ANTICONVULSANTS PHENYTOIN - rEMERGs
ANTICONVULSANTS PHENYTOIN - rEMERGs
ANTICONVULSANTS PHENYTOIN - rEMERGs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>ANTICONVULSANTS</strong><br />
GENERAL<br />
Relatively common overdoses<br />
Valproic acid and other newer anticonvulsants becoming more common<br />
Most common are valproic acid, carbemazepine, phenytoin<br />
Four groups of mechanisms of action: some have multiple MOAs (see figure 21-1)<br />
‣ Na channel blockers: phenytoin, carbemazepine, valproic acid, etc<br />
‣ GABA effects/agonism: gabapentin, valproic acid<br />
‣ Glutamate antagonism: lamotrigine<br />
‣ Calcium channel blockade: lamotrigine<br />
<strong>PHENYTOIN</strong><br />
INTRODUCTION<br />
NO role in treatment of most toxic seizures<br />
NO role in alcohol withdrawl seizures (GABA related thus Na+ channel blockade doesn’t help)<br />
Non sedating in therapeutic doses thus preferred initial agent for long term seizure control<br />
PHARMACOLOGY<br />
Highly protein bound to albumin: only unbound drug can exert action<br />
Rapidly distributed into tissues<br />
Absorption is slow (8+hrs)<br />
May for concretions in GI tract<br />
Metabolized in liver by P450 system<br />
Therapeutic range = 40 - 79 umol/L<br />
Pharmacokinetics<br />
‣ Low dose: first order thus elimination increases as drug increases<br />
‣ Higher dose: zero order thus elimination is constant despite increasing drug<br />
(reason by can become toxic if dose is advanced to fast); becomes zero order once<br />
enzymes become saturated<br />
‣ Elimination T ½ is 6-24 hours with first order kinetics<br />
‣ Elimination T ½ is 20-60 hours with zero order kinetics<br />
Adverse Effects of Therapeutic dosing<br />
‣ CNS: nystagmus, ataxia, dizziness, diplopia, drowsiness, involuntary movements<br />
‣ Involuntary movements are similar to dyskinesias with anitpsychotics<br />
‣ Gingival hyperplasia: dose related, > 40%, decreased with oral hygeine<br />
‣ Dysmorphic changes of nose, lips, brows<br />
‣ Peripheral neuropathy<br />
‣ Acne, alopecia, hirsutism<br />
‣ Megaloblastic anemia<br />
‣ Leukopenia, thrombocytopenia, aplastic anemia<br />
CLINICAL MANIFESTATIONS<br />
Neurologic Manifestations
Other<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
‣<br />
Phenytoin > 60 umol/L: nystagmus<br />
Phenytoin > 120: ataxia<br />
Phenytoin > 200: lethargy, slurred speech, movement disorders<br />
Can be toxic at lower levels with low albumin (more free drug)<br />
Seizures can occur but are VERY rare<br />
Choreas and opisthotonic movements more common in children and elderly<br />
No cardiotoxicity reported from oral doses<br />
IV doses has caused hypotension (propylene glycol), negative inotropy, decreases<br />
SVR all leading to hypotension<br />
Extravasation can cause tissue necrosis<br />
Increased toxicity in low albumin, neonates, elderly, as well as certain coingestants<br />
(salicylates, vlaproate, sulfonamides)<br />
<br />
Diagnostic Testing<br />
‣ Total phenytoin level measures bound and unbound drug: conversion factor for<br />
albumin level required<br />
‣ Conversion<br />
Phenytoin = measured/(0.25 X measured) + 0.1<br />
MANAGEMENT<br />
Supportive care is the mainstay<br />
Activated charcoal (caution in seizure d/o patients as may ppt seizure)<br />
MDAC if levels increasing or persistently elevated<br />
Serial examinations for resolution of ataxias<br />
NO routine cardiac monitoring required<br />
Follow serial levels as absorption unpredictable and may be delayed<br />
Dyskinesis during therapeutic administration usually self limited and resolve after few hours<br />
Hemodialysis of little benefit b/c highly protein bound<br />
No specific antidotal therapy<br />
CARBEMAZEPINE<br />
INTRODUCTION<br />
Tegretol<br />
Structurally similar to TCAs (think of TCA of anticonvulsants!!)<br />
Only available for oral use<br />
Considered best anticonvulsant by many<br />
PHARMACOLOGY<br />
MOA: Na channel block<br />
Lipophilic, slow absorption<br />
Levels may not peak for 24hrs after acute ingestion<br />
Some anticholinergic properties; delays ingestion even further<br />
There is not a simple relationship between dose and levels<br />
Metabolized by P450 system
First order kinetics and doses often have to be increased<br />
Elimination T ½ is 10-20 hours<br />
Therapeutic level = 17 - 51 umol/L<br />
Adverse effects of Therapeutic dosing<br />
‣ Irritability, impaired cognition/memory<br />
‣ Rashes, Steven’s-Johnson<br />
‣ Hepatitis<br />
‣ Drug induced SLE<br />
‣ Leukopenia, aplastic anemia<br />
‣ Anticonvulsant hypersensitivity syndrome<br />
CLINICAL MANIFESTATIONS<br />
Neurologic<br />
‣ Nystagmus, ataxia, dysarthria<br />
‣ Lethargy, coma with large ingestions<br />
‣ Seizures more common than dilantin od: increased seizure frequency may be only<br />
presenting feature of carbamezepine chronic toxicity<br />
‣ Can have status epilepticus<br />
‣ Peds: dystonic reactions, choreoathetosis, seizures<br />
Cardiovascular<br />
‣ Tachycardia: anticholinergic effect<br />
‣ Hypotension: myocardial inhibition<br />
‣ Wide QRS and prolonged QT<br />
15% of acute ingestions have QRS > 100 msec<br />
50% of acute ingestions have QT > 420 msec<br />
Can also occur with chronic ingestions<br />
May present delayed (absorption can be delayed)<br />
Terminal 40 msec right axis not documented in literature<br />
Chronic Overdoses<br />
‣ Seizures, headaches, ataxia, diplopia, SIADH<br />
<br />
Diagnostic Testing<br />
‣ Measure carbemazepine levels<br />
‣ Levels need to be repeated as absorption is highly variable and may be delayed<br />
‣ Therapeutic levels 17-51 umol/L<br />
‣ Levels > 120: coma, seizures, resp depression, cardiotoxicity<br />
‣ Can be toxic with levels in therapeutic range as there are ACTIVE<br />
METABOLITES (especially if combination therapy with valproate, etc)<br />
MANAGEMENT<br />
Activated charcoal<br />
MDAC is indicated and helpful as there is prominent enterohepatic circulation<br />
Delayed rise in levels can reflect concretions<br />
Hemodialysis ineffective<br />
Cardiac Toxicity<br />
‣ Cardiac monitoring required<br />
‣ Sodium Bicarb for QRS > 100 msec (not studied): as per TCAs
VALPROIC ACID<br />
INTRODUCTION<br />
Valproate, Epival, Depakene, Depacon,Depakote<br />
Di-n-propylacetic acid<br />
Uses: seizures, bipolar, migraines<br />
SR preparations are very common<br />
Common presentation of mild symptoms, discharged after few hours, delayed<br />
absorption and later crashes with decreased LOC 6-12hrs later due to delayed<br />
absorption (consider WBI)<br />
PHARMACOLOGY<br />
MOA: GABAergic effect (decreases degredation of GABA), some Na+ channel effects<br />
Therapuetic levels = 347 - 833 umol/L<br />
Complex metabolism in liver<br />
Valproic acid metabolism is dependant on carnitine as a cofactor (see 41-2 in goldfranks)<br />
‣ Complicated interaction with carnitine<br />
‣ Valproate DECREASES carnitine stores through various mechanisms<br />
‣ Carnitine depletion or deficiency decreases metabolism of valproic acid<br />
‣ Carnitine depletion has other metabolic effects: impaired transport of fatty acids,<br />
inhibition of ketoacid oxidation, and inhibition of the urea cycle resulting in an<br />
increased ammonia<br />
‣ Valproate therapeutic or overdose setting<br />
DECREASED CARNITINE<br />
INCREASED AMMONIA<br />
Adverse effects of Therapeutic dosing<br />
‣ Elevated liver enzymes<br />
‣ Toxic hepatitis --------> can be fatal<br />
‣ Reye’s syndrome<br />
‣ Hyperammonia<br />
‣ Carnitine deficiency<br />
CLINICAL MANIFESTATIONS<br />
Most are benign<br />
Hallmarks = COMA and RESPIRATORY DEPRESSION<br />
Neurologic<br />
‣ Decreased LOC<br />
‣ Ataxia, nystagmus, dyarthria do NOT occur<br />
Other<br />
‣ Increased Ammonia: 40% of those on chronic therapy, may occur after acute<br />
ingestion also, levels > 60 umol/L<br />
‣ Decreased Carnitine<br />
‣ Metabolic acidosis: secondary to lactate, can be severe, poor prognostic sign<br />
‣ Leukopenia, anemia, thrombocytopenia<br />
‣ Renal failure<br />
‣ Hepatotoxicity
Diagnostic Testing<br />
‣ Valproic acid levels<br />
‣ Repeat 2-3 hours and monitor closely<br />
‣ Carnitine and ammonia levels<br />
MANAGEMENT<br />
Supportive is mainstay<br />
Activated charcoal<br />
MDAC for large ingestions and rising levels<br />
Whole bowel irrigation for SR preps<br />
Dialysis may have a role<br />
Narcan<br />
‣ Case reports of increased LOC with narcan<br />
‣ Other reports show no effect<br />
‣ Not dangerous but unlikely to make much difference<br />
‣ ? mechanism related to GABA<br />
Carnitine<br />
‣ Role not well defined<br />
‣ No controlled studies<br />
‣ Pediatric neurology society recommends that all children on valproic acid should<br />
have prophylactic carnitine supplementation<br />
‣ Others recommend carnitine supplementation only for those children who have<br />
acutely ingested > 400 mg/kg<br />
‣ Unclear if carnitine will DECREASE HEPATOTOXICITY incidence<br />
‣ Generally, carnitine prophylaxsis is indicated for < 2yo, malnurished, other<br />
anticonvulsants, ketogenic diets<br />
‣ Role in acute ingestion undefined<br />
‣ Carnitine = 100mg/kg/d divided into 3 doses orally<br />
Dialysis<br />
‣ Rapid clinical deterioration<br />
‣ Hepatic failure<br />
‣ Rising levels despite MDAC or WBI<br />
‣ Serum levels > 1000 mg/L (? SI units)<br />
OTHER <strong>ANTICONVULSANTS</strong><br />
GABAPENTIN<br />
Sedation, ataxia, slurred speech<br />
No major toxicities or deaths reported<br />
Supportive care<br />
Activated charcoal<br />
No dialysis<br />
No specific antidote
LAMOTRIGINE<br />
Sedation, ataxia, nystagmus, slurred speech, seizures<br />
ECG abnormalities: QRS prolongation has been seen (uncommon)<br />
Supportive care<br />
Activated charcoal<br />
ECG monitoring<br />
Bicarb for wide QRS (unproven)<br />
Benzodiazepines for seizures<br />
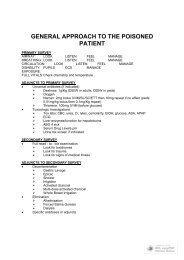
PRESENTATION LEVELS MANAGEMENT<br />
<strong>PHENYTOIN</strong><br />
Nystagmus<br />
Ataxia<br />
Movement disorders<br />
Seizures RARE<br />
40 - 79 umol/L<br />
check albumin level<br />
Supportive<br />
Activated charcoal<br />
CARBEMAZEPINE<br />
Nystagmus<br />
Ataxia<br />
Seizures COMMON<br />
WIDE QRS<br />
WIDE QT<br />
17 - 51 umol/L Cardiac monitoring<br />
MDAC<br />
BICARB<br />
VALPROIC ACID<br />
Coma<br />
Respiratory depression<br />
NO ataxia seizures<br />
347-833 umol/L<br />
Carnitine decreased<br />
Ammonia increased<br />
MDAC<br />
WBI for SR prep<br />
Carnitine<br />
Narcan<br />
Dialysis