanosis may suggest airway problem but may be<br />
ventilation problem (ie; pneumothorax)<br />
‣ Intubation of the unconscious may produce a pneumo<br />
CIRCULATION PITFALLS<br />
‣ Elderly can have diminished tacchycardic response to hypovolemia :. they<br />
are hypovolemic and you don’t suspect it. Must suspect hypovolemia<br />
even in absence of tacchycardia. BP has little correlation w/ cardiac<br />
output in elderly.<br />
‣ Children have excellent physiological reserve :. CRASH very quickly a/f<br />
having previously normal vitals<br />
‣ Athletes have unusally low heart rates<br />
‣ Central line or cut down necc. for difficult access<br />
‣ If hypotensive, look for source in primary survey (Chest, abdomen, pelvis)<br />
DISABILITY PITFALLS<br />
‣ Rapid deterioration in neurological status is imp<br />
‣ Lucid interval commonly associated w/ epidural hematoma is an example<br />
of how the pt can “ talk and die” .<br />
‣ Reassesment is critical<br />
EXPOSURE PITFALLS<br />
‣ Early control of hemorrhage to prevent req’t for massive fluids/blood which<br />
induce hypothermia<br />
FULL VITALS<br />
‣ Failure to repeat vitals<br />
‣ Failure to take core temperature<br />
‣ Failure to focus on primary survey: do not move on to secondary<br />
survey until happy with primary survey; or do quick secondary looking<br />
for etiology of primary survey problem<br />
ADJUNCTS TO THE PRIMARY SURVEY<br />
ECG monitoring<br />
‣ Essential in all trauma pts
‣<br />
‣<br />
‣<br />
Blunt cardiac injury: tachycardia, Afib, PVCs, ST changes<br />
PEA: cardiac tamponade, tension pneumo, profound hypovolemia<br />
Hypoxia, hypovolemia: bradycardia, abereant conduction, premature<br />
beats<br />
<br />
<br />
<br />
<br />
Foley Catheter<br />
‣ Monitor fluid status<br />
‣ Must not put in b/f genital and rectal examination<br />
‣ Contraindicated if urethral transection suspected.......<br />
(1) penile meatus blood<br />
(2) perineal echymosis<br />
(3) blood in scrotum<br />
(4) high-riding or nonpalpable prostate<br />
(5) pelvic fracture<br />
Gastric Catheters<br />
‣ Reduce stomach distension and decrease (NOT prevent) the risk<br />
of aspiration<br />
‣ May induce vomiting; must have suction ready<br />
‣ MUST be placed orally if cribriform plate fracture is suspected<br />
Monitoring<br />
‣ Ventilatory rate and ABGs: colorimetric carbon dioxide detector<br />
confirms that the ETT is in the airway but DOES NOT confirm<br />
proper placement<br />
‣ Pulse oximetry: do not place distal to the BP cuff.<br />
‣ BP monitor: can be placed on leg if arms are burned<br />
Xrays<br />
‣ Must do even in the pregnant pt<br />
<strong>TRAUMA</strong> ARREST<br />
Combination of ATLS and ACLS<br />
CPR inneffective b/c either exsanguination or tamponade<br />
Epinephrine ineffective<br />
Thoracotomy<br />
‣ Indicated in penetrating trauma unless dead at scene<br />
‣ NOT indicated in blunt (may consider with loss of vitals in ED)<br />
PEA in trauma pt<br />
‣ ABCs: hypoxia<br />
‣ Fluids: hypovolemia<br />
‣ Needles<br />
Bilateral tension pthrx decompression<br />
Pericardiocentesis decompression: debatable in<br />
trauma setting b/c basically useless